Author(s): Nidhi Sapolia*, Samar Qasem, Shushma Shetiya and Wael Hosni
Background: Ectopic pregnancy complicates 2% of all pregnancies, and accounts for 6% of pregnancy-related mortality [1]. It ends with rupture before the end of the first trimester [2]. Case Report: We report a case of a 27 yr old primigravida with unruptured left ovarian ectopic pregnancy treated with a wedge resection of ovary laparoscopically. Post-operative period of the patient was uneventful. Conclusion: Ovarian pregnancies are rare, and unruptured ovarian pregnancies are rarer. Early detection and treatment plays an important role in prevention of serious complications.
Apart from the tubes, pregnancies can also implant in unusual implantation sites, such as the previous cesarean scar, intra- abdominally, cervix, and ovaries. Ovarian pregnancy is a rare event, with estimates of frequency ranging from 1 in 2,100 to 1 in 7,000 pregnancies or 3% of all ectopic pregnancies.
It occurs when an ovum is fertilized prior to the release at the surface of the ovary itself and is retained within the ovary or the reflux of a fertilized ovum from the fallopian tube [1,2]. There is an associated increased risk with IntraUterine devices- one in every 9 ectopic pregnancies among IUCD users is an ovarian pregnancy [3].
Ovarian pregnancy appears to be a random event that is not associated with a history of infertility or recurrent extra uterine pregnancy [4].
Our patient is 27 years primigravida, she conceive spontaneously, her menstrual cycle was regular and uneventful medical or surgical history. For writing this study oral consent was obtained from our case She presented to the emergency department of our hospital at 6 week pregnancy as referred case of left ectopic pregnancy from other hospital with mainly complaining of pain in the left lower abdomen and vaginal spotting, On examination she was hemodynamically stable, abdomen soft with marked tenderness in the lower abdomen with no rigidity or guarding.
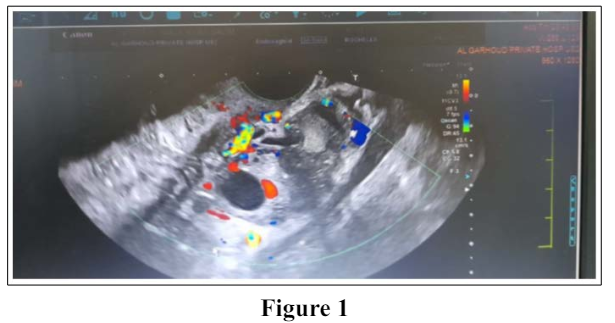
On admission her serum hCG was 3341, and The ultrasound revealed a normal size uterus with an empty uterine cavity and evidence of left adnexal heterogenous lesion is seen measuring 26x25mm showing minimal internal vascularity, Minimal free fluid seen in POD ,no right adnexal lesion are seen. A diagnosis of left ectopic pregnancy was made.
Following the patient’s consent, laparoscopic exploration was indicated.
