Knowledge and Attitude Among Medical and Non-Medical Students Regarding Tuberculosis: A Questionnaire Based Study
© 2023 Qadeer Ahmed, Muhammad Talha, Abdul Qadeer, Muhammad Zubair, Ali Akhtar, et al., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Tuberculosis is a major global health concern, ranking as the second most deadly infectious disease. Over 8 million people worldwide develop active TB, with the majority of cases occurring in developing countries. The World Health Organization has highlighted the importance of education in ensuring that medical students graduate with the knowledge, skills, and attitudes necessary for effective TB management.
Objective: The purpose of this study was to assess the level of knowledge, attitude among medical and non-medical students regarding the tuberculosis. Method: A cross sectional survey was performed among medical and non-medical students. Knowledge and attitude of the participants regarding the tuberculosis were assessed using a validated questionnaire. The collected data was analyzed using statistical methods to draw the achieve the study objectives.
Results: The data was collected from 300 students, of whom 53% are medical students and 46.7% are non-medical students. Most students in both groups answered correctly that TB is caused by M. tuberculosis, that a persistent cough with sputum is a symptom, that HIV positive people are more at risk, that TB is spread by air, that BCG vaccine can prevent it, and that chest X-ray can diagnose it. However, some students in both groups did not know that not every TB patient needs to be hospitalized and that the standard treatment for new cases of pulmonary TB is a six-month course of four drugs. This shows that some students need more education on these aspects of TB management.
Conclusion: The study concluded that more efforts should be made to improve the knowledge of medical students regarding TB transmission and the role of sputum smear in diagnosis, as well as emphasis on the importance of the BCG vaccination.
Introduction
Tuberculosis (TB) is a widespread infectious disease caused by mycobacterium tuberculosis. It remains a significant public health issue globally, particularly in low and middle-income countries [1]. According to the World Health Organization (WHO) Global TB Report 2019, TB resulted in an estimated 1.3 million deaths among HIV-negative individuals and an additional 300,000 deaths among HIV-positive individuals [2].
Pathogenesis
Pathogenesis of tuberculosis involve a complex interplay between the bacterium and the immune system of the infected individual such as formation of granuloma’s, that are due innate inflammatory response of an individual immune systems [3]. Persistent response of immune system can cause tissue damage [4]. Alveolar infections occur due to deposition of bacilli into alveoli.
Sign and Symptoms
The lung is the organ most commonly affected by tuberculosis infection in immune-competent hosts, with 79 to 87% of subjects with active tuberculosis having lung involvement [5]. Common symptoms include cough, fever, weight loss and Hemoptysis. Other symptoms of TB such as weakness, fatigue, headache, and weight loss may occur. Chest pain and SOB may also occur. Fever usually develops in the late afternoon and may not have pronounced symptoms. Sweating during sleep is common, known as the classic night sweat [6].
Diagnosis
The most helpful study for indicating a tuberculosis diagnosis is the chest radiographs [7]. Regular lab tests are seldom useful in confirming or indicating a diagnosis [5]. In chronic tuberculosis, a mild anemia with normal red blood cell size and colour may be present. CT scans provide a more detailed view of the pulmonary tissue and lymph nodes than plain chest X-rays. In primary tuberculosis patients, chest CT typically shows lobar consolidation with mediastinal or hilar adenopathy.
Treatment of Tuberculosis
Clinical trials conducted by the U.K. Medical Research Council and the U.S. Public Health Services between 1948 and 1986 found that completing a 6-month course of multidrug therapy Is oniazid,Rifampin,Ethambutol,and Pyrazinamide could cure drug- susceptible tuberculosis with a less than 5-8% chance of relapse [8]. When relapse occurs, it usually happens within 12 months after therapy completion [9].
Side Effects of Anti-Tuberculosis Drugs
Patients with minor side effects should be encouraged to continue treatment with symptomatic measures such as antacids, antihistamines, anti-emetics, or analgesics. If major side effects occur, the regimen or the offending drug must be stopped. Further management depends on the nature of the side effects and may require hospitalization [10].
Liver damage is a significant adverse reaction to anti-tuberculosis drugs that may restrict their use. Some other side effects may include Postural hypotension, depression, asthenia, drowsiness, Skin rash, purpura, gynecomastia, impotence.
Methodology Study Design
A cross sectional survey was conducted to explore the research question [11]. The study focused on medical and non-medical students in Pakistan and collected data from 300 participants through both online and face to face means.
Study Population
The study focused on medical students enrolled in MBBS and other students enrolled in non-medical programs.
