Author(s): Teresa Della Corte
Background: Lipohypertrophy (LH) is a frequent cutaneous complication in people with insulin-treated type-2 DM (IT-T2DM). Its pathogenesis is not fully known, however. Retinal and kidney microangiopathy (MIA) is also frequent in such patients, especially in case of poor metabolic control.
Aim: To assess whether specific nailfold video-capillaroscopy (NVC) patterns could be identified in MIA-affected IT-T2DM patients, thus eventually helping explain LH pathogenesis.
Methods: 50 IT-T2DM patients with LH and 50 without LH undergoing NVC were enrolled. All followed a multiple daily injection regimen and had established retinal and renal microangiopathic complications.
Results: While confirming expected MIA-related skin changes in both groups, our data failed to detect any specific NVC pattern in LH-affected patients yet showed the most severe NVC changes to be significantly associated with HbA1c values over 9%.
Conclusion: Severe NVC-assessed MIA lesions reflect longstanding poor metabolic control in IT-T2DM rather than contributing to LH pathogenesis
The prevalence of micro- and macrovascular changes characterizing chronic complications of type-2 diabetes mellitus (T2DM) increases with disease duration and poor metabolic control [1]. As T2DM proceeds, beta-cell function progressively decreases until insulin treatment gets necessary for health and even survival. Any longstanding incorrect insulin injection behavior leads to a typical skin complication named lipohypertrophy (LH), mainly due to both repeated local microtraumas and anabolic insulin effects [2, 3]. LHs are present in 38% of insulin-treated patients with T2DM on average, especially in those with micro- and macrovascular complications, and often comes with bruising (BR) [4-6]. Notoriously enough, LHs severely impair glucose control, yet, as apart from those reported above, the inner mechanisms behind their formation are not fully understood, nor are any data available on eventually occurring LH-related microvascular skin changes. Nailfold videocapillaroscopy (NVC) is a noninvasive technology widely used in T2DM to reveal skin microangiopathic lesions so far [7-12].
This preliminary retrospective study aimed to check whether insulin-treated T2DM patients with clearly evident LHs have more severe or different NCV-diagnosed microvascular changes than usual, to evaluate the need for an extensive, demanding, prospective investigation on the item.
After signing a written informed consent to anonymized data utilization for research purposes, all patients reporting to our diabetes center had their clinical and laboratory parametersrecorded in our electronic database (EDB), among which LH lesions as identified through a validated method already described by our group elsewhere [2]. Briefly, the latter consisted of a structured, standardized diagnostic technique based on inspection and palpation of all patient-reported injection sites by two specifically trained health care practitioners (HCPs), eventually confirmed by an ultrasound (US) scan, used as the reference method to precisely identify LHs in the case of lacking agreement between HCPs.
Subjects: we were able to extract 918 records by querying our EDB the following criteria: (i) BR at injection sites; (ii) a multiple daily insulin injection-based regimen at least for the last two years; (iii) well-documented microvascular complications in terms of non-proliferating retinopathy, microalbuminuria (reference value ≤20 ml/l) or grade I kidney disease (eGFR ranging 45-59 ml/ min/1.73m2), (iv) no use of antiplatelet agents or anticoagulants. We found 15% also having NVC results.
We then divided the original set of records into two subsets depending on the presence or absence of flat or protruding LHs. No reliable sample size calculation was possible due to missing literature, so we arbitrarily chose to select the first 50 records per subset according to the simple randomization method to keep on the safe side as for statistical power, and classified them into “index” and “control” groups, respectively. General characteristics of patients are summarized in Table 1.
