Patient Centered Preference Survey for Identifying a Proceduralist Performing Endobronchial Ultrasound Bronchoscopy (EBUS)
© 2022 Amit K Mahajan, Bonnie Fairbanks, Lolita Ramsey, Priya P Patel, Kevin Duong, et al., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Endobronchial ultrasound bronchoscopy (EBUS) is a minimally invasive procedure using real-time imaging to biopsy malignant and benign lesions within the thoracic cavity. While physicians rely heavily on the degree of training to obtain EBUS procedural proficiency, patients may not consider training to be the primary factor that influences the physician they choose. Traditionally, patients undergoing any medical procedure assume that the treating physician has completed standardized training and is proficient in procedural techniques. Because there is no standardized training for EBUS, patients cannot necessarily rely on the level of training of the physician performing the procedure. This survey-based study examines factors that were most and least important to patients regarding the physician who would be performing their EBUS bronchoscopy.
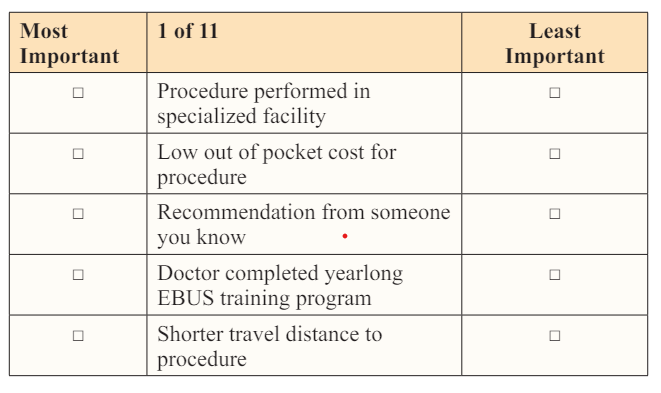
Methods: Using best-worst scaling (BWS), object case methods (case 1; Louviere et al, 2015), a survey was developed with a balanced incomplete block design (BIBD): 11 objects (Figure 1), repeated 5 times across 11 sets with a set size of 5 and co-occurs with the other 10 objects twice. In the survey, titled EBUS Patient Preference Survey, participants were instructed to identify the factors (objects) that were most and least important to them when making arrangements for an EBUS procedure. The data was analyzed by calculating a normalized best-worst (NBW) score for the total sample/aggregate for each object. The data was also analyzed as a percentage distribution on the proportion selected as most versus least important versus never selected (denominator = 930). Analyses were conducted using SPSS (IBM Corp, Version 26.0).
Results: Of the 193 patients who consented, 3 withdrew due to the length of the survey and 4 incorrectly completed the survey, resulting in a sample size of 186. The overall sample felt that a doctor who communicated well was most important to them when arranging for an EBUS procedure, followed by a physician with more years of experience performing EBUS, referral from their doctor, and procedure performed in a specialized facility. ). The least important factor when arranging for an EBUS procedure was out of pocket cost for procedure, time to scheduling, and positive doctor rating online.
Conclusions: Our study reveals that patients prefer physicians who communicates well, has more years of experience performing EBUS, and was referred to by their physician to be the most important factors when choosing an EBUS proceduralist.
Introduction
Endobronchial ultrasound bronchoscopy (EBUS) is a minimally invasive procedure using real-time imaging to biopsy malignant and benign lesions within the thoracic cavity. Bronchoscopy utilizing EBUS shows a significant increase in diagnostic yield by transbronchial needle aspiration (TBNA) in all lymph nodes stations, except for the subcarinal regions, when compared to conventional, non-image-guided bronchoscopic TBNA [1]. The use of EBUS-TBNA by pulmonologists and thoracic surgeons has become a standard procedure for the important task of diagnosing and staging lung cancer.