Inclusion Criteria
Medical students must be enrolled in MBBS. Participants must be between the Ages of 15-30.
Exclusion Criteria
Students who have previously been diagnosed with tuberculosis. Students who are unable to complete the survey due to language barriers or other reasons
Sample Size
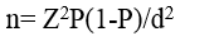
The number of participants in this study was 300. This number was determined by adding or subtracting 18 from the sample size which is obtained by the Daniel, 1999 formula which should be given as:
Ethical Approval
This study received ethical approval from the Riphah Institute of pharmaceutical sciences (RIPS) Riphah International University (RIU).
Statistical Analysis
The study’s data was analyzed using statistical package for social sciences (SPSS) to perform a descriptive frequency analysis of the data.
Results
The results of this study offer a comprehensive view of tuberculosis knowledge among medical and non-medical students. By analyzing the frequency and percentage of responses, valuable insights are provided.
Demographics Data
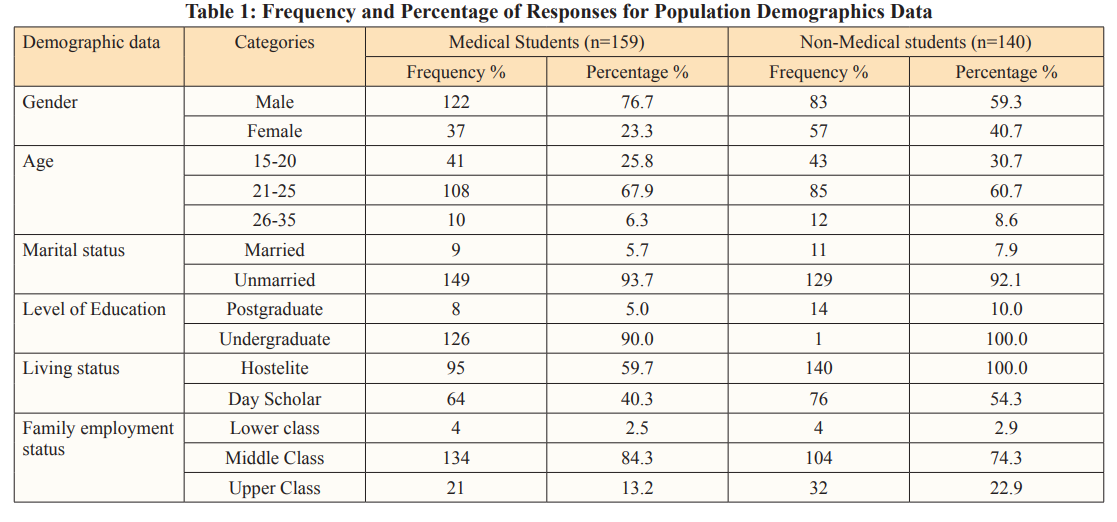
A total number of 300 Students data was collected. Out of these (53%) of the respondents are medical students while (46.7%) are not. (68.7%) of the respondents are male while (31.3%) are female. The majority of the respondents (64.7%) are between the ages of 21-25, followed by (28%) between the ages of 15-20 and 7.3% between the ages of 26-30.The vast majority (93%) of the respondents are unmarried. Most of the respondents (92.7%) are undergraduate students while 7.3% are postgraduate students. (53.3%) of the respondents are hostelite while (46.7%) are day scholars. The majority (79.7%) of the respondents come from middle-class families, followed by 17.7% from upper-class families and 2.7% from lower-class families.
