Effective Strategies for Managing Substance Use Disorders in Older Adults in Nursing Homes
© 2024 Pavani Kottapalli, Ranjith Kumar Beluri Talari, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Substance use disorder is very prevalent in nursing home (NH) residents due to aging, the number of prescription drugs that are being used to manage their physical and psychological pain, and several discharges with the diagnosis of substance use disorder from hospitals to NH for aftercare support. However, many nursing homes are not equipped to provide adequate care for residents with a diagnosis of substance use. The staff is not well-trained to care for this type of population, which is becoming a challenge for the staff to manage residents in-house, leading to overdose, recurrent hospitalization, and unsuccessful discharges to communities due to relapses and an increase in the number of frequent flyers. Substance use disorder has become a significant public health concern in the United States, especially in the older population from the past couple of decades, which tends to increase. Discharging older adults with substance use disorders into nursing homes without ensuring established resources in the long-term care setting raises safety and quality concerns, emphasizing a pressing need for innovative preventive and management approaches for substance use disorders to meet unique needs of older adults in nursing homes.
Purpose: The purpose of the study is to explore and identify the interventions, treatments and care models to effectively manage substance use disorders in older residents who are living in nursing homes. The study further focuses on the unique challenges that are faced by older adults and staff in nursing homes to understand the need for integrating addiction treatments in Long-term care settings to assess the need to enhance care strategies to improve resident outcomes, which includes handling overdose emergencies, prevention, rehabilitation and relapse management of substance use disorders (SUDs).
Scope: Provides valuable insights for future researchers and points out the need for collaborative models among the rehabilitation, addiction centers, and LTC and the need for virtual health platforms to improve access to care, interdisciplinary approaches, and policy innovation on resident retention and optimum resource allocation to reduce the health care cost of frequent flyers or unnecessary hospitalizations, therefore, improve patient outcomes.
Introduction
Substance Use Disorders (SUDs) are a drastically growing and escalating global public health concern that is imposing a strain on society. It was estimated that 31 million people around the globe are diagnosed with Substance abuse disorders, and 275 million people use illegal substances [1]. Substances such as alcohol, tobacco, opioid usage, and other drugs increase the risk of injuries, diseases, increased emergency visits, and mortality rates in the population that consumes them [2].
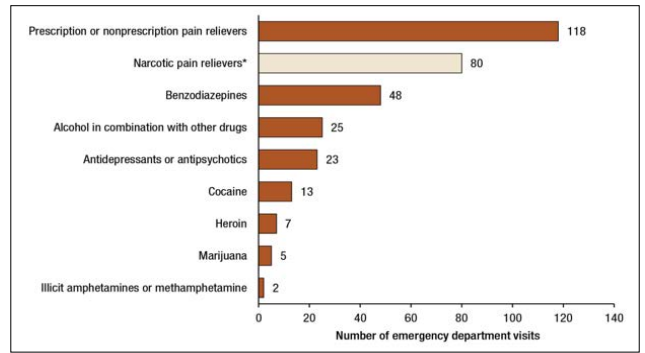
Figure 1: A day in the Life of Older Adults: Substance Use Facts [3].
Additionally, SUDs turn into chronic disease conditions and cause long-lasting changes in the brain, which leads to mental health issues and social consequences [4]. While the changes in the brain can be reversed with abstinence from substance usage, it depends on the individual’s support systems to care for SUDs, as many of the care systems rely on acute care models or episodic care for SUD rather than adopting more effective chronic care models [4]. Compounding this issue, the rapid rise of substance use disorder and opioid use disorders in older adults in nursing homes leaves the facilities without adequate resources as nursing home traditional treatment models do not allow the staff to care effectively for the vulnerable population.
It was estimated that in 2018, a total of 125,000 older population admitted to hospitals due to opioid usage and other substance use disorders in the United States [5]. Also, the recurring nature and rapid growth in the SUD/OUD (Opioid Usage Disorder) have become a burden in various sectors, which include substance- use violence and criminal activities, leading to high judicial and legal expenditure and further costing the healthcare system by increasing the need for rehabilitative services and decreasing human productivity, resulting in economic costs [6].
Further, the Medicare beneficiary analysis report reveals that in 2020, seven million older population diagnosed with opioid use disorders were discharged from hospitals to nursing homes, where Nursing Home (NH) facilities are required to manage and provide care for the growing population, presenting multifaceted challenges in addressing addiction treatment and other complex care needs [5]. Therefore, it is imperative to empower nursing home staff with adequate training to provide optimum care for older adults with SUD/OUD in NH.
Strategies for Managing Substance Use Disorders in Older Adults Initially, substance use disorders are considered chronic and high risk for relapsing; therefore, significant support and adequate efforts to be put in to provide close guidance from the beginning through each stage of the treatment is imperative to further motivate and counsel the candidates with lived experiences through recovery which would lead to the success [7]. Therefore, active staff participation in engaging the residents through each step of recovery and having non-judgmental attitudes towards residents with diagnoses of substance use disorders allow the older adults to be successful through their long-term treatment.