While physicians rely heavily on the degree of training to obtain EBUS procedural proficiency, patients may not consider training to be the primary factor that influences the physician they choose. Traditionally, patients undergoing any medical procedure assume that the treating physician has completed standardized training and is proficient in procedural techniques. Because there is no standardized training for EBUS, patients cannot necessarily rely on the level of training of the physician performing the procedure. Instead, patients may rely more heavily on factors such as distance needed to travel for the procedure, who their referring physician recommends performing the procedure, and the number of procedures performed per year.
This survey-based study examines factors that were most and least important to patients regarding the physician who would be performing their EBUS bronchoscopy. A variety of elements were considered when determining patient preference. To our knowledge, no study has examined patient preferences for physicians performing EBUS bronchoscopy
Methods
Using best-worst scaling (BWS), object case methods (case 1; Louviere et al, 2015), a survey was developed with a balanced incomplete block design (BIBD): 11 objects (Figure 1), repeated 5 times across 11 sets with a set size of 5 and co-occurs with the other 10 objects twice. Objects were developed based on a literature review and were pilot tested. In the survey, titled EBUS Patient Preference Survey, participants were instructed to identify the factors (objects) that were most and least important to them when making arrangements for an EBUS procedure (Figure 1). This study was approved by the Western Institutional Review Board. Patients were approached to consent for study in the pre-procedural area and asked to complete the survey prior to the EBUS procedure, with or without navigation bronchoscopy. The average time to complete the self-administered paper survey was 20 minutes.
The data was analyzed by calculating a normalized best-worst (NBW) score for the total sample/aggregate for each object. The frequency to which an object was selected as the most important was subtracted from the number of times selected as least important. This difference was divided by the total availability, which was the sample size multiplied by the number of times that object appeared in the survey (185 x 5 =930); (NBW score = (N Most - NLeast)divided by(N x 5)). The NBW score ranges from -1 to +1. Positive values closer to +1 indicate objects that are considered most important in aggregate, 0 indicates neither and negative values closer to -1 indicate the least important object selected by the cohort. The data was also analyzed as a percentage distribution on the proportion selected as most versus least important versus never selected (denominator = 930). Analyses was conducted using SPSS (IBM Corp, Version 26.0).
Figure 1: Example of Patient Preference Survey Question
Now it is your turn. You will see 11 different questions like this. Which of these things are the most and the least important to you when choosing the doctor who will perform your EBUS? Please check one box for “Most Important” column and one box for “Least Important” column.
Results
Of the 193 patients who consented, 3 withdrew due to the length of the survey and 4 incorrectly completed the survey, resulting in a sample size of 186. The average age was 63 years old, with an equal distribution of male to female participants (Figure 2). The majority of this cohort was Caucasian (71.5%), with a higher level of education and employment (bachelor’s or graduate degree = 59.5%; full-time or part-time employment = 47.4%). 75.1% denied working in a primary job that exposed them to dust or breathable particles. Smoking status varied, with 44.6% never smoked more than 100 cigarettes, cigars or pipes in their lifetime, followed by 41.3% with a history of smoking, 13% with current smoking in the past 4 weeks, and 1.1% reported smoking but unknown if this was current or history.
The overall sample felt that a doctor who communicated well was most important to them when arranging for an EBUS procedure, followed by a physician with more years of experience performing EBUS, referral from their doctor, and procedure performed in a specialized facility (Figure 2). The least important factor when arranging for an EBUS procedure was out of pocket cost for procedure, time to scheduling, and positive doctor rating online. A distribution of item selection percentages is depicted in Figure 3. A recommendation from someone you know had the highest percentage in the never selected category and low out of pocket cost had the highest percentage in selection as the least important factor.
