Author(s): Sékangué Obili G, Ossibi Ibara BR*, Potokoué Mpia NSB, Adoua Doukaga T, Itoua C, Djendja Ingoba I, Gackosso G and Iloki LH
Introduction: Vaginal candidiasis is a mycosis caused by a yeast of the genus Candida. Candida albicans was for a long time the first etiology of these mycoses. However, in recent years, an increasing involvement of non-albicans Candida species has been observed.
Objective: To describe the epidemiological and mycological aspects of vaginal candidiasis due to Candida non albicans in women who have performed an analysis of the vaginal sample in the Parasitology Mycology laboratory of the University Hospital Center of Brazzaville.
Patients, Materials And Method: This was a descriptive and analytical cross-sectional study from July to October 2019 (i.e. 3 months). It concerned all the patients received at the Parasitology-mycology and parasitic immunology laboratory of the CHUB for an analysis of the vaginal sample. The diagnosis was made after direct examination and culture of samples on Sabouraud Chloramphenicol medium with and without Actidione*. The filamentation test on calf serum and the study of the biochemical characteristics of the yeast colonies using the API candida strips from Biomérieux were carried out for each positive culture. Statistical analysis was performed using Epi-info 7.2.2.6 softwares.
Results: The frequency of Candida non albicans yeast infection was 64.7%. The median age of patients with Candida non albicans vaginal candidiasis was 35.5 years (25.0 years - 47.0 years) with extremes of 18 and 59 years old. The age group between 18 and 40 was the most represented (68.2%). These were women with secondary education (n=12 ; 54.5%), with a notion of a single sexual partner (n=17 ; 77.3%), pregnant (n=6 ; 27, 3%). In 22.7% there was poor faecal hygiene. The main reasons for taking the samples were… and the non-albicans Candida species were represented by Candida glabrata (36.4%), Candida tropicalis (18.2%), Candida krusei (13.6%), Candida famata (13.6%), Candida parapsilosis (9.1%) and Candida spp (4.6%).
Analytical Study
Conclusion: Candida non albicansremains the common fungus in our context with a predominance of Candida glabrata. Age, poor faecal hygiene could have a link with the occurrence of these fungal infections, hence the importance of good awareness and systematic research in young women.
Vaginal candidiasis is a vaginal mycosis due to the presence of a fungus of the genus Candida, of which there are several species [1-3]. It is the most common genital infection in women and affects nearly 75% of sexually active women [4-7]. While Candida albicans has long been implicated in the occurrence of vaginal candidiasis, in recent years we have seen an emergence of Candida non albicans in women of childbearing age [4, 8, 9]. Among these species, Candida glabrata was the most frequent [2, 10, 11]. Candida glabrata is part of our natural microflora and can be present in the digestive tract, mouth and genital area. Usually well controlled, or harmless, yeast can become pathological in people with weakened immune systems. For example, this includes people living with HIV, people receiving cancer treatment, and people who have had an organ transplant. Candida glabrata also has a high resistance to some antifungal drugs, which can make it difficult to treat
It would seem that poor hygiene associated with excessive consumption of antibiotics would facilitate the occurrence of this condition in women [12]. In the Congo, few studies have addressed the problem of vaginal candidiasis caused by candida non albicans, hence the interest of this work, which aimed to determine the frequency of vaginal candidiasis caused by candida non albicans, to identify the types of responsible species and to research the factors associated with the CHU of Brazzaville
This was a descriptive cross-sectional study that was held from July 15 to October 31, 2019 in the Parasitology-Mycology laboratory of the CHUB. All patients who came to the sampling room during the study period for a vaginal sample analysis were included after completing a consent form. Data related to sociodemographic variables (age, profession, level of education), medical and gynecological history, symptoms and mycological analysis were collected from a survey sheet.
Each sample collected was the subject of a measurement of the vaginal pH using a colorimetric strip, a macroscopic examination to assess the appearance of the leucorrhea and the vaginal mucosa. A direct microscopic examination in search of yeasts and a culture on Sabouraud chloramphenicol medium were carried out. The culture media were incubated at 37° C. in an aerobic atmosphere for 24 hours. The filamentation test in calf serum and Biomérieux’s Api Candida type identification biochemical galleries were used to determine the Candida species.
The data collected was analyzed using the Epi-info 7.2.2.6 softwares. The calculations were made by the frequencies for the qualitative data and the parameters of central tendency and dispersion for the quantitative variables.
Of the 152 samples, the frequency of Candida non albicans candidiasis was 64.7% (n=22) while that of Candida albicans was 35.3% (12 patients). The median age of patients with vaginal candidiasis was 35.5 years (25.0 years ; 47.0 years) with extremes of 18 and 59 years. 68.2% of the patients belonged to the age group of [18-40 years]. They were unemployed in more than half of the cases (n=13; 59.1%). The socio-demographic characteristics of the patients are represented by Table I.
