Economic Impact of Health Intervention by Telemedicine during Covid 19 Pandemic at Nicaragua, June – July 2020
© 2021 Francisco Medrano, Patricia Castro, Jose Antonio Vásquez, Américo Gámez, Anely Pérez, et al, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
SARS-CoV-2 its infectious diseases was named coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) a really pandemic.
The first report on prevalence of SARS-Cov2 at Nicaragua, showed the first cases March 2020 and during the months of June and July began exponential growth period.
The telemedicine can provide rapid access, efficient and immediately available person. This approach has been explored most fully in the context of Covid 19 stroke. The estimates of intervention costs are really challenge, particularly for low- and middle-income countries. Create a health strategy during a health emergency with the lowest cost investment but great population health impact are the primary objective. The gold of this study is decide the economic impact, through of the cost benefit of medical advice through mobile phone during the COVID-19 pandemia , as health strategy at Nicaragua.
Methods
A cost-minimization analysis was carried out, during two months after the use of telemedicine as health intervention face to Covid 19 at Nicaragua. A sensitivity analysis was carried out increasing the baseline of telemedicine by users.
We have reviewed the file records of 5,712 mobile phone call as Interactive Voice Response (IVR) service the economic impact of this health intervention was decided the Cost benefit through of the cost efficient of this.
Direct Costs
Administrative resource, domestic cost to physician payments,. Cost of medical training, cost of mobile phone equipment and service. Estimated Costs for face to face medical care vs medical advice through telemedicine. Publicity Cost. The unit price: International Dollar ($). The cost estimate is based local market price. The cost of face to face medical care vs use of telemedicine, identified as social savings.
Results
A total of 5,712 service of telemedicine were registered during June and July 2020. The number of visits weekly to telemedicine: June- week # 1: 1008 Week #2: 1289 /Week #3: 987/ Week #4 : 923 July-week # 1:439 / Week #2: 371/ Week #3: 365/ Week #4: 330 The Cost of administrative resources: $3,000.00 (plan, organize, execute, and monitor team) The Domestic cost to physician payments: $2,000.00 ( 4physicians to medical advice by telemedicine) The Cost of medical training to medical advice: $ 706.00 (medical training about COVID 19 using WHO guidelines) The Cost of mobile phone equipment and service: $ 640.00 (mobile phone equipment and network internet service) The Publicity Cost: $ 1,000.00 (publicity of telemedicine strategy for radio) Total Cost to health intervention by telemedicine: $ 7,346.00 Estimated cost in the local market for 5,712 face to face medical attention: Low price: $ 57,120.00 Median price: $ 66,259.20 Highest price: $ 85,680.00 The Social Saving got in Public Health with economic impact: between $ 49,774.00 - $ 78,334.00
Conclusion
During the months of June and July 2020 were the highest peak of Covid 19 pandemic at Nicaragua. This permitted to develop a quick health strategy of low cost but large health improvement to vulnerable population. Making use of technological development and adequate medical training permitted wide coverage, indirect decrease in cost incurred by the patients and his family, helping to avoid the collapse of hospital emergency and significantly reducing the economic cost that would have been obtained if the medical attention were in person.
Introduction
In December 2019, an increasing number of cases of patients with pneumonia of unknown etiology emerged in Wuhan, China [1]. SARS-CoV-2 its infectious diseases was named coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) [2]. With its rapid spread, the virus has extended to most parts of China and whole world, a really pandemic according WHO [3-4].
The first confirmed case of coronavirus disease (COVID-19) in Nicaragua was reported March 2020 [5]. Nicaragua made up of 15 departments and two autonomous regions. Nicaragua is part of undeveloped countries with low incomes [6].
Health intervention includes any use of resources aimed at improving health outcomes be they preventive, promotive, curative, rehabilitative or palliative. It includes clinical care and public health programs and strategies.
The WHO made a guideline about to use the digital technology intervention in the health field. The mobile phone uses by the health worker in general to allow them to offer more tasks and reach more people and work more efficiently; too find treatment algorithms on digital devices useful and reassuring because they guide and simplify deliver care, what’s more, may use their mobile devices to toast information and advice online [7].