Also, the growing body of research reveals that the barriers to admission for SUD/OUD at nursing homes are very evident that the nursing homes use risk-aversion strategies (behavioral contracts and community pass restrictions) that are not similar across the nursing home industry due to the lack of clear guidance on the admission process. Subsequently, besides knowing that it is discriminatory under Disability Act, Nursing homes are hesitant to admit older adults with substance use disorder diagnosis due to the complexity and involved risk leading to barriers in care accessibility [5]. Furthermore, the lack of active referral process and follow-up support through the substance use disorders recovery steps, minimal to no counseling or group therapy support, and not providing the required information for the cases that left Against medical advice also led to care inaccessibility, which requires the staff to improve the skill set in areas of communication. Also, enhancing the networking strategies with addiction specialty clinics in long-term care to refer the residents who need aftercare support would help older adults with the SDU/OUD’s [7]. Consequently, the studies suggest to the staff that peer recovery support systems for long-term continuity care or chronic care models for older adults with substance use [7].
Additionally, the research has suggested that anti-stigma interventions involving the subject matter expertise in staff education, such as addiction prevention physicians’ researchers to educate on neurobiology, neurotransmitter pathways, addiction trajectories, and lived experiences of addiction recovery has changed the staff perspectives towards substance disorders and enhanced their ability towards therapeutic communication, therefore the harm reduction strategies, which is a highly suggested strategy for Long-Term care settings [1].
Likewise, an integrated health and substance use treatment system needs an addiction specialist, psychiatrist, specialty nurses, peer recovery coaches, and multiple other members. However, nursing homes lack appropriate multidisciplinary team members. There are only a few licensed members who can bill for their services under Medicare and Medicaid reimbursement, where the care aspect is limited in integration [8]. Therefore, the Nursing homes that are open to accepting older adults with substance use disorders must include addiction specialists and peer recovery coaches in their teams and train the nursing home staff to educate on robust documentation to meet the reimbursement standards further also the barriers that are existed in the reimbursement system, must be amended to improve the access for care.
Further, staff must be trained to use electronic and digital health integration models and enhance monitoring skills such as understanding the withdrawal symptoms and differentiating them from possible delirium (such as delirium vs delirium tremens) in older adults [8]. Also, staff must be trained to build positive attitudes towards SUDs to build trust with the residents to establish therapeutic relationships [8].
Further, training the staff on emergency management of overdose and withdrawal and how to take advantage of evidence-based, team-based, and integrated care models to improve the outcomes of older adults with the diagnosis of substance use disorders along with patient-centered strategies in place would help improve the quality of care and reduce the unnecessary cost of rehospitalizations. Meanwhile, training the staff on standard medication reconciliation strategies during the care transitions and the right-weaning strategies to avoid higher tendencies of opioid usage after discharge from facilities also allows the staff to prevent SUDs [5]. Finally, Opioid Usage Disorders (OUD) must be enrolled in Medication-Assisted Treatment (MAT) such as methadone, buprenorphine, and naloxone treatments to avoid withdrawals and improve sobriety before the care transition. Care facilities must be able to accept the residents without hesitance to manage residents on MAT and bill the services, as MAT is more effective than placebo effects [9]. Therefore, Medicare and Medicaid agencies must take initiatives with guidance on reimbursement, long-term care admission, and care compliance regulations [10].
Conclusion
In conclusion, although there are some advancing initiatives in combating substance use disorders in the United States and around the globe, there are many aspects that need to be improved for care accessibility and patient outcomes, such as reimbursement and networking strategies, to connect the fragmented health systems. Integrating substance use disorders courses in clinical and healthcare programs curricula also prepares clinicians and healthcare professionals to bring better patient outcomes. Further, system corrections prevent the misusage of prescriptions, which administrators, researchers, and policymakers are required to address in substance use disorders and reduce the cost to society while improving the quality.
References
- Dion K, Griggs S (2020) Teaching Those Who Care How to Care for a Person with Substance Use Nurse Educ 45: 321-325.
- Mitchell AM, Mahmoud KF, Finnell D, Savage CL, Weber M, et (2020) The Essentials Competencies: A Framework for Substance Use-Related Curricula. Nurse Educ 45: 225-228.
- Berks-Lancaster-Lebanon LINK. (2017) A day in the life of older adults: Substance use facts. Available at: https://org/2017/05/18/a-day-in-the-life-of-olderadults-substance-use-facts-samhsa/.
- Volkow ND, Blanco C (2023) substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. journal of the World Psychiatric Association 22: 203-229.
- Yang M, Beiting KJ, Levine S (2023) Barriers to Care for Nursing Home Residents with Substance Use Disorders: A Qualitative Study. Journal of addiction medicine 17: 155-162.
- Lo TW, Yeung JWK, Tam CHL (2020) Substance Abuse and Public Health: A Multilevel Perspective and Multiple Responses. Int J Environ Res Public Health 17: 2610.
- Stanojlovic M, Davidson L (2021) Targeting the Barriers in the Substance Use Disorder Continuum of Care with Peer Recovery Substance Abuse: Research and Treatment 15: 1-10.
- Substance Abuse and Mental Health Services Administration (US), Office of the Surgeon General (US) (2016) Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Available from: https://www.nlm.nih.gov/books/NBK424848/.
- Timko C, Schultz NR, Cucciare MA, Vittorio L, Garrison- Diehn C (2016) Retention in medication-assisted treatment for opiate dependence: A systematic review. J Addict Dis 35: 22-35.
- Treating Substance Use Disorder in Older Adults (2020) Substance Abuse and Mental Health Services Available from: https://www.ncbi.nlm.nih.gov/books/NBK571036/.