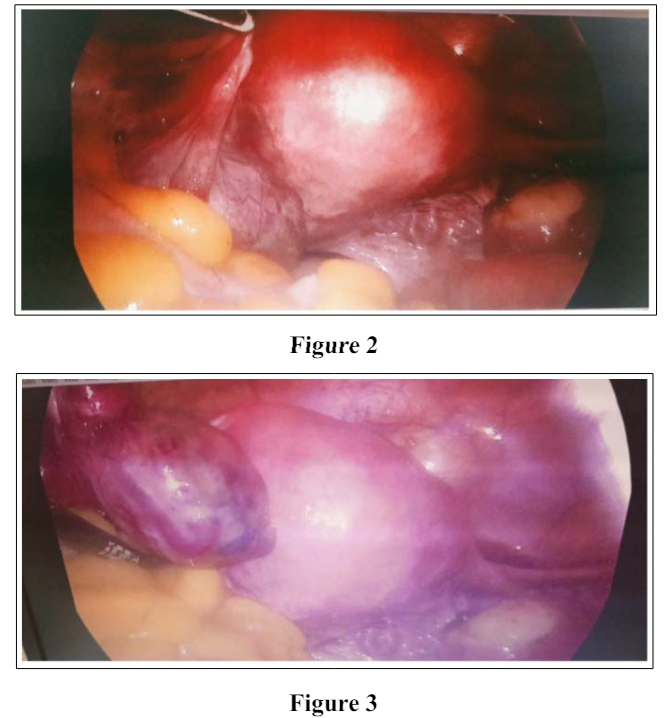
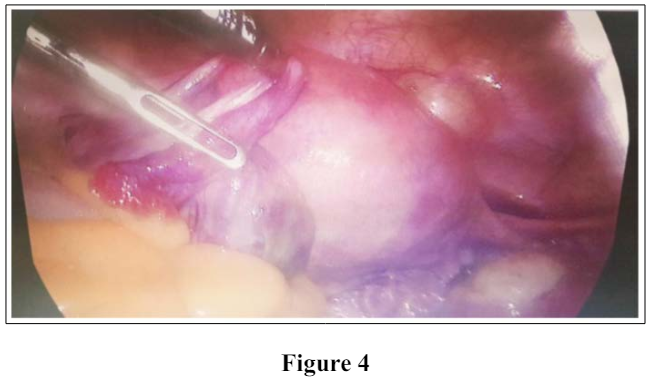
During the procedure, a normal-sized uterus, with normal right tube and ovary and normal left tube was seen. Left ovary was enlarged with the gestational sac seen at the posterior part of the ovary with some oozing was seen. Resection of the ovary was done and intact Laparoscopic removal of the gestational sac was performed. Hemostasis achieved with electrocautery.
Few Endometriotic spots were seen at the posterior aspect of Uterus and pouch of Douglas but no adhesion seen as shown in figure 2,3 and 4
The patient’s postoperative period was uneventful, and patient had no complication. The patient was discharged the next day. Postoperative pathological analysis confirmed left ovarian gestation.
The diagnosis of an ovarian ectopic pregnancy is difficult as it mimics a ruptured ovarian cyst or corpus luteum cyst. Transvaginal ultrasound increases the chances of an early diagnosis [3]. Laparoscopy is both diagnostic and therapeutic in these cases.
It is important to remember, however, that hemorrhage from ruptured ectopic pregnancy is still the leading cause of pregnancy- related maternal mortality in the first trimester and accounts for 4 percent of all pregnancy-related deaths, despite improved diagnostic methods leading to earlier detection and treatment [4-6].
Ovarian ectopic pregnancy is a rare type of ectopic pregnancy, and the pathogenesis remains unclear. Common risk factors for tubal ectopic pregnancy (e.g. pelvic inflammation) are not relevant in ovarian pregnancy. Suspected risk factors for ovarian pregnancy include prior use of the intrauterine device (IUD), assisted reproductive techniques, concurrent endometriosis leading to pelvic adhesions and intrauterine surgery causing intrauterineadhesions [7].
In addition, concurrent endometriosis and pelvic adhesions can block ovulation, forcing the egg cell to stay in the ruptured follicle and develop in the ovary causing and ovarian pregnancy. Some scholars believe that the irregular maturation of follicles during ovulation could also cause ovarian pregnancy [8].
There are no specific agreed criteria for the ultrasound diagnosis of ovarian ectopic pregnancy. A transvaginal ultrasound showing a normal size uterus with an empty cavity and a wide echogenic ring with an internal anechoic area on the ovary can be suspicious of an ovarian ectopic pregnancy. A yolk sac or embryo is less commonly visualized [9,10].