After the Covid 19 pandemic as a true health emergency, the WHO and the PHAO find an excellent opportunity to use medical advice through telemedicine as health tool against it [8].
Several international experience of the use of this strategy are found in the medical literature. Hollander and Brendan reported that the telemedicine can provide rapid access to subspecialists who aren’t immediately available person. This approach has been explored most fully in the context of Covid 19 stroke [9].
Telemedicine connects the convenience, low cost, and ready accessibility of health- related information and communication using the Internet and associated technologies. Telemedicine during the coronavirus epidemic has been the doctors’ first line of defense to slow the spread of the coronavirus, keeping social distancing and providing services by phone or videoconferencing for mild to focus personal care and limited supplies to the most urgent cases [10]
Emergency Telemedicine Consultation System, has demonstrated substantial benefits in terms of the effectiveness of consultations and remote patient monitoring, multidisciplinary care, and prevention education and training. This facilitates the avoidance of direct physical contact, thus reducing the risk of exposure to respiratory secretions and preventing the potential transmission of infection to physicians and nurses [11].
Estimating the costs of health interventions is important to policymakers for a number of reasons including the fact that the results can be used as a component in the assessment and improvement of the performance of their health systems [12].
The estimates of intervention costs are really challenge to some countries, very few countries are able to estimate these; particularly for low- and middle-income countries where the majority of the world’s poor live, there has been little progress towards the goal of providing affordable and timely information on the costs and effects of a wide array of interventions to inform policy [13].
Create a health strategy during a health emergency with the lowest cost investment but great population health impact are the primary objective. The Covid 19 pandemic permitted to develop a emergency health strategy, through of develop technology of the mobile cell phone that used to medical advice about Covid 19.
The PAHO and Inter-American Development Bank created a tool in the face of the Covid 19 pandemic. This tool has been designed to help health institutions assess their level of maturity to offer telemedicine services. The Central American Health Informatics Network, RECAINSA PAHO Information Systems for Health (IS4H) network of experts, contributed to the regional implantation of this strategy [14].
Medrano et al. presented their expertise during Covid 19 pandemic at Nicaragua, using telemedicine to medical advice through mobile phone with successful result to vulnerable people [15].
Every time that an health interventions is carried out, it is necessary to use financial resources, which are increasing limited in developing countries. Implement high cost strategy with poor results in health benefits to the population it is a really tragedy in public health in the cost benefits evaluation. Knowing the economic impact of the health strategy will allow the develop of health police that make the difference in achieving more efficient health benefits at low cost.
The gold of this study is decide the economic impact, through of the cost benefit of medical advice through mobile phone during the COVID-19 pandemia, as health strategy at Nicaragua.
Methods
Study Type: A cost-minimization analysis was carried out, during two months after the use of telemedicine as health intervention face to Covid 19 at Nicaragua.
We have reviewed the file records of 5,712 mobile phone call as Interactive Voice Response (IVR) service , using mobile phone as stablished by Derenzi and Borriello The economic impact of this health intervention was decided the Cost benefit through of the cost efficient of this [16].
Direct Costs
Administrative Resources: Human Resources to organizing, planning, implement and executive the health strategy, Domestic cost to physician payments: payments to professional service according local market. Cost of medical training to medical advice: payments by period to medical training about Covid 19 disease.
Cost of Mobile Phone Equipments and Service: payments by cost of mobile phone equipments, network and Internet service. Estimated Costs for face to face medical care vs medical advice through telemedicine.
Publicity Cost: payments by radio publicity about health strategy according Baltussen and Adam [17].
The Unit Price: International Dollar ($) according to Mirrlees JA. Project. The cost estimate is based local market price [18].
The cost of face to face medical care vs use of telemedicine, identified as societal savings (distinguishing between those of the healthcare system and of the users) from the use of telemedicine in comparison to usual care.