Knowledge of Tuberculosis
Knowledge Regarding the Etiology, Transmission and Symptoms
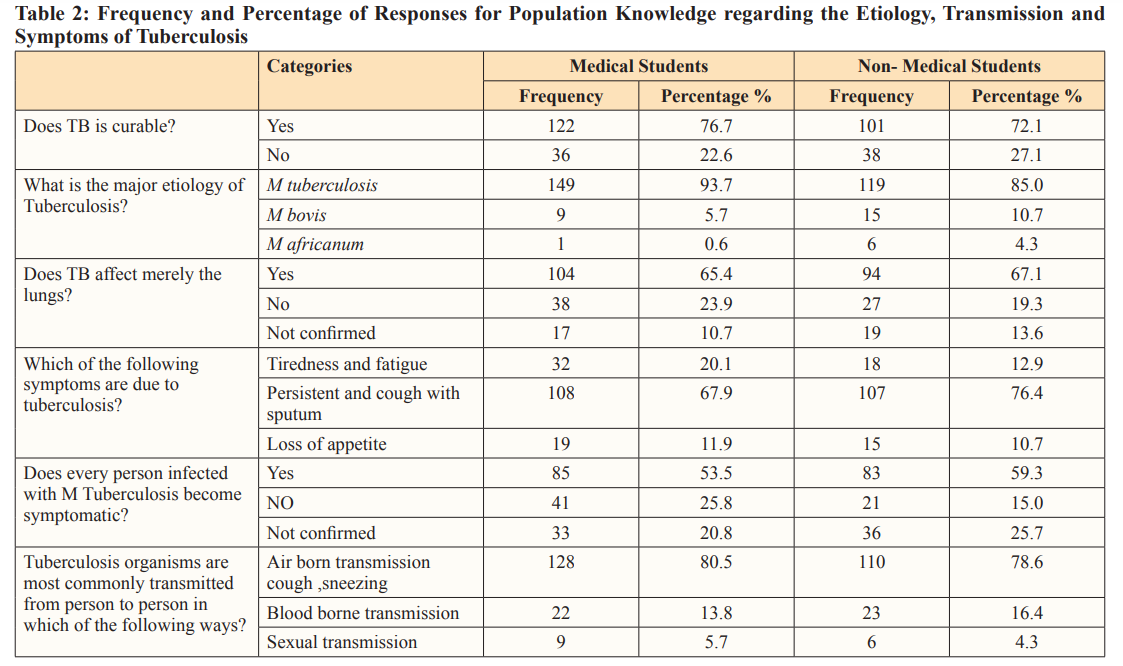
Table 2 gives brief information about the etiology, transmission, and symptoms of tuberculosis among medical and non-medical students. The data was collected from 300 students. Among these (76.7%) of medical students and (72.1%) of non-medical students believe that TB is curable. (93.7%) of medical students and (85.0%) of non-medical students believed that M. tuberculosis as the major etiology of tuberculosis. (65.4%) of medical students and (67.1%) of non-medical students believe that TB affects merely the lungs. The most commonly identified symptom of tuberculosis among both medical and non-medical students was a persistent cough with sputum (67.9% and 76.4%, respectively). (53.5%) of medical students and (59.3%) of non-medical students believe that every person infected with M. tuberculosis becomes symptomatic. The majority of both medical and non-medical students (80.5% and 78.6%, respectively) identified that airborne transmission through sneezing is the most common way that tuberculosis organisms are transmitted from person to person.
Knowledge Regarding the Risk Factors of Tuberculosis
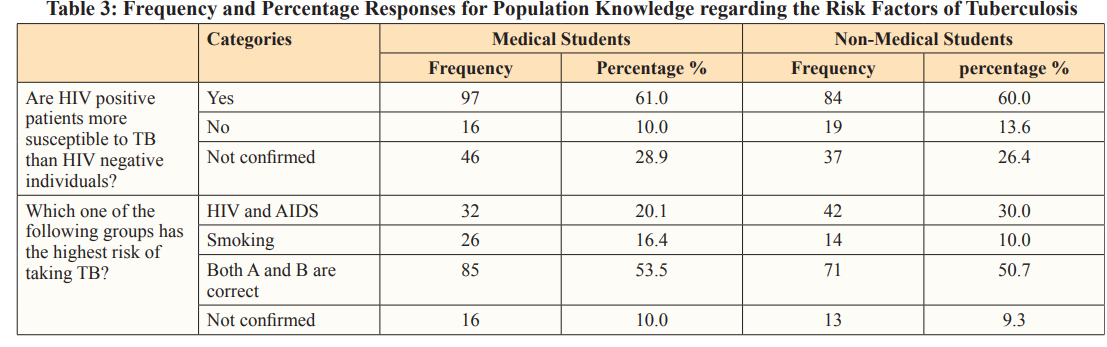
Table 3 gives brief information about the risk factors of tuberculosis among medical and non-medical students. The data was collected from 300 students. Among these (61.0%) of medical students and (60.0%) of non-medical students believe that HIV positive patients are more susceptible to TB than HIV negative individuals.When asked which group has the highest risk of taking TB, (53.5%) of medical students and (50.7%) of non-medical students correctly identified that both HIV/AIDS and smoking are risk factors for TB.
