Author(s): <p>Joana Lopes Ferreira*, Inês Ângelo, Joaquim Peixoto and Martinho Fernandes</p>
Cytomegalovirus (CMV) pneumonia is a viral infection of the lungs that affects immunocompromised patients. Although it is a rare opportunistic infection in the setting of HIV (Human Immunodeficiency Virus)-infection, in most of these patients, CMV pneumonia is believed to be caused by reactivation secondary to severe immunocompromise.
In this article we present a case of a patient with poor immunological status that developed clinical features of respiratory infection. Initially pulmonary pneumocystis was diagnosed and treated accordingly. After presenting clinical worsening, other diagnostic hypotheses were placed and broad-spectrum antibiotics and antifungal drugs were administered. However, with no clinical improvement. Facing this, a rarer opportunistic infection, cytomegalovirus (CMV) pneumonia, was considered. The diagnosis of this pathology can be difficult because of its unspecific clinical presentation and radiological findings, however it can be done by detection of positive CMV serostatus together with detection of virus DNA in blood and/or bronchoalveolar lavage samples. The treatment goal is to stop viral replication, and the first-line therapy is Ganciclovir intravenous (IV).When presenting clinical signs of infection, in HIV positive patients, immunological status should be taken into consideration, and opportunistic infections cannot be overlooked. Early diagnosis allows prompt treatment and potentially complete recovery.
Human Cytomegalovirus (HCMV, Human Herpesvirus 5) is a double-stranded DNA virus and it belongs to the β-herpesvirus family. Primary infection by CMV is usually asymptomatic as the intact immune system limits active viral replication effectively. However, CMV is capable of multiple immune evasion mechanisms and complete eradication of the virus may not be achieved.
Instead, the virus remains quiescent within endothelial cells, stem cells of the bone marrow and peripheral blood monocytes, establishing a lifelong latent infection. When the immune system is suppressed, latent CMV can reactivate and replicate rapidly. This can result in high levels of CMV viremia and infection of multiple organ systems. Among the high-risk group are patients receiving immunosuppressive medication for prevention of organ transplant rejection, infection with immune-modulating pathogens such as human immunodeficiency virus (HIV), and infection in the early life period. In HIV patients, the most common presentation of CMV infection is retinitis, although colitis, esophagitis, pneumonitis and neurological disorders can also occur.
Whereas retinal disease caused by CMV is distinctive and readily recognizable, pulmonary disease is not and it can sometimes be missed out. CMV pneumonia symptoms are nonspecific, and they include low-grade fever, shortness of breath, and dry cough. Radiographic features are also nonspecific, including patchy or diffuse ground-glass opacities, patchy consolidation, small nodular opacities, thickened bronchovascular bundles, tree-in-bud opacities, reticular opacities, and small pleural effusions. Thus, the diagnosis of suspected CMV pneumonia can be complicated. Although biopsy is the gold standard for tissue invasive disease, positive CMV serostatus together with detection of virus DNA in blood and/or bronchoalveolar lavage samples can be used to confirm CMV pneumonia. The goal of treatment is to use antiviral drugs to stop the virus from copying itself. First-line treatment for CMV disease is IV ganciclovir or its prodrug, oral valganciclovir, which acts by inhibiting viral DNA polymerase, thereby interfering Case Report 63-year-old female recently diagnosed with HIV infection, with poor immune status showing absence of CD4+ cells, was observed for the first time in an Infectious Diseases consultation. Due to presentation of respiratory symptoms, with sensation of dyspnea and productive cough, the patient was referred to the emergency department. After clinical observation and chest radiography, with evidence of interstitial, diffuse, bilateral infiltrate, the hypothesis of pulmonary pneumocystis was considered. In this context, the patient was hospitalized and started targeted therapy. Bronchoscopy with bronchoalveolar lavage confirmed the diagnosis. The patient completed 21 days of therapy with clinical improvement. During hospitalization, antiretroviral therapy was initiated. After a few days, the patient showed worsening of her clinical status, presenting with fever, dyspnea and need for supplemental oxygen. A new chest radiography was placed and it showed bilateral interstitial infiltrate with nodular areas of consolidation. Empirical broad-spectrum antibiotic therapy was started, with coverage for Gram+ and Gram-. However, there was no clinical improvement. Subsequently, antifungal coverage was added, once more, with no favorable clinical response. At last, the hypothesis of cytomegalovirus (CMV) pneumonia was considered and therapy with Ganciclovir was started. Another bronchoscopy was performed, with bronchoalveolar lavage, which would confirm the presence of CMV by Polymerase chain reaction (PCR). After therapy with Ganciclovir, clinical and radiographic improvement was observed (Figure 1.) and the patient was discharged after complete resolution of the disease.
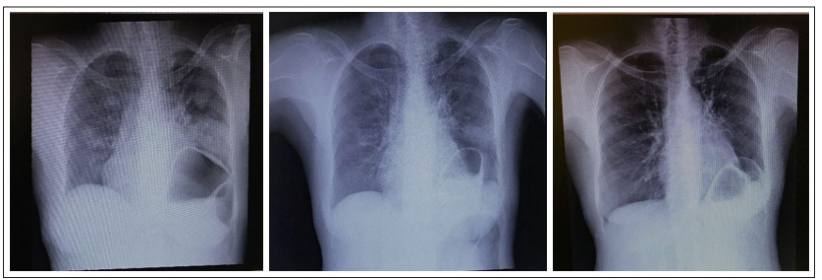
Figure 1: Radiological evolution of CMV Pneumonia treated with Ganciclovir
Opportunistic infections remain a major concern in Human Immunodeficiency Virus infected individuals as they contribute significantly to morbidity and mortality. When facing an infection in an HIV patient, it is very important to take into account not only the patient’s clinical presentation, but also his immunological situation, namely the CD4+ cell count. CMV is a very rare cause of pulmonary opportunistic infection in the setting of HIV-infection. CMV pneumonia should be carefully evaluated amongst patients with AIDS who are critically ill and not responding to treatment of other diagnosed pulmonary infections. The diagnosis of CMV pneumonia can only be made with consistent clinical, radiological, microbiological and cyto-histopathologic features. The response to therapy directed to certain pathogens is sometimes slower in immunocompromised patients, however, over-infection by other agents should not be ruled out in the absence of clinical improvement.
This case is of particular interest as it concerns two opportunistic infections of the respiratory system. In patients with CD4+ count less than 200 cells/mm3 Pneumocystis jiroveci infection is frequent and should not be overlooked in a patient with a typical respiratory and radiological pattern. CMV pneumonia, on the other hand, is relatively rare and its diagnosis can be a challenge. One should always keep in mind the possibility of viral infections such as CMV in immunocompromised patients and workup should be tailored accordingly [1-13]