Indirect patients costs were not included
Cost Assessment: All resources consumed during health intervention.
Detailed listing of quantities and prices used in the analysis [19- 20].
A sensitivity analysis was carried out increasing the baseline for use of telemedicine by user.
Personnel time allocated is used in the start-up and post start-up periods is expressed in person-months. The results presented in table using Excel office 2010.
Results
The strategy of medical advice using mobile phone call, (interactive voice response), during two months (June and July 2020) due Covid 19 pandemic at Nicaragua. The number of visits weekly to telemedicine with an increasing the baseline by users as show the graphics #1
The service message system (SMS) was added in July month, a modality used by visitors , with lower prices.
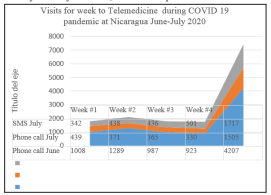
Graphic #1 Visits for week to Telemedicine during COVID 19 pandemic at Nicaragua June-July 2020 SMS (service message system)
Cost of Administrative Resources
| Human Resources | Person | Unit | Unit cost | Period (Months ) | Total Cost $ | 25% Local Market price |
|---|---|---|---|---|---|---|
| Director | 1 | 1 | $250.00 | 2 | $1000.00 | $2000.0 |
| Co-Director | 1 | 1 | $250.00 | 2 | $1000.00 | $2000.0 |
| Supervisor | 1 | 1 | $250.00 | 2 | $1000.00 | $2000.0 |
| Administrative Cost | 3 | $3000.00 |
Domestic Cost to Physician Payments
| Human Resources | Person | Unit | Unit cost | Period (Months ) | Total Cost | 50% working day / local market price |
|---|---|---|---|---|---|---|
| Physician 1 | 1 | 1 | $250.00 | 2 | $500.00 | $500.0 |
| Physician 2 | 1 | 1 | $250.00 | 2 | $500.00 | $500.0 |
| Physician 3 | 1 | 1 | $250.00 | 2 | $500.00 | $500.0 |
| Physician 4 | 1 | 1 | $250.00 | 2 | $500.00 | $500.0 |
| Physician payments | 4 | $250.00 | $2,000.00 |
Cost of Medical Training to Medical Advice
| Human Resources | Curse | Unit | Unit cost | Time | Total Cost | |
|---|---|---|---|---|---|---|
| Course management | One curse | 7 | $50.00 | One day | $350.00 | 3 curses online (8hours) |
| Personal time | One day | 7 | $42.87 | One time | $300.00 | Local market price |
| Internet network / PC use | One day | 7 | $ 8.00 | One time | $ 56.00 | Cost local price $2.00 |
| Medical training Covid 19 | $706.00 |
Cost of Mobile Phone Equipment and Service
| Human Resources | Unit | Unit cost | Total | Period service | Total Cost |
|---|---|---|---|---|---|
| Mobile Phone | 4 | $120.00 | $480.00 | 2 months | $480.00 |
| Internet Network | 4 | $ 20.00 | $ 80.00 | 2 months | $160.00 |
| Total mobile phone service | $640.00 |
Estimated Cost in the Local Market for 5,712 Face to Face Medical Attention
| Cost for Call | Unit cost | Total Cost | Period service |
|---|---|---|---|
| Low price local market | $10.00 | $57,120.00 | 2 Months |
| Median price Local market | $11.60 | $66,259.20 | 2 Months |
| Highest price Local market | $15.00 | $85,680.00 | 2 Months |
Total Cost of Telemedicine Health Intervention during Covid 19 Pandemic at Nicaragua June - July 2020
| Cost of administrative resources | $3,000.00 |
| Domestic cost to physician payments | $2,000.00 |
| Cost of medical training to medical advice | $706.00 |
| Cost of mobil phone equipment and service | $640.00 |
| Publicity Cost | $1,000.00 |
| Total Cost by Intervention | $7,346.00 |
| Total cost of telemedicine as Health intervention during Covid 19 pandemic for two months | Estimated cost in the local market for 5,712 face to face medical attention | Social Saving in Public Health with economic impact |
|---|---|---|
| $7,346.00 | Low price $57,120.00 | $ 49,774.00 |
| $7,346.00 | Median Price $66, 259.20 | $ 58,913.20 |
| $7,346.00 | Highest price $85,680.00 | $ 78,334.00 |
Discussion
World Health Organization (WHO) declared SarCov2 a real Pandemic, divers ministries of health of several countries developed health intervention as strategy to reduce the health impact in theirs citizens. Countries have experienced the COVID-19 pandemic under various circumstances and have adopted a variety of policy responses [21].