Table II shows the medical and gyneco-obstetrical history of patients with vaginal candidiasis caused by Candida non albicans. None of the patients had taken hormonal treatment and 77.3% of the patients had only one sexual partner, of whom 27.3% were pregnant. Information related to the notion of hygiene is given in Table III. Candida glabrata was the most represented species 36.4%, followed by Candida tropicalis : 18.2% (Figure 1).
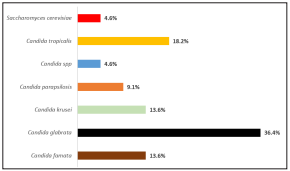
Figure 1: Distribution Of The Different Species Of Candida Non Albicans
Table I: Epidemiological Aspects Of Women With Vaginal Candidiasis Caused By Candida Non Albicans
| Variables | Workforce (N) | Percentage (%) |
| Age range | ||
| [18 to 40 years old] | 15 | 68.2 |
| [41 to 59 years old] | 7 | 31.8 |
| Occupation | ||
| Without | 13 | 59.1 |
| With | 9 | 40.9 |
| Educational level | ||
| Secondary | 12 | 54.5 |
| University | 10 | 45.5 |
| Marital status | ||
| Single | 13 | 59.1 |
| Bride | 9 | 40.9 |
Table II: Medical And Gyneco-Obstetrical History Of Patients With Candidiasis Vaginal Candida Albicans From July 15 To October 31, 2019
| Variables | Workforce (N) | Percentage (%) |
| Concept of chronic pathology | ||
| Diabetes | 3 | 13.6 |
| Hypertension | 0 | 0 |
| Cancer | 0 | 0 |
| HIV | 0 | 0 |
| Concept of long-term hormone treatment | ||
| Yes | 0 | 0 |
| Nope | 22 | 100 |
| Notions of taking antibiotics | ||
| Yes | 1 | 4.6 |
| Nope | 21 | 95.4 |
| Concept of taking corticosteroids | ||
| Yes | 1 | 4.6 |
| Nope | 21 | 95.4 |
| Virginity concept | ||
| Yes | 2 | 9.1 |
| Nope | 20 | 90.9 |
| Partner | ||
| Unique | 17 | 77.3 |
| Multiple | 0 | 0 |
| Without | 5 | 22.7 |
| Abortion concept | ||
| Yes | 6 | 27.3 |
| Nope | 16 | 72.7 |
| Gynecological disease concept | ||
| Yes | 2 | 9.1 |
| Nope | 20 | 90.9 |
| Pregnancy concept | ||
| Yes | 6 | 27.3 |
| Nope | 16 | 72.7 |
| Treatment for candidiasis | ||
| Yes | 3 | 13.6 |
| Nope | 19 | 86.4 |
| Condom use | ||
| Yes | 4 | 18.2 |
| Nope | 18 | 81.8 |
Table III: Hygienic Characteristics Of Patients With Vaginal Candidiasis Candida Non Albicans
| Variables | Workforce (N) | Percentage (%) |
| Intimate baths | ||
| Yes | 7 | 31.8 |
| Nope | 15 | 68.2 |
| Communal use of bath towels | ||
| Yes | 2 | 9.1 |
| Nope | 20 | 90.9 |
| Shared wearing of underwear | ||
| Yes | 1 | 4.5 |
| Nope | 21 | 95.4 |
| Wearing synthetic underwear | ||
| Yes | 4 | 18.2 |
| Nope | 18 | 81.8 |
| Wearing tight clothes | ||
| Yes | 7 | 31.8 |
| Nope | 15 | 68.2 |
| Cleaning mode | ||
| Back and forth | 17 | 77.3 |
| Back forward | 0 | 0 |
| Both | 5 | 22.7 |
The prevalence of vaginal candidiasis due to Candida non albicans is high in our series as reported in the literature. Indeed, alongside Candida albicans, several studies have already reported the possible emergence of non-albicans candida in the pathogenesis of vaginal candidiasis in women of childbearing age [10, 13- 16]. These data corroborate those obtained in the sub-region and elsewhere [17-20]. Hormonal treatment could have a link with the occurrence of non-albicans candidiasis. This finding similar to that made in India by Tamsikar is no longer a new fact since the same study had made it possible to highlight their role in modifying the balance of vaginal Candida species that hormones have. [16]. The same is true in Burkina Faso where Sangaré and collaborators found a greater involvement of Candida non albicans compared to Candida albicans in a population of pregnant women [21]. Alongside these authors who obtained these results of the predominance of Candida albicans in particular populations, there are, as in our case, authors who found a predominance of Candida non albicans. This is the case of Kalaiarasan K and collaborators who obtained a prevalence of vaginal candidiasis due to nonalbicans candida, in particular Candida glabrata [22]. When the existence of a hormonal disturbance is proven, the involvement of non-albicans Candida species compared to Candida albicans can be explained. However when no cause can explain it, only the search for risk factors can enable us to provide an appropriate response to each case. Our results could, however, be explained either by a lack of knowledge of the hormonal disturbances in the majority of the women who were retained in the study, or by habits not recognized as dangerous by these women.
