A Case of Chronic Aortic Dissection in Malagasy Patient Suspected of Turner Syndrome
© 2023 Holy Mihanta Sabrina Ranaivoson, Rado Olivier Rakoto Sedson, Nancy Lorena Rakotomalala, Nirina Rabearivony, Solofonirina Rakotoarimanana, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The association between aortic dissection and Turner syndrome has been described in the literature as rare. We report a case of a Stanford type-A chronic aortic dissection in a woman suspected of Turner syndrom. Our goal is to recall the association between these two diseases for early detection and follow-up.
Introduction
Turner syndrome was first described by Henry Turner in 1938. It is one of the most common chromosomal abnormalities. More than 95% of adult women with Turner syndrome have short stature and infertility [1]. Turner syndrome is associated with an increased risk of aneurysms and aortic dissection, which increases the morbidity and mortality of the disease [2].
Medical observation
Our patient was a 51-year-old woman presented at the clinic complaining of chest pain. First episode of this chest pain had appeared 2 years ago with a back and migratory irradiation, intense associated with a dyspnea of progressive aggravation NYHA (New York Heart Association) class II to III associated with a nocturnal cough.
She had no secondary sexual characteristics and primary infertility, and had hypertension for 5 years treated regularly with amlodipin. She had a sister who died at the age of 40 years for sudden death whose etiology was not explored. Cardiovascular examination revealed mild high blood pressure (150/90mmHg), heart rate: 80 beats/min and her heart aortic insufficiency murmur 4/6, no sign of heart failure. The morphological examination of the patient revealed a small size, she was 135 cm tall and weighed 45 kg (Body Surface Area: 1,3m 2 ). She presented a malformation and hypotrophy of the left lower limb, synddromic facies, an absence of secondary sexual characteristics.
The electrocardiography had recorded a regular sinus rhythm, normal axis, normal duration of QRS complex, negative T waves from V1 to V4, absence of arrhythmia and cardiac conduction disorder.
The patient had normal renal function with a creatinine level of 77 mmol/L. Echocardiography found normal left ventricular systolic function (LVEF) at 67% in biplane Simpson, dilated left heart chambers with left ventricular end-diastolic volume (LVEDV) at 110 ml/m2 , left ventricular end-systolic volume (LVESV) at 37 ml/ m2 , a dilated left atrium (LA) at 45 ml/m 2 , a dilation of the thoracic aorta with a sinus of Valsalva at 3,4cm/m2 , a sino-tubular junction at 3,6cm/m2 , an ascending aorta at 3,9cm/m2 . The descending aorta had no dilation or aortic coarctation, and was normal in size. The aortic valve was tricuspid. There was a thick intimal flap at the aortic root and the aortic valve had severe eccentric leakage. There was no pericardial effusion. Genetic testing for Turner syndrome karyotype could not be performed and surgical treatment is not feasible in Madagascar due to the lack of a technical platform, which is the limit of our observation. We put the patient on medical treatment with beta-blocker, diuretic and losartan. After 6 months of the discovery of her aortic dissection, chest pain occurred at the slightest effort with associated dyspnea. Echocardiography revealed the appearance of a portal of entry of the dissection at the level of the sinus of valsalva, the systolic function of the left ventricle remained preserved and there was no appearance of a pericardial effusion.
Discussion
The small size, the syndromic facies, and the anomaly of the lower limb make us suspect a Turner syndrome. Turner syndrome is due to a chromosomal anomaly in women characterized by a complete or partial loss of 1 of the 2 X chromosomes. It is characterized by short stature, absence of menarche and absence of the growth spurt. Other clinical features may be present such as typical dysmorphia, renal, cardiac, skeletal and metabolic abnormalities [2]. Our patient had mild hypertension (Blood pressure 150/90mmHg). The prevalence of hypertension is clearly increased in girls and adults with Turner syndrome. It affects up to 25% of adolescents and 40-60% of adults with Turner syndrome [3, 4]. This hypertension is often mild hypertension in patients with Turner syndrome who have presented with aortic dissection [5].