Strong public health measures and surveillance capacity are essential to prepare, prevent, detect and respond to health emergencies. WHO is examining the relationship between COVID-19 data and self-reported country readiness measured by International Health Regulations (IHR) capacity and health emergency preparedness to understand the weakness of current public health system against public health events and risks, to assess and close the gaps to reduce the risk of future pandemics [22].
A nation’s preparedness to respond to the COVID-19 pandemic depends to a large extent on the healthcare system capacity, but also on the abilities of institutions to effectively maintain essential public services, provide a social safety net for most vulnerable, prop up the economy, and mobilize collective action in all segments of the society. Every society is vulnerable to shocks and adversities, but some suffer far less harm and recover more quickly than others. Countries at lower level of human development are at a higher risk when crises strike [23].
Every time it show up a health emergency, health strategy
arise to reduce the impact of it on the most vulnerable population. Due to technological development of last decade, several health care platforms have surged as new tools to provide healthcare,( mHealth, eHealth ) principally vulnerable people as low incomes countries [24]. There are lots research realized principally at low income countries taken advantage mobile phone technology to implement various programs in health field [25-26]. We consider reproducing these examples in our country, hit by pandemic Covid 19; It would be an excellent alternative as a strategy due to the health emergency.
The first report on prevalence of SARS-Cov2 at Nicaragua, showed that during the months of June and July 2020 began five week into exponential growth period [27]. The result published by Huette et al, coincides that during the period in which the telemedicine strategy began after exponentially growth reflected in our work after the number of visits per user every week, an element that allowed us to evaluate the efficiency of the strategy. Our paper allow us to compare that through telemedicine were able to efficiently provide medical attention, similar to face to face medical attention. With this strategy we reduced the cost of patients due to not charging for care, avoid transportation and mobilization cost to the emergency units of hospital, we avoid the collapse of these by reducing the arrival of patients.
The Covid 19 pandemic at Nicaragua permitted to implement a health intervention using advantage mobile phone technology, following the recommendation by WHO in this filed and taking the experience in health strategies of the other countries [28-30]. Innumerable benefits in the field of health has shown telemedicine, not only in terms of care , data collection, follow up chronic patients , but also in the economic advantage in public health [31-33].
Several researches showed that the patients with Covid-19 with mild symptoms could be treated at home with medical advice and symptomatic treatment [34-36].
This behavior of Covid 19 provided an excellent opportunity for us to efficiently attend to patients, advice family member to care for them, identify those at greatest risk early and when to go to the health United. The analysis of the benefits in our intervention is translated into avoiding the risk of exposure and contagious to others members of the family, the unnecessary mobilization of health units with reducing exposure for health care workers and other patients. The economic impact of telemedicine have been demonstrated in several trials, allowing significant social saving for citizens and health public system [37]. The benefits achieved in our paper are similar to those obtained in others institutions at USA that used telemedicine before the Covid 19 Pandemic [38, 39].
To select a health strategy, the evaluation of the cost of the intervention and the health benefits achieve must be used. The interpretation of results is only straightforward in cases where the intervention produces more health benefits at lower cost in comparison with current practice, in which case the intervention should always be chosen. Using this scoop, ours trial take two fundamental elements: a quick and simple intervention of great benefits to the community and low cost. The results of this type of strategy are more and more efficient, it might suggest a new intervention.
Carry out health intervention always is necessary have financial resources that even develop country present somehow limitation, even more in undeveloped countries as Nicaragua [40].