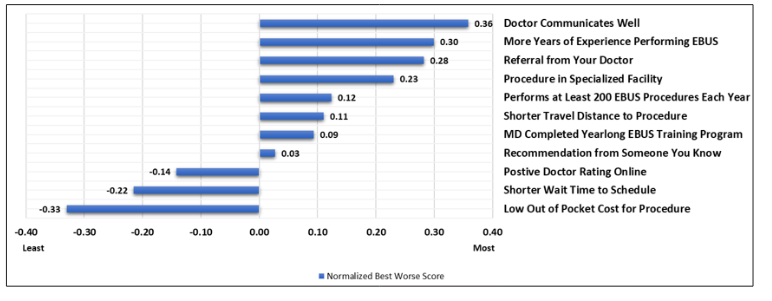
Figure 2: Patient Preference in EBUS, Factors Most Important to Least Important
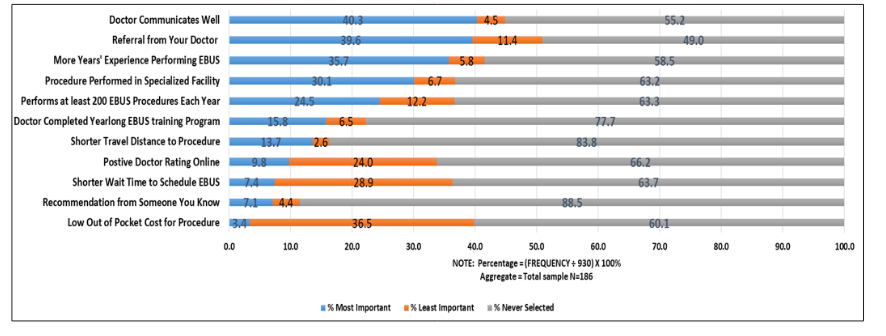
Figure 3: Distribution of Item Selection (Aggregate, %)
Discussion
We have demonstrated that patients undergoing EBUS bronchoscopy consider a physician who communicates well, has more years of experience performing EBUS, was referred to by their primary physician, and has the procedure performed at a specialized facility to be among the most important factors when choosing a proceduralist. These factors were more important than the number of EBUS procedures performed per year or the level of training (IP fellowship completion) of the physician who is performing the EBUS. This finding is contrary the traditional assumption that proceduralists with more advanced training in EBUS and performed more procedures per month would be more desired by patients, which is a common belief held by physicians. Instead, patients appear to prefer more experienced physicians regardless of training level.
The most important factor patients sought in their procedural physician was the ability to communicate well rather than procedural training. The ability for physicians to describe the EBUS procedure, relay expectations, and discuss results appears to be central to patient satisfaction. Patient surveys have consistently shown that patients want better communication with their doctors [2]. Patients reporting good communication with their doctor are more likely to be satisfied with their care, and especially to share pertinent information for accurate diagnosis of their problems, follow advice, and adhere to the prescribed treatment [3-7]. Additionally, satisfied patients are advantageous for doctors in terms of greater job satisfaction, less work-related stress, and reduced burnout [8, 9].
The significance of physician experience in EBUS rather than the level of training for patient satisfaction is reinforced by procedural competency data. Learning curve assessments regarding EBUS competency indicates that performance continues to improve up to 120 to 160 EBUS procedures [10, 11]. Fernandez-Villar et al. Medford et al both assessed the diagnostic accuracy achieved for increasing number of EBUS procedures performed (Figure 3). Fernandez-Villar et al. analyzed performance in unselected consecutive patients based on diagnostic yield, procedure length, number of lymph nodes passes performed in order to obtain adequate samples, and the number of lymph nodes studied per patient. Learning curves were evaluated by assessing consecutive groups of 20 patients, the number of adequate samples obtained, and the diagnostic accuracy of the patient. Their analysis indicates that the diagnostic effectiveness of EBUS-TBNA improves with increasing number of procedures performed. Additionally, with more procedures performed, physicians were able to access a greater number of lymph nodes without increasing length of time needed to perform the procedure, and by reducing the number of punctures in each nodal station. Similarly, Medford conducted a study during which one operator performed 160 consecutive EBUS-TBNA procedures over an 18-month period for a similar unselected cohort as those in Fernandez-Villar’s study with mediastinal or hilar lymph nodes. Based on Medford’s and Fernandez-Villar data, diagnostic accuracy can be achieved after completion of 40-60 EBUS procedures. Currently, physician’s in general pulmonary training can reach these learning curve targets without completing a specialized IP fellowship. In these situations, once adequate volumes are achieved, general pulmonologists who have longevity in EBUS may be more desirable to patients than the less experienced physician who may have completed a specialized IP fellowship.