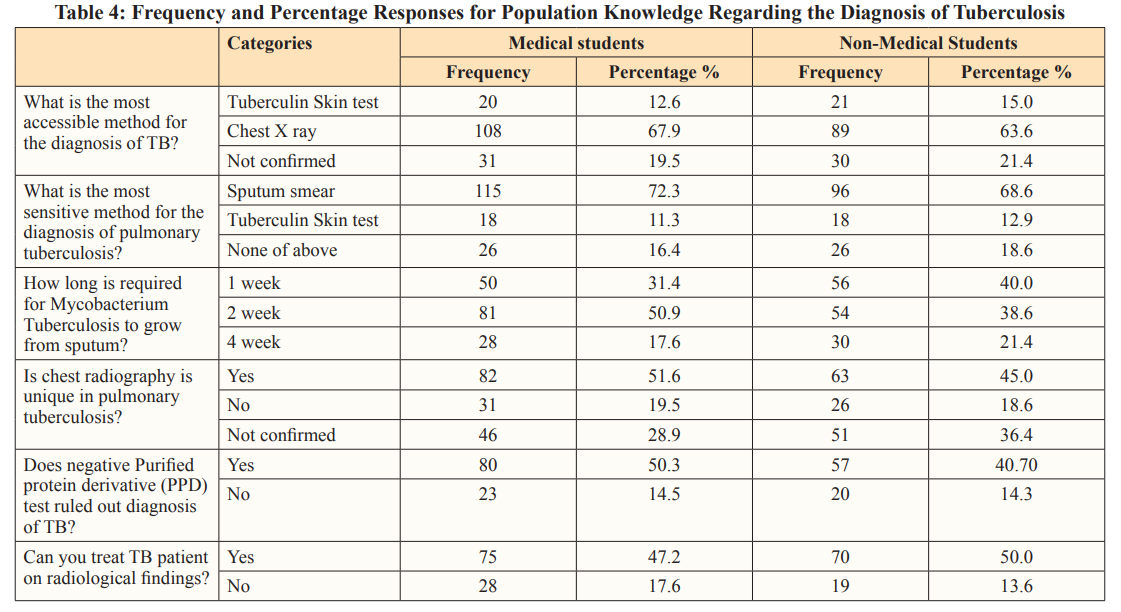
Knowledge regarding the Diagnosis of Tuberculosis
Table 4 gives brief information about the risk factors of tuberculosis among medical and non-medical students. The data was collected from 300 students. Among these students When asked about the most accessible method for the diagnosis of TB, (67.9%) of medical students and (63.6%) of non-medical students identified chest X-ray as the most accessible method. When asked about the most sensitive method for the diagnosis of pulmonary tuberculosis, (72.3%) of medical students and (68.6%) of non-medical students believed that sputum smear as the most sensitive method. When asked how long it takes for Mycobacterium tuberculosis to grow from sputum, (50.9%) of medical students and (38.6%) of non-medical students correctly identified that it takes 2 weeks. When asked if chest radiography is unique in pulmonary tuberculosis, (51.6%) of medical students and (45.0%) of non-medical students responded “Yes”. When asked if a negative purified protein derivative (PPD) test rules out the diagnosis of TB, (50.3%) of medical students and (40.7%) of non-medical students responded “Yes”. When asked if a TB patient can be treated based on radiological findings alone, (47.2%) of medical students and (50.0%) of non-medical students responded “Yes”.
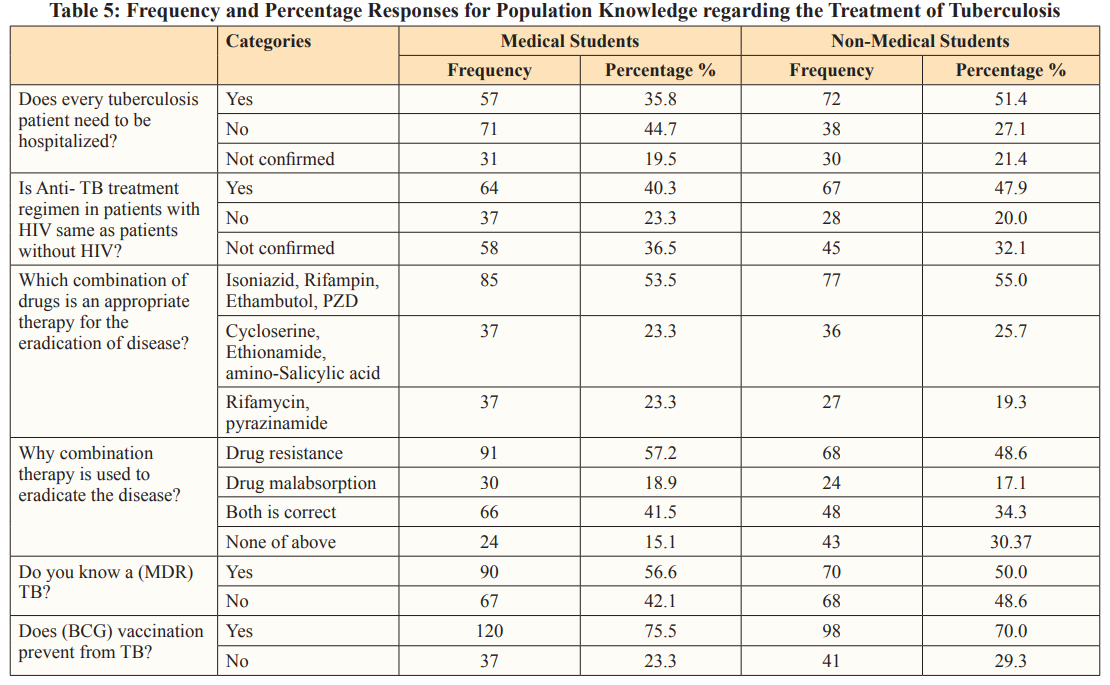
Knowledge Regarding the Treatment of Tuberculosis
Table 5 gives brief information about the risk factors of tuberculosis among medical and non-medical students. The data was collected from 300 students. When asked if every tuberculosis patient needs to be hospitalized, 44.7% of medical students and 27.1% of non- medical students responded “No”. When asked if the anti-TB treatment regimen in