The health intervention represent a real challenge , from planing, the identification of costs, the selection of the target people, the use of the appropriate technologic , among others technical aspects , to be effective the health benefit that is intended.
Several researchers have demonstrated health intervention with few achieve and high cost . Health economics literature provides ample evidence for existing inefficiencies in health. Economic appraisal seeks to improve efficiency by guiding policy-makers in how scarce resources can be used to derive the greatest possible social benefit [41].
The knowledge of the cost benefits of health intervention allows planning health budget between interventions in such a way as to maximize health in a society. The development of valuational measures of outcomes of health care treatments and programs, these outcome measures are designed to guide health policy and so must be able to be applied to substantial numbers of persons, including across or even between whole societies [42]. Our results showed that an adequate planning of the strategy against COVID 19 allowed to elaborate budget to execute it correctly and efficiently with the expected social coverage.
Under the principle of reducing intervention cost, our trial considered only administrative cost, use of equipment and Internet network service and publicity cost. This study calculated the cost, adjusting to local market price, as suggestion WHO and classifying only administrative. This paper only quantifies the cost for publicity of the strategy through the radio, we know the other cost to consider: Media inputs television time, leaflets or posters are provided in terms of their unit of measurement, (size of newspaper advertising) but those increase the intervention cost
Globally, more than 93% of the world’s population is covered by mobile phone networks, and more than 87% of people living in the developing world are mobile phone subscribers [43]. The development of the telecommunications in the health field has broken various barriers , however have arisen new problems that limit effective access to these benefits as network connectivity, access to electricity, system integration and usability of the device, and concerns about data confidentiality, the cost of call [44]. The cost to enable available phone, available hours to phone line, number of available phone line, the trainer of health workers, are some aspects that influence the number of call .Lee and Chang reported theirs expertise at Korea [45].
When we treated to reduce the intervention cost, one barrier to overcome is the equipment mobile phone cost. The smart mobile phone with high technology are very expensive compared with others, however, mobile phone with cheeper price, allowed adequate medical advice to target people during COVID 19 pandemic , to reach the golds of health intervention.
We had a small group dedicated to organizing, planning and executing the strategy, taking the local market referral cost. The cost of training medical personal have been necessary in view of training in a new disease. Some consider that this variable should not be included, prior medical knowledge, howeve , when the appearance of this new entity, the WHO made various training courses available free of charge, allowing us to decrease our intervention const, only assuming the cost generated during training time as reflected this study
Other point to evaluate the economic impact of an health intervention is the COVERAGE LEVELS. This could involve regional place, remote area even international coverage as achieved in our study. The greater coverage in the urban area, distant place and even some user outside the country, reflecting the scope of telemedicine during health emergency. This item can constitute a substantial component of costs and should not be ignored in the economic evaluation of health interventions even adapt the regional estimates to their local setting to make the results more relevant for local decision makers [46-48]. Finally, when comparing the telemedicine strategy versus face to face medical care, the social saving generated, it is very significant, in our results as other papers.
The importance of cost benefit study is to know the efficiency of the health intervention, especially at low expenditure levels. These findings can in part be explained by variation in factors outside of health systems, such as the education level of the population. However, a further part can be explained by the fact that some systems devote resources to expensive interventions with small effects on population health, while at the same time low cost interventions which would result in relatively large health improvements are not fully implemented or even ignored as this trial [49].
Conclusion
During the months of June and July 2020 were the highest peak of Covid 19 pandemic at Nicaragua. This permitted to develop a quick health strategy of low cost but large health improvement to vulnerable population. Making use of technological development and adequate medical training permitted wide coverage, indirect decrease in cost incurred by the patients and his family, helping to avoid the collapse of hospital emergency and significantly reducing the economic cost that would have been obtained if the medical attention were in person.