| LH-positive T2DM | LH-free T2DM | |
|---|---|---|
| Gender M/F (%) | 40/60 | 40/60 |
| Age (years) | 61±7 | 60±8 |
| BMI (Kg/m2) | 29.4±6.2 | 30.1±5.9 |
| HbA1c (%) Range | 9.4±1.1 7.8 - 11.1 | 9.5+0.9 7.7 - 11.5 |
| Microalbuminuria mg/l (nv <20) | 96+12 | 88±18 |
| eGFR mj/min/1.73m2 | 52+8 | 56±8 |
| Diabetes duration (years) | 10±7 | 9±8 |
| Insulin treatment duration (years) | 7±2 | 7±3 |
| Daily insulin dose requirement (IU/day) | 56.5±10.2 | 42.7± 9.8 |
| Diabetes complications (%) | ||
| - Cardio/cerebrovascular Complications | 90 | 80 |
| - Lower Limb Complications | 20 | 20 |
| - Retinopathy | 100 | 100 |
| - Nephropathy | 100 | 100 |
| - Sensory-Motor Neuropathy | 100 | 90 |
| - Autonomic Neuropathy | 100 | 90 |
| Injection habits (%) | ||
| Needle reuse >3 times | 100 | - |
| Failure to rotate injection sites | 100 | - |
| Ice-cold insulin injections | 80 | - |
| Injection into LH nodules | 100 | - |
| Bruising at injection sites | 70 | - |
Nailfold Videocapillaroscopy (NVC): after patients’ acclimatization at a 24°C room-temperature for 20 minutes, a single, well trained operator blinded to clinical diagnosis used a videocapillaroscope (Videocap 25-DS Medica; Freiburg, Germany) with optical probes providing 200-fold magnification on the 4th finger of each participant’s left hand according to a standardized, validated method [8, 13]. Examined fields were: (i) capillaries in the distal nailfold row and (ii) hemorrhages close to the distal nailfold row. The following morphological features were recorded: (i) increased, regular, or reduced capillary length (reference length is 200-500 mm); (ii) ordered, comma-like, irregular, or severely deranged distribution; (iii) hairpin, tortuous, ramified, or bushy morphology; (iv) 10-30/ mm2, 8-10/mm2, or <8/mm2 density; (v) regular, enlarged, or giant loop diameter; (vi) absent, rare, or diffused hemorrhages; and (vii) normal, slow, or discontinuous flow patterns [9, 11]. Based on capillary length, distribution, morphology, density, and diameter, as well as on the presence of hemorrhages, sub-venular plexuses, capillary flow changes, and edema/exudate, a quantitative validated NVC scoring criterion allowed classification of NVC changes into a 0 to 3 range, where 0 = normal, 1 = light, 2= mild, and 3 = severe abnormalities [4, 8].
Data Analysis: statistical analysis was based on IBM SPSS Statistics 19 (IBM Co., NY). Data were presented as mean ± SD, number or %. Alterations of NVC characteristics were quantified as NVC scores [7, 11]. Differences were tested by the repeated measures analysis of variance (rANOVA) integrated by twotailed paired Student’s t-test with 95% Confidence Intervals (CI) for parametric variables and Mann-Whitney’s U test for nonparametric ones. A p<0.05 was chosen as the least acceptable level of statistical significance.
As from Table 1, 35 subjects from the IG had protruding, 15 flat LHs. All had BRs, both close to and outside LH-affected sites, as well as microalbuminuria, reduced eGFR together, and other microand macrovascular complications. The CG displayed no significant differences from the IG, as also apparent from Table1. Thirty subjects from the IG scored mild, and twenty severe at NVC as per the abovementioned classification. Similarly, twenty-nine patients scored mild and twenty-one severe in the CG. Most frequent abnormal capillary patterns involved morphology, distribution, length (<200mm), and flow. Fig.2 shows representative NVC pictures. Moreover, as seen in Table 2, a significant difference was apparent in either group between mild and severe NVC scores only in terms of HbA1c when classified as relatively- and definitelyhigh (≤ 9%, and >9%, respectively).
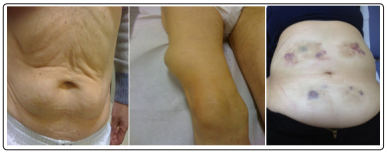
Figure 1: Left and middle panels show examples of large LH nodules; the right panel show less visible LH nodules identified by palpation and pinching maneuvers, instead, with clearly evident BRs
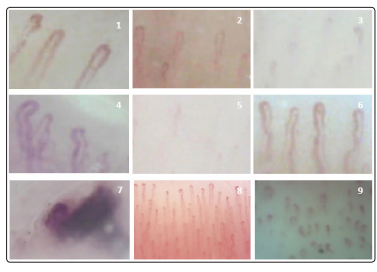
Figure 2: Characteristics of single nailfold videocapillaroscopy alterations: (1) normal patterns; (2) reduced capillary length; (3) irregular capillary distribution; (4) abnormal capillary morphology; (5) reduced capillary density; (6) enlarged capillary loop; (7) hemorrhage, as compared to a (8) wide-field view of normal capillary pattern, and (9) associated typical DM alterations (from patient n. 8).
| LH-positive T2DM | LH-free T2DM | p | |||
|---|---|---|---|---|---|
| HbA1c overall (%) |
n. 50 | 9.4±1.1 (7.8 - 11.1) |
n. 50 | 9.5+0.9 (7.7 - 11.5) |
n.s. |
| HbA1c NVC score 2 |
n. 29 | 8.2+0.7 (7.8 - 9.4) |
n. 30 | 8.4+0.8 (7.7 - 9.3 |
n.s |
| HbA1c NVC score 3 |
n.21 | 10.5+0.6 (9.4 - 11.1) |
n. 20 | 10.7+0.7 (9.5 - 11.5) |
n.s |
| p: score 2 vs score 3 |
<0.05 | <0.05 | |||
Our preliminary data came from a sample population kept at a relatively small size on purpose to check whether or not to investigate this issue further. We could confirm the NVC results obtained by others in patients with ITT2DM but failed to find any increased blood leakage at the microcapillary level despite the high BR rate at injection sites [7-12 & 14-16].