patients with HIV is the same as in patients without HIV, 40.3% of medical students and 47.9% of non-medical students responded “Yes”. When asked about the appropriate combination of drugs for the eradication of TB, 53.5% of medical students and 55.0% of non-medical students answered that Isoniazid, Rifampin, Ethambutol, and PZD as an appropriate therapy. When asked why combination therapy is used to eradicate TB, 57.2% of medical students and 48.6% of non-medical students answered that drug resistance as a reason for using combination therapy. When asked if they know what MDR TB is, 56.6% of medical students and 50.0% of non-medical students responded “Yes”. When asked if BCG vaccination prevents TB, 75.5% of medical students and 70.0% of non-medical students responded “Yes”.
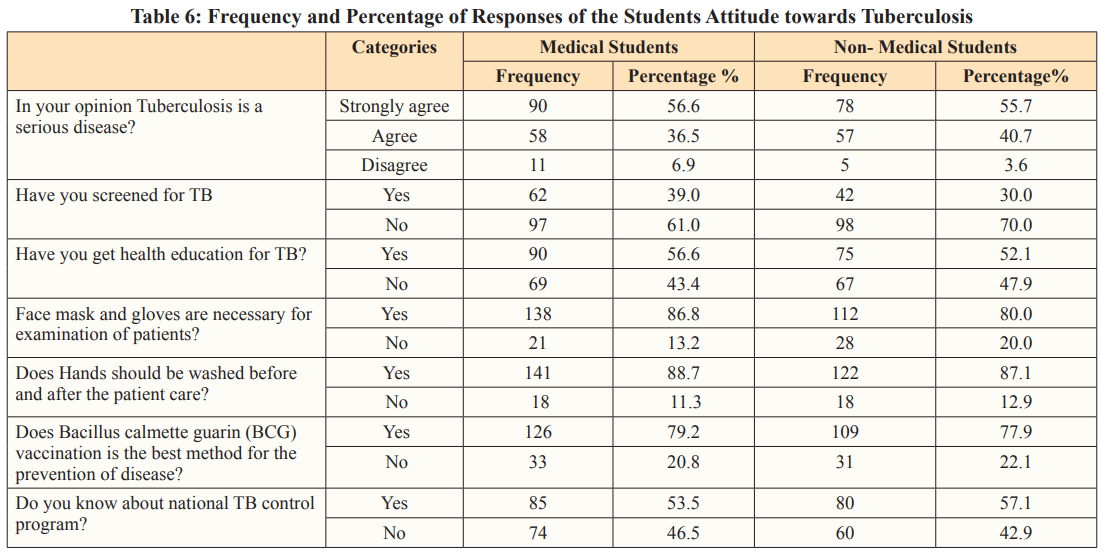
Attitudetowards Tuberculosis
Table 6 gives brief information about the attitude of the students towards the tuberculosis. A total number of 300 Students data was collected. Among these 94.6% of respondents either strongly agree (56.3%) or agree (38.3%) that tuberculosis is a serious disease while only 5.3% disagree.34.7% of respondents have been screened for TB while 65.3% have not.54.7% of respondents have received health education for TB while 45.3% have not.83.7% of respondents believe that wearing a face mask and gloves is necessary for the examination of tuberculosis patients while 16.3% do not.88.0% of respondents believe that hands should be washed before and after patient care while 12.0% do not.78.7% of respondents believe that Bacillus Calmette-Guerin (BCG) vaccination is the best method for the prevention of disease while 21.3% do not. Finally, 55.3% of respondents know about the national TB control program while 44.7% do not.