References
- Zhu N, Zhang D, Wang W (2020) A novel coronavirus from patients with pneumonia in China. 382:
- World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. 2020; Available at: https://www.who. int/emergencies/diseases/ novel-coronavirus-2019/technical-guidance/ naming-thecoronavirus-disease-(covid-2019)-and-the-virus-that-causesit
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA 323:
- Country & technical guidance-coronavirus disease (COVID-19) [website]. Geneva: World Health Organization; 2020
- Health Ministery from Nicaragua
- PHAO. Salud de Las Ame?ricas.Nicaragua, 2017. En https:// www.paho.org/salud- en-las-americas-2017/?post_t_ es=nicaragua&lang=es
- WHO guideline recommendations on digital interventions for health system 2019) 8- WHO/ PHAO: COVID-19 AND TELEMEDICINE Tool for assessing the maturity level of health institutions to implement telemedicine Version 3 2020
- Judd Hollander, Brendan G (2020) Virtually Perfect? Telemedicine for Covid-19. The New England Journal of Medicine 382:
- Josep Vidal-Alaballa,b, Ruthy Acosta-Roja (2020) Telemedicine in the face of the COVID-19 pandemic. Aten Primaria. 52:
- Yunkai Zhai1, Yichuan Wang. National Telemedicine Center of China, From Isolation to Coordination: How Can Telemedicine Help Combat the COVID-19 Outbreak?. https:// full.pdf+html
- Benjamin Johns, Rob Baltussen, Raymond Hutubessy (2003) Programme costs in the economic evaluation of health interventions Cost Effectiveness and Resource Allocation 1:
- T Tan-torres edejer R, Baltussen t, Adam R, Hutubessy A, et al. Making choices in health: who guide to cost-effectiveness
- PHAO-WHO: Conference: From the evolution of Information Systems for Health (IS4H) to the Digital Transformation of the Health Sector. February
- F Medrano, P Castro (2020) Medical Advice Through mobile Phone During the COVID-19 Pandemia, June - July 2020 at Nicaragua. Journal of Virology Research & Reports 1:
- Derenzi B, Borriello G, Jackson J, Kumar VS, Parikh TS, Virk P, et al. (2011) Mobile phone tools for field-based health care workers in low-income countries. Mt Sinai J Med 78:
- Baltussen RM, Adam T, Tan Torres T, Hutubessy RC, Acharya A. Generalized Cost-Effectiveness Analysis: A Geneva, World Health Organization, Global Programme on Evidence for Health Policy
- Mirrlees JA (1974) Project appraisal and planning for developing countries. London: Heinemann Educational
- Mishan EJ (1982) Cost-benefit analysis. 3rd ed. London: George Allen & Unwin (Publishers)
- Peter Berman (1989) Cost efficient in primary health care: studies of health facility in Indonesia. Health and Policy Planning 4:
- Kristine A. Moore and others. “The future of the COVID-19 pandemic: Lessons learned from pandemic influenza”, Center for Infectious Disease Research and Policy (CIDRAP), University of Minnesota, 30 April 2020, cidrap.umn.edu/sites/
- Nirmal Kandel, Stella Chungong (2020) Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. The Lancet 395:
- UNDP (2019) Human development report 2019. Beyond income, beyond averages, beyond today: Inequalities in human development in the 21st century.