The corpus luteum should be identified separate from the suspected ovarian pregnancy. Colour Doppler may aid detection of a fetal heart pulsation within the ovary. A complex echogenic adnexal mass with free fluid in the pouch of Douglas without a visualization of a separate ovary can represent a ruptured ovarian ectopic pregnancy. As it can be difficult to distinguish ovarian ectopic pregnancies from corpus luteal cysts, tubal ectopic pregnancy stuck to the ovary, ovarian germ cell tumours and other ovarian pathologies. Diagnosis is usually confirmed surgically and histologically. After surgical treatment, the histopathology result will confirm the diagnosis of ovarian ectopic pregnancy [11].
Minimal access surgery is now the treatment of choice for ovarian ectopic pregnancy. Removal of the gestational products by enucleation or wedge resection (in the presence of a large ectopic mass) is preferred. Enucleating the products of conception bluntly from the ovary minimises damage to the surrounding ovarian tissue. Haemostasis can be achieved by electrocautery or suturing. Oophorectomy is occasionally required when there is coexisting ipsilateral ovarian pathology or excessive bleeding. Systemic methotrexate can be used to treat ovarian ectopic pregnancy postoperatively in the presence of persistent residual trophoblast or persistently raised b-hCG levels [11,12].
Ovarian pregnancy is a rare form of ovarian pregnancy. Once the ovarian pregnancy is ruptured, a massive hemorrhage can lead to severe maternal morbodity. Early detection of an unruptured ovarian pregnancy can allow implementation of an active treatment plan to reduce the risk of serious complications [13].
A special thanks to the nurses in the operation theater, emergency room, the inpatient ward and a special note of thanks to Dr Samar and Dr Shushma for assisting in the surgery and taking great care of the patient post operatively.
1. American College of Obstetricians and Gynecologists (2008) ACOG Practice Bulletin No. 94: Medical management of ectopic pregnancy. Obstet Gynecol 111: 1479-1485.
2. Shrestha A, Chawla CD, Shrestha RM (2012) Ruptured primary ovarian pregnancy: a rare case report. Kathmandu Univ Med J 10: 76-77.
3. Comstock C, Huston K, Lee W (2005) The ultrasonographic appearance of ovarian ectopic pregnanciesObstet Gynecol 105: 42-45.
4. https://www.uptodate.com/contents/ectopic-pregnancy-epidemiology-risk-factors-and-anatomic-sites?.
5. Creanga AA, Shapiro-Mendoza CK, Bish CL, Suzanne Zane, Cynthia J Berg, et al. (2011) Trends in ectopic pregnancy mortality in the United State: 1980-2007.Obstet gynecol 117: 837-843.
6. Berg CJ, Callaghan WM, Syverson C, Hendrson Z (2010) pregnancy related mortality in the United State, 1998 to 2005. Obstet gynecol 116: 1302-1309.
7. Ghasemi, Sajad Jeddi (2014) Streptozotocin as a tool for induction of rat models of diabetes: a practical guide. EXCLI J 22: 274-294.
8. Suikkari, Viveca Söderström-Anttila (2007) In-vitro maturation of eggs: is it really useful? 21: 145-155.
9. Comstock C, Huston K, Lee W (2005) The ultrasonographic appearanceof ovarian ectopic pregnancies.Obstet Gynecol 105: 42-45.
10. Shiau CS, Hsieh CL, Chang MY (2007) Primary ovarian pregnancy.Int J Gynaecol Obstet 96: 127.
11. RCOG Green-top Guideline No. 21e29 of e55ª2016 Royal College of Obstetricians and Gynaecologists https://www. rcog.org.uk/guidance/browse-all-guidance/green-top- guidelines/.
12. Joseph RJ, Irvine LM (2012) Ovarian ectopic pregnancy: aetiology, diagnosis, and challenges in surgical management.J ObstetGynaecol 32: 472-474.
13. Goyal, Sonal Singh, Erica MS Sibinga, Neda F Gould, Anastasia Rowland-Seymour, et al. (2014) Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med 174: 357-368.
View PDF