Discussion
The study focused on the common manifestations, etiology, transmission, latent infection, vaccination, and treatment of TB. The data revealed that majority of both medical and non-medical students demonstrated adequate knowledge of the basic aspects of tuberculosis (TB) such as etiology, major affecting organ, and prevention symptoms, transmission [12-15]. These findings are consistent with the results of previous studies performed by Tolossa et al, Rana et al, on the respective topics. The data in this study revealed that (67%) of the medical and (63%) of the non-medical students answered that chest X-ray is the most accessible method for diagnosing TB that is related to the study performed by Van Cleef [15]. The majority of students in both groups also correctly identified that sputum smear is the most sensitive method for diagnosing pulmonary TB. This is consistent with the results of study by Ramsay et al [16]. In this study (76.7%) of the medical students and (72.1%) of the non-medical students answered that TB is completely curable. that is related with the study performed by Goletti, Arlehamn [17]. The data also showed that only (44.7%) of the medical students and (27%) of the non-medical students answered that every person infected with TB not need to be hospitalized and (35.8%) of the medical students and (51.4%) of the non-medical students answered that every TB patient need hospitalization. Benefits of hospitalization includes isolation of infectious patients but hospitalization is the most costly health system component of tuberculosis (TB) control programs. This is consistent with the results of study by Ronald [18]. The data showed that (47.2%) of the medical students and (50%) of the non- medical students answered correctly that TB patients are treated on radiological findings. This is consistent with the results of study by Andreu [19]. On the other hand (35.2%) of the medical students and (36.4%) of the non-medical students answered that they are not confirmed about the treatment on radiological findings and the remaining percentage of both participants answered that TB patients are not treated on radiological findings because Chest radiography is not an accurate method for assessing the activity of post-primary disease that is related to study by McAdams [20]. The data showed that only (27.7%) of the medical students answered correctly about the standard treatment of new case of pulmonary tuberculosis. According to the current TB management guidelines, the treatment regimen for new smear-positive pulmonary tuberculosis (PTB) patients should be six months. This is consistent with the results of study by Mitchison, Ellard et al [8].
The data also revealed that (57.2%) of the medical student and (48.6%) of the non-medical students answered that due to drug resistance combination of therapy is used to eradicate the disease that is related to the study of Johnson [13]. while (19%) of the medical students and (17%) of the non-medical students answered that due to malabsorption of Isoniazid, and Rifampin, combination of drug therapy is used. This is consistent with the results of study by Ramos et al [21]. The data in this study shows that (41.5%) of the medical students (34%) of the non-medical students answered correctly that due to drug resistance, malabsorption, and non-adherence to the therapy are reasons behind the failure of tuberculosis that is closed to the study of Cohen [22]. In this study (56.6%) of the medical students and (50%) of the non-medical students know about the multidrug resistant TB that is consistent with the results of study by Zhang [23]. The data in this stu dy showed that only (35.2%) of the medical students and (30%) of the non-medical students answered correctly that Hepatitis, GI upset and liver failure are the common side effects of anti-tuberculosis drugs that is resembles to study by Ali [1]. The data in this study also showed that (49.7%) of the medical students and (55.7%) of the non-medical students answered correctly that tuberculosis in Pakistan are common in the age of 40-60 years. This is consistent with the results of study by Sultana, Afzal [24].
The data in this study also include the attitude of the participants towards the tuberculosis. It seems to be appears that the majority of both medical and non-medical students believe that tuberculosis is a serious disease, with (56.6%) of medical students and (55.7%) of non- medical students strongly agreeing with this statement. These results are consistent with the results of study by Gelaw, Genebo et al. [25].
A large majority of both groups also believe that face masks and gloves are necessary for the examination of patients and hands should be washed before and after patient care. This is consistent with the results of study by Bai, Xio [26]. The data in this stusdy also shows that just over half of both groups reported knowing about the national TB control program (53.5%) of medical students and (57.1%) of non-medical students that relates to the study performed by Behnaz, Mohammad Zaid [11].