- Alain B Labrique, Lavanya Vasudevan, Erica Kochi, Robert Fabricant, Garrett Mehl (2013) mHealth innovations as health system strengthening tools: 12 common applications and a visual framework, Global Health: Science and Practice 1:
- Gibson D, Pereira A, Farrenkopf B, Pariyo G, Labrique A, et al. (2017) Mobile phone surveys for collecting populationlevel estimates in low- and middle-income countries: a literature review. J Med Internet Res 19:
- Du X, Wang W, van Velthoven MH, Chen L, Scherpbier RW, et al. (2013) mHealth series: text messaging data collection of infant and young child feeding practice in rural China - a feasibility study. J Glob Health 3:
- Huete JA, Quant C (2021) PLOS ONE: First report on prevalence of SARS-COV-2 infection among health care workers in Nicaragua- 27:
- (2019) WHO guideline recommendations on digital interventions for health system strengthening
- Abigail R Greenleaf, Saifuddin Ahmed, Caroline Moreau a, Georges Guiella, Yoonjoung Choi (2019) Cell phone ownership and modern contraceptive use in Burkina Faso: implications for research and interventions using mobile technology. Contraception 99:
- Moura E, Claro RM, Bernal R, Ribeiro J, Malta D, et (2011) A feasibility study of cell phone and landline phone interviews for monitoring of risk and protection factors for chronic diseases in Brazil. Cad Sau?de Pu?blica 27:
- Delgoshaei B, Mobinizadeh M, Mojdekar R, Afzal E, Arabloo J, et al. (2017) Telemedicine: A systematic review of economic evaluations. Med. J. Islam. Repub. Iran 31:
- Natafgi N, Shane DM, Ullrich F, MacKinney AC, Bell A, et al. (2018) Using tele-emergency to avoid patient transfers in rural emergency departments: An assessment of costs and benefits. J. Telemed 24:
- Vidal-Alaball J, Alamo-Junquera D, Lo?pez-Aguila S, Garci?aAlte?s A (2015) Evaluation of the impact of tele-dermatology in decreasing the waiting list in the Bages region Aten. Primaria 47:
- WHO. Home care for patients with COVID-19 presenting with mild symptoms and management of their Geneva: World Health Organization;
- WHO. The use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients with COVID-19. Geneva: World Health Organization;
- Greenhalgh T, Koh GCH, Car J (2020) Covid-19: a remote assessment in primary care. BMJ 368:
- Lacktman NM, Acosta JN, Levine SJ. 50-State survey of telehealth commercial payer statutes. Foley.com/Telemedicine, December 2019 https://w w / media/files/insights/health-care-law-today/ 19mc21486- 50state-survey-of-telehealth - commercial.pdf
- Langabeer JR II, Gonzalez M, Alqusairi D (2016) Telehealthenabled emergency med- ical services program reduces ambulance transport to urban emergency departments. West J Emerg Med 17:
- Lurie N, Carr BG (2018) The role of telehealth in the medical response to disasters. JAMA Intern Med 178:
- Rodríguez Artalejo (2004) El medico ante la evaluacion economica. Editorial . Med Clin ( Barc) 122 :
- Raymond CW, Hutubessy Rob, M PM Baltussen, Tessa Tan-Torres Edejer, David B (2002) Evans Applied Health Economics and Health Policy © copyright Open Mind Journals Limited. 1:
- Brock DW (1992) Quality of life measures in health care and medical ethics. In: Sen A, Nussbaum M, eds.The quality of life. Oxford: Oxford University
- (2012) World Bank and International Telecommunication Union. The little data book on information and communication technology Washington, DC: The World Bank 246
- Greenleaf AR, Gibson DG, Khattar C, Labrique AB, Pariyo GW (2017) Building the evi- dence base for remote data collection in low- and middle-income countries: comparing reliability and accuracy across survey modalities. J Med Internet Res 19:
- Lee Y, Chang H (2012) Ubiquitous health in Korea: progress, barriers, and prospects. Healthc Inform Res 18:
- Creese A, Parker D (1994) Cost analysis in primary health care: A training manual for programme managers. Geneva: World Health Organization
- Drummond MF, O’Brien BJ, Stoddart GL, Torrance GW (1997) Methods for the economic evaluation of health care programmes. 2nd ed. Oxford: Oxford University Press 47. Khan MM, Ali D, Ferdousy Z, Al Mamun A (2001) A cost-minimization approach to planning the geographical distribution of health facilities. Health Policy and Planning 16:
- Evans DB, Tandon A, Murray CJ, Lauer JA (2001) Comparative efficiency of national health systems: cross national econometric analysis. BMJ 323:
- Josep Ma. Argimon, Josep Jimenez V. Mètodos de investigacion clínica. 2013- 4ta Edicion . www.elsevier.com/books/metodos-de-investigacion-clinicay-epidemiologica/argimon-pallas/978-84-9113-007-9.