An ongoing debate continues regarding the number of EBUS procedures needed to be performed to attain basic competency. Both the American Thoracic Society (ATS) and the American College of Chest Physicians (ACCP) have published recommendations for initial acquisition and maintenance of competency based on number of procedures performed [12, 13]. Additional training can be acquired for general pulmonologist in EBUS procedures in multiple ways including fellowship rotation with IP service at their fellowship institution, attending weekend course with high fidelity training models (cadaver, animals), and observation/ sabbatical training at high volume centers [14]. Unfortunately, the ability to perform EBUS bronchoscopy in hospitals is usually based on institutional credentialing, which is often significantly lower than those recommended by the ATS and ACCP. While fellowship training is often equated with procedural proficiency, patient preference does not necessarily depend on level of training. Unfortunately, due to the variability in the training and the lack of standardization in assessing procedural competency makes reliance purely on number of procedures performed to be inappropriate. Instead, focus on competency-based metrics and simulator utilization is favored.
A limitation of this study is inherent in the design of BWS. Depending on the number of objects and BIBD, the length of the survey can be a burden. Participants require clear instructions and/or confirmation upon survey completion.
Factors influencing patient preference for procedure lists performing EBUS bronchoscopy are rarely considered and may vary significantly. Our study reveals that patients prefer physicians who communicates well, has more years of experience performing EBUS, and was referred to by their physician to be the most important factors when choosing an EBUS proceduralist. These findings suggest that formal IP fellowships may expose trainees to an increase number of EBUS procedures, but studies show that the number of procedures does not always translate to mastery. Instead, experienced physicians, both with procedures and communication skills, may be more desired by patients than formal advanced IP fellowship training.
References
- Herth F, Becker HD, Ernst A (2004) Conventional vs endobronchial ultrasound-guided transbronchial needle aspiration: a randomized trial. Chest 125: 322-325.
- Duffy FD, Gordon GH, Whelan G, Kathy Cole-Kelly, Richard Frankel, et al. (2004) Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med 79: 495-507.
- Hall JA, Roter DL, Rand CS (1981) Communication of affect between patient and physician. J Health Soc Behav 22: 18-30.
- Herndon J, Pollick K (2002) Continuing concerns, new challenges, and next steps in physician-patient communication. J Bone Joint Surg Am 84: 309-315.
- Kindler CH, Szirt L, Sommer D, Hausler R, Langewitz W (2005) A quantitative analysis of anaesthetist-patient communication during the pre-operative visit. Anaesthesia 60: 53-59.
- Kaplan SH, Greenfield S, Ware JE (1989) Jr assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 27: S110-S127.
- Harmon G, Lefante J, Krousel-Wood M (2006) Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol 21: 310- 315.
- Bredart A, Bouleuc C, Dolbeault S (2005) Doctor-patient communication and satisfaction with care in oncology. Curr Opin Oncol 17: 351-354.
- Maguire P, Pitceathly C (2002) Key communication skills and how to acquire them. BMJ 325: 697-700.
- Fernandez-Villar A, Leiro-Fernandez V, Botana-Rial M, Represas-Represas C, Nunez-Delgado M (2012) The endobronchial ultrasound-guided transbronchial needle biopsy learning curve for mediastinal and hilar lymph node diagnosis. Chest 141: 278-279.
- Medford AR. Learning curve for endobronchial ultrasoundguided transbronchial needle aspiration. Chest 141: 1643.
- Ernst A, Silvestri GA, Johnstone D (2003) Interventional pulmonary procedures: Guidelines from the American College of Chest Physicians. Chest 123: 1693-1717.
- Bolliger CT, Mathur PN, Beamis JF (2002) ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J 19: 356-373.
- Wahidi MM, Hulett C, Pastis N (2014) Learning experience of linear endobronchial ultrasound among pulmonary trainees. Chest 145: 574-578.