Conclusion
Despite efforts, there have been no significant recent breakthroughs in the development of anti-TB drugs or research that would lead to an immediate and significant reduction in transmission. This means that other cost-effective methods must be considered to sustainably control infectious diseases like TB and counter their increasing prevalence. More efforts should be made to improve the knowledge of medical students regarding TB transmission and the role of sputum smear in diagnosis, as well as emphasis on the importance of the BCG vaccination.
References
- Ali H (2019) Knowledge, attitude and practice regarding tuberculosis management among final year students of two medical colleges of Pakistan Journal of Chest Medicine 25: 166-180.
- Saqib SE (2018) Treatment delay among pulmonary tuberculosis patients within the Pakistan national tuberculosis control The American journal of tropical medicine and hygiene 99: 143-149.
- Orme IM, Basaraba RJ (2014) The formation of the granuloma in tuberculosis Seminars in immunology, Elsevier 26: 601-609.
- Tiwari D, Martineau AR (2023) Inflammation-mediated tissue damage in pulmonary tuberculosis and host-directed therapeutic Seminars in Immunology, Elsevier 65: 1-16.
- Farer LS (1979) Extrapulmonary tuberculosis in the United American journal of epidemiology 109: 205-217.
- Lyon SM, Rossman MD (2017) Pulmonary tuberculosis. Microbiology spectrum 5: 5-24.
- Holden M (1971) Frequency of negative intermediate-strength tuberculin sensitivity in patients with active tuberculosis. New England Journal of Medicine 285: 1506-1509.
- Mitchison D (1999) Studies on the treatment of tuberculosis undertaken by the British Medical Research Council Tuberculosis Unit between 1946-86. Int J Tuberc Lung Dis 10: 231-279.
- Nunn A (2010) Timing of relapse in short-course chemotherapy trials for The International journal of tuberculosis and lung disease 14: 241-242.
- Koju D (2005) Occurrence of side effects from anti- tuberculosis drugs in urban Nepalese population under DOTS Kathmandu University J Sci Eng Technol 1: 1-9.
- Behnaz F (2014) Assessment of knowledge, attitudes and practices regarding tuberculosis among final year students in Yazd, central Iran. Journal of epidemiology and global health 4: 81-85.
- Tolossa D (2014) Community knowledge, attitude, and practices towards tuberculosis in Shinile town, Somali regional state, eastern Ethiopia: a cross-sectional study. BMC Public Health 14: 804-817.
- Johnson R, Elizabeth M Streicher, Gail E Louw, Robin M Warren, Paul D van Helden, et (2006) Drug resistance in Mycobacterium tuberculosis. Current issues in molecular biology 8: 97-111.
- Rana M, Reazul Karim, Nurul Islam, Rafiqul Islam, Tunku Kamarul Zaman, et al. (2015) Assessment of knowledge regarding tuberculosis among non-medical university students in Bangladesh: a cross-sectional BMC Public Health 15: 1-7.
- Van Cleeff M (2005) The role and performance of chest X-ray for the diagnosis of tuberculosis: a cost-effectiveness analysis in Nairobi, BMC Infectious Diseases 5: 111.
- Steingart KR (2007) Optimizing sputum smear microscopy for the diagnosis of pulmonary tuberculosis. Expert review of anti-infective therapy 5: 327-331.
- Goletti D, Cecilia S Lindestam Arlehamn, Thomas J Scriba, Richard Anthony, Daniela Maria Cirillo, et al. (2018) Can we predict tuberculosis cure? What tools are available? European Respiratory Journal 52: 1801089
- Ronald LA, Mark FitzGerald J, Andrea Benedetti, Jean- François Boivin, Kevin Schwartzman, et (2016) Predictors of hospitalization of tuberculosis patients in Montreal, Canada: a retrospective cohort study. BMC Infectious Diseases 16: 679.
- Andreu J (2004) Radiological manifestations of pulmonary European journal of radiology 51: 139-149.
- McAdams HP (1995) Radiologic manifestations of pulmonary Radiologic Clinics of North America 33: 655-678.
- Pinheiro VG, Lysiane MA Ramos, Helena SA Monteiro, Elizabeth C Barroso, Oluma Y Bushen, et al. (2006) Intestinal permeability and malabsorption of rifampin and isoniazid in active pulmonary tuberculosis. Brazilian Journal of Infectious Diseases 10: 374-379.
- Cohen FL (1997) Adherence to therapy in Annual review of nursing research 15: 153-184.
- Zhang Y (1992) The catalase-peroxidase gene and isoniazid resistance of Mycobacterium Nature 358: 591-593.
