Author(s): Mckey Remy, Akiki Laura, Hallal Marwa and Hallal Mahmoud*
Background: Lower gastrointestinal bleeding can cause a life-threatening condition especially in the elderly with multiple comorbidities. Whilst some infectious colitis can cause bloody diarrhea, usually the blood loss is minimal and does not require an endoscopic intervention.
Case Presentation: In this report, we present a case of a 64-year-old Lebanese female with multiple comorbidities including renal failure on hemodialysis, hypertension and multiple myeloma on chemotherapy who presented for an acute episode of lower GI bleeding as a result of an antibiotic associated colitis by clostridium difficile infection.
Conclusion: Therefore, we should be vigilant about infectious colitis as a cause of GI bleeding in the immunosuppressed individuals and elderly with multiple comorbidities.
Gastrointestinal bleeding can be classified into upper and lower source of bleeding anatomically according to the angle of Treitz [1]. Hence most cases of upper GI bleeding present with melena, while lower GI bleeding mostly cause rectorrhagia. However, hematochezia associated with hemodynamic instability may be indicative of a massive upper gastrointestinal (GI) bleeding source and thus warrants an upper endoscopy [2]. For that reason, physical examination and medical history are inseparably essential to decide the treatment protocol, timing and type of intervention needed for the patient.
Lower GI bleeding is a frequent cause of hospitalization of the elderly and is increasing in incidence due to the use of blood thinners especially in this population. Colonoscopy is the diagnostic and therapeutic intervention of choice because it can detect all sources of bleeding in the colon and treat the majority with cauterization or endoclips with very minimal complication rate [3].
We present a case of a 64 -year-old Lebanese female with a past medical history of hypertension, multiple myeloma currently on chemotherapy, ESRD on hemodialysis, presented to the emergency department for one day history of acute rectorrhagia. History goes back 4 weeks ago when the patient presented for a mild gastroenteritis that resolved on oral antibiotic Cefixime 400mg OD for 5 days that was prescribed by her family physician. Patient denied the use of any anti-platelets or anticoagulation therapy.
Upon presentation, the patient was pale and lethargic. Blood pressure 110/60 mmHg, heart rate 100 Bpm, no fever or chills and normal Spo2. Physical examination revealed a soft abdomen with fresh blood per rectum. Laboratory tests in the emergency showed Hgb 4 g/dl, platelets 38000/mcL, wbc 3000/mcL with normal ANC and normal PT and PTT. The patient was stabilized, given 2 units of pRBCS and 1 unit of platelets.
Twelve hours later, colonoscopy was done after regular purgative preparation. It showed 3 small elevated lesions in the rectum oozing blood, hemostasis was done using hot forceps fig1. The sigmoid, descending and transverse colon were tinged with blood but after cleaning with water jet it showed normal mucosa with no source of bleeding fig2. In the ascending colon and cecum there were multiple bullous shaped lesions with moderately active bleeding and mucosal sloughing fig3. Argon plasma coagulation was applied to actively bleeding lesions and biopsies were taken. Stool culture revealed positive GDH and clostridium difficile toxin A that confirmed the diagnosis of clostridium difficile induced hemorrhagic bullous colitis. Therefore patient started on vancomycin 125 mg orally every 6 hours. The next day our patient was clinically better with resolution of rectorrhagia and stabilization of her hemoglobin levels.
She was discharged home after 72 hours on oral vancomycin. Pathology Result Showed Benign Colonic Mucosa with Acute Inflammation

Figure 1: Showing a Rectal Retroflexed Vision of the Three Bleeding Bullous Lesions Marked by Arrow

Figure 2: Showing Normal Colonic Mucosa in the Descending Colon
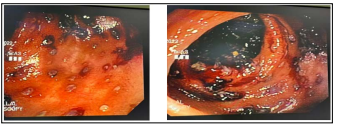
Figure 3: Showing the Bullous Bleeding Lesions with the Sloughed Fragile Mucosa in the Right Colon and Cecum
Antibiotic associated colitis is an undesirable side effect of the use of antibiotics in hospitalized and non-hospitalized patients; however it is especially encountered in the elderly and immunocompromised patients. It can range from an asymptomatic condition, sometimes with only leukocytosis, to a fulminant disease with severe diarrhea leading to dehydration, megacolon, pseudomembranous colitis and very rarely hemorrhagic diarrhea [4].
Usually, symptoms of CDI happen during or shortly after the course of antibiotics, although in some documented cases, the timeframe can extend as long as 10 weeks. In our case it happened 4 weeks after the use of antibiotics [5]. According to studies, 10-20% of the cases of AAC are due to C diff infection, the majority are related to other pathogens like Clostridium perfringens, Staphylococcus aureus, Klebsiella oxytoca, Candida species, and Salmonella species. In addition, it may be the result of allergic reaction of the intestinal mucosa to the antibiotic, a disturbance in the intestinal carbohydrate and bile acid metabolism or a pharmacological effect of the drug on the gut motility [4-6].
The majority of AAHC are found to be caused by Klebsiella oxytoca, they are categorized as clostridium difficile negative antibiotic associated hemorrhagic colitis, whereas only 14% are related to C diff [7,8]. The main picture is a severe segmental colitis typically in the right colon causing hematochezia, which can be treated with proper antibiotics. In most cases the condition will not cause massive blood loss and therefore no need for endoscopic intervention [9].
The mechanism underlying pseudomembranous colitis is toxin mediated, however the mechanism behind AAHC is still unknown and it is supposed to be immunologic in nature [10]. Nevertheless, it is very uncommon for a hemorrhagic colitis to cause severe blood loss and the need for an endoscopic intervention like our case, since almost all cases can be treated with antibiotics and supportive therapy [11]. Presumably we had an atypical case due to underlying multiple comorbidities and immunocompromised state. Supposedly, our patient had thrombocytopenia that also played a role in making her condition more severe. Consequently, infectious colitis can cause a serious condition in this category of patients and should be kept in mind for early diagnosis because it can be treated by resuscitation and antibiotic therapy.
Acknowledgements: We Thank the Patient for allowing us to publish this Report.
Funding: No Funding