Candida glabrata was the most common species found in our study. This was also found in several studies, whether in studies where Candida albicans was the majority species or those where Candida non albicans was. In general, this species is isolated in cases of complicated candidiasis or recurrent vaginal candidiasis. However, it should be noted that there is variability in the prevalence of non-albicans Candida species in different studies. Thus, some authors have predominantly found [23-27]. Despite this diversity in prevalence, overall it appears that C. glabrata is the species of C. non albicans most found in several studies. This could be explained on the one hand by the fact that C. glabrata is one of the species most found among the Candida species commensal to the digestive tract and the genito-urinary tract. On the other hand, the increase in their incidence could be attributable to the selection pressure exerted by the increasingly increasing use of azoles in the treatment of certains cancers and vaginal candidiasis. [28]. The increase in non-albicans Candida species should raise fears of an increasingly frequent occurrence of recurrent vaginal candidiasis. Because these species are becoming more and more resistant to antifungals, especially on certains terrains. This could be explained on the one hand by the fact that C. glabrata is one of the species most found among the Candida species commensal to the digestive tract and the genito-urinary tract. On the other hand, the increase in their incidence could be attributable to the selection pressure exerted by the increasingly increasing use of azoles in the treatment of certains cancers and vaginal candidiasis. [28]. The increase in non-albicans Candida species should raise fears of an increasingly frequent occurrence of recurrent vaginal candidiasis. Because these species are becoming more and more resistant to antifungals, especially on certains terrains. This could be explained on the one hand by the fact that C. glabrata is one of the species most found among the Candida species commensal to the digestive tract and the genito-urinary tract. On the other hand, the increase in their incidence could be attributable to the selection pressure exerted by the increasingly increasing use of azoles in the treatment of certains cancers and vaginal candidiasis. [28]. The increase in non-albicans Candida species should raise fears of an increasingly frequent occurrence of recurrent vaginal candidiasis. Because these species are becoming more and more resistant to antifungals, especially on certain terrains. the increase in their incidence could be attributable to the selection pressure exerted by the ever increasing use of azoles in the treatment of certain cancers and vaginal candidiasis. [28]. The increase in non-albicans Candida species should raise fears of an increasingly frequent occurrence of recurrent vaginal candidiasis. Because these species are becoming more and more resistant to antifungals, especially on certain terrains. the increase in their incidence could be attributable to the selection pressure exerted by the ever increasing use of azoles in the treatment of certain cancers and vaginal candidiasis. [28]. The increase in non-albicans Candida species should raise fears of an increasingly frequent occurrence of recurrent vaginal candidiasis. Because these species are becoming more and more resistant to antifungals, especially on certain terrain
It is true that C. glabrata has often been found among the 3 nonalbicans Candida species isolated from vaginal samples. But, in Franceville, Gabon, this species had been the 6th species incriminated in vaginal candidiasis [24]. In Nigeria at Onitsha, Ejike Chinwe et al found that C. glabrata in their series was the ‘th species implicated in candidiasis caused by Candida non albicans [29].
The variable place occupied by C. glabrata infection may be attributable to various factors to which the populations studied are exposed. In addition, a more increasing involvement of Candida non albicans would expose women to increasingly symptomatic vaginal candidiasis due to the invasion of the vagina by fungi which, unlike C. albicans, do not belong to the flora commensal.
With regard to epidemiological aspects, in particular age, level of education, occupation, our study shows that candidiasis due to Candida non albicans has mainly affected single women during periods of sexual activity, unemployed and with an acceptable level of education. Such a patient profile could be explained by the performance of certain gynecological practices, without medical advice, having an impact on the vaginal flora. Unfortunately, the present work did not make it possible to notify aspects that could explain this epidemiological profile. Regarding the age of the patients, the majority of the patients were between [18-40 years old]. This is similar to the results of several studies carried out on vaginal candidiasis where the age group most affected by vaginal candidiasis was that of women in the period of genital activity [7-12,14,16,17,26]. However, the majority of these studies did not specifically focus on Candida non albicans candidiasis. The same is true for items related to occupation, level of education and marital status.
The implication of Candida non albicans is a reality in our country which should raise fears of an increase in cases of recurrent vaginal candidiasis with, as a corollary, an increase in resistance to antifungals. Because not only are these species involved, but they are becoming more frequent than candida albicans. Hence the need to study vaginal candidiasis in populations at risk in order to identify the mycotic ecology and adapt the management measures in our environment.