Echocardiography is a non-invasive exam, easily accessible screening test. At the time of diagnosis of Turner syndrome, every patient should have a cardiovascular imaging test such as TTE or cardiac MRI (Magnetic Resonance Imaging). Children who have had an antenatal imaging test should have repeat cardiac imaging tests at a later date. Common abnormalities detected by MRI but not visualized by Echocardiography include elongated transverse aortic arch, aberrant right subclavian artery and abnormal pulmonary venous returns. Disturbances in cardiac conduction or repolarization, a prolonged QT interval, have been described and attributed to neuroautonomic dysfunction. An electrocardiogram should be performed with cardiac imaging studies [6]. All aortic measurements should therefore be indexed to body surface area (BSA). An indexed aortic diameter >2 cm/m 2 in the ascending aorta should be monitored annually, as the risk of aortic dissection is increased [7]. Cardiac imaging of the aorta should be performed every 5 to 10 years to assess and monitor aortic diameters even in those with a normal initial cardiac study [8]. Aortic dissection, occurs in 1-2% of the Turner syndrome population and is usually preceded by dilatation of the aortic root and ascending aorta. Dissection occurs relatively early in life at a median age of 35 years [9]. The late onset of our patient's aortic dissection was probably due to her nulliparity. The majority of aortic dissections occur during pregnancy [10].
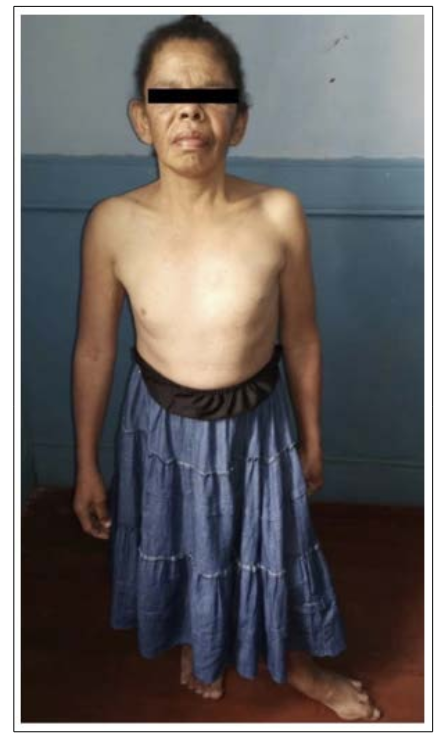
Figure 1: Our Malagasy patient with short stature, absence of secondary sexual characteristics, typical of a Turner syndrome

Figure 2: Image of a thick intimal flap, apical section 5 cavity centered on the aorta in echocardiography
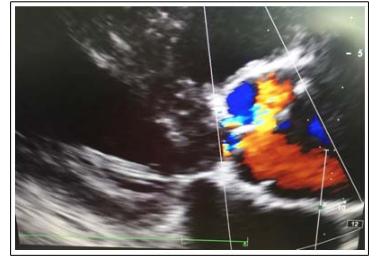
Figure 3: Cardiac Doppler ultrasound image in a parasternal long axis slice: image of the portal of entry at the level of the intimal
Conclusion
The occurrence of aortic dissection is a serious complication in patients with Turner syndrome. When faced with discovery of syndromic morphotypes such as small size and absence of menarche, Turner syndrome should be suspected, cardiovascular damage should be screened and these patients should be monitored for cardiovascular disease even if it is absent at screening. Hypertension is a risk factor for the progression of ascending aortic aneurysm and its progression to dissection.
References
- G Nabi, ON Siraj (2011) Turner Syndrome in a neonate. Physicians Academy. Octobre 5: 130-133
- C Pater, I Gutmark-Little, J Tretter, L Martin, P Backeljauw, et al. (2022) Rate of aortic dilatation in Turner syndrome. JACC. Mars 73: 601
- T Cheng, X Li, J Chen, L Yang, J Liu, et al. (2022) Investigating Hub Genes Involved in Turner Syndrome Using Biological Computational Methods. Medicine. Mars 101.
- Y Dulac, C Pienkowski, S Abadir, M Tauber, P Acar (2008) Cardiovascular abnormalities in Turner’s syndrome: what prevention? Arch Cardiovasc Dis 101: 485-490.
- NC Nathwani, R Unwin, CG Brook (2000). Blood pressure and Turner syndrome. Clin Endocrinol 52: 363-370.
- CA Bondy (2008) Aortic Dissection in Turner Syndrome. Curr Opin Cardiol 23: 519-526.
- ML Davenport (2010) Approach to the Patient with Turner Syndrome. J Clin Endocrinol Metab, April 95:1487-1495.
- CH Gravholt, K Landin-Wilhelmsen, K Stochholm, BE Hjerrild, T Ledet, et al. (2006) Clinical and epidemiological description of aortic dissection in Turner’s syndrome. Cardiol Young 16: 430-436.
- CH Gravholt (2002) Turner Syndrome and the Heart Cardiovascular Complications and Treatment Strategies. Am J Cardiovasc Drug 2: 401-413.
- H Baumgartner, J De Backer, SV Babu-Narayan, W Budts, M Chessa, et al. (2021) ESC Guidelines for the management of adult congenital heart disease 2020. European Heart Journal 42: 563-645.