NVC is a noninvasive diagnostic method used to evaluate the
morphology, distribution, density, and blood flow of nailfold
dermal papillary capillaries, thus unraveling extremely fine
circulation abnormalities and identifying microvascular patterns
in many rheumatic diseases, particularly systemic sclerosis and
related disorders [8, 9]. Noteworthily, diabetic microangiopathy is
a frequent and often early complication, mainly involving retinal
and kidney microcirculation. Our results support those from the
few previous studies showing abnormalities in nailfold flow and
capillary morphology in patients with diabetes [13, 14]. Moreover,
NVC allowed to qualitatively and quantitatively evaluate such
changes in patients with ITT2DM, thus revealing mild and severe
alterations to cluster according to the presence of relatively- and
definitely-high HbA1c values, respectively [11, 1 2].
Actually, people with T2DM usually display specific NVC
patterns consisting of capillary dilatation, avascular zones, and
tortuous capillaries, and those with longer-duration disease and
more comorbidities show more significant microvascular damage
[16]. Capillaroscopic alterations in the IG coincided with those
reported above and expected in any patients with T2DM and
failed to show any different microhemorrhage or microvascular
abnormality rates compared to the CG.
Our study's primary limitation is the relatively limited number of subjects involved, despite the latter not impairing the ability to identify any statistically significant changes, if so ever. Nevertheless, such limitation reflected a specific choice by our group to conduct a preliminary investigation not to waste precious resources in a wide enough, yet potentially inconclusive study. Moreover, the main feature characterizing our investigation consisted of (i) the structured method used to identify IG and CG patients, i.e., the involvement of expert devoted HCPs using a validated, standardized method and (ii) the US-based discrimination between LHs and any possible lesions reflecting different skin abnormalities as needed.
In line with the literature dealing with microangiopathy in T2DM, our results witness in favor of the so-called 'diabetic capillaropathy' in longstanding IT-T2DM and of the strong relationship linking NVC abnormalities to blood glucose control and microangiopathy, with particular reference to retinal and kidney damage [12, 17].
In conclusion, our data cannot be of any help in assessing whether or not microvascular IT-T2DM changes favor insulin injection-related LH formation. However, the observed direct association between NVC scores and HbA1c levels supports the hypothesis that longstanding high glucose levels are associated with severely altered capillary features besides typical chronic disease complications [18].
We acknowledge the logistic support of Nefrocenter Research Network & Nyx, research startup, Naples, Italy. Our heartfelt thanks go to patients giving informed consent to the study and the publication of their own anonymized data and pictures.
Funding: The study did not have a sponsor/funder. None of the authors or co-workers received funding or another type of payment for this paper. No Rapid Service Fee was received by the journal for the publication of this article.
Authorship: All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions: SG and FS prepared and wrote the paper. GG, GC, LAS, and CL critically read and approved the paper. All authors checked the data collection, critically assessed the results, and approved the final text. All Collaborators critically read and approved the final text.
Disclosures: Sandro Gentile, Giuseppina Guarino, Giovanna Cuomo, Clelia Lamberti, Luisa Anna Stile and Felice Strollo have no disclosures.
Compliance with Ethics Guidelines: This study was conducted in conformance with good clinical practice standards and was performed according to the Declaration of Helsinki 1975, as subsequent amendments. It was approved by Vanvitelli University, Naples, Italy as part of a general trial on insulin-induced lipohypertrophy in type 2 diabetic subjects (Trial registrationnumber 172-11:12.2019). Written informed consent was obtainedfrom all participants before enrollment to participate in the study and to have their data and pictures published under an anonymized format . The complete list of Collaborators is available on reference n. 2.
Editorial Assistance: Special thanks are due to Members of the AMD-OSDI on Injection Technique Study Group, and to Members of Nefrocenter Research & Nyx Start-up Study Group for critical reading and approval of the manuscript. The complete list of Members of the two Study Groups is available on reference n. 2.
Data Availability: The datasets analyzed during the current study are available from the corresponding author on reasonable request.