- Sultana T (2017) Epidemiological estimates of Respiratory diseases in the hospital population, Faisalabad, Pakistan. Brazilian Archives of Biology and Technology 60: 1-12.
- Gelaw M (2001) Attitude and social consequences of tuberculosis in Addis Ababa, East African medical journal 78: 382-387.
- Bai L (2003) Knowledge and practice regarding tuberculosis among final-year medical students in Hunan, Zhonghua jie he he hu xi za zhi= Zhonghua jiehe he huxi zazhi= Chinese journal of tuberculosis and respiratory diseases 26: 458-461.
- Barberis I (2017) The history of tuberculosis: from the first historical records to the isolation of Koch’s Journal of preventive medicine and hygiene 58: 9-12.
- Churchyard G, Peter Kim, N Sarita Shah, Roxana Rustomjee, Neel Gandhi, et (2017) What we know about tuberculosis transmission: an overview. The Journal of infectious diseases 216: 629-635.
- Griffiths G (2010) Nanobead-based interventions for the treatment and prevention of tuberculosis. Nature Reviews Microbiology 8: 827-834.
- Gupta KB (2009) Tuberculosis and nutrition. Lung India: official organ of Indian Chest Society 26: 9-16.
- Hopewell PC, Jasmer RM (2004) Overview of clinical Tuberculosis and the tubercle bacillus. https://onlinelibrary.wiley.com/doi/epdf/10.1128/9781555817657.ch2.
- Horsburgh Jr CR (2015) Treatment of tuberculosis. New England Journal of Medicine 373: 2149-2160.
- Iseman MD (1993) Treatment of multidrug-resistant New England Journal of Medicine 329: 784-791.
- Konstantinos A (2010) Testing for Aust Prescr 33: 12-18.
- Lange C, Mori T (2010) Advances in the diagnosis of Respirology 15: 220-240.
- Lyon SM, Rossman MD (2017) Pulmonary tuberculosis. Microbiology spectrum 5: 5-24.
- Narasimhan P (2013) Risk factors for tuberculosis. Pulmonary medicine 2013: 1-12.
- O’Garra A, Paul S Redford, Finlay W McNab, Chloe I Bloom, Robert J Wilkinson, et al. (2013) The immune response in Annual review of immunology 31: 475-527.
- Rieder H, JM Watson, MC Raviglione, M Forssbohm, GB Migliori, et (1996) Surveillance of tuberculosis in Europe. Working Group of the World Health Organization (WHO) and the European Region of the International Union Against Tuberculosis and Lung Disease (IUATLD) for uniform reporting on tuberculosis cases. European Respiratory Journal 9: 1097-1104.
- Scordo JM (2016) Alveolar epithelial cells in Mycobacterium tuberculosis infection: active players or innocent bystanders. Journal of innate immunity 8: 3-14.
- Shingadia D, Novelli V (2003) Diagnosis and treatment of tuberculosis in children. The Lancet infectious diseases 3: 624-632.
- Yee D, Chantal Valiquette, Marthe Pelletier, Isabelle Parisien, Isabelle Rocher, et al. (2003) Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. American journal of respiratory and critical care medicine 167: 1472-1477.
- Ali H (2019) Knowledge, attitude and practice regarding tuberculosis management among final year students of two medical colleges of Pakistan Journal of Chest Medicine 25: 166-180.
- Ali J (1996) Hepatotoxic effects of tuberculosis therapy: a practical approach to a tricky management Postgraduate medicine 99: 217-236.
- Koju D (2005) Occurrence of side effects from anti- tuberculosis drugs in urban Nepalese population under DOTS Kathmandu University J Sci Eng Technol 1: 1-9.
- Orme IM, Basaraba RJ (2014) The formation of the granuloma in tuberculosis Seminars in immunology, Elsevier 26: 601-609.
- Tiwari D, Martineau AR (2023) Inflammation-mediated tissue damage in pulmonary tuberculosis and host-directed therapeutic Seminars in Immunology Elsevier 65: 1-16.
- Gurpinar E, Musal B, Aksakoglu G, Ucku R (2005) Comparison of knowledge scores of medical students in problem-based learning and traditional curriculum on public health BMC Medical Education 5: 1-7.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N (2010) Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet 376: 1923-1958.
- Nath LM, Narain JP (2002) The role of medical schools in Tuberculosis control. https://apps.who.int/iris/bitstream/handle/10665/205996/B3438.pdf?sequence=1&isAllowed=y

