Author(s): <p>Nwaopara Uche</p>
Background: Some medical disorders occurring in psychiatric settings cause diagnostic delays and missed diagnoses which may lead to poor prognosis and outcomes.
Aim/Objective: The aim was to determine the uncommon medical diagnosis and their profiles among psychiatric settings in South-South, Nigeria.
Materials and Methods: The study was done in centers across three states in a cross-sectional descriptive study that examined diagnostic profiles of a sample of 134 psychiatric patients that received medical care over one year (July 2021-July 2022) using questionnaires generated by the clinical team. Data analysis: was done using SPSS version 27. Chi-squared tests were conducted and a probability value of p<0.05 was considered significant.
Results: The results show a preponderance of females with a frequency of 66.4% when compared to 33.6% for males. The most predominant age range was 10-19 years with 57 (42.5%) patients and 78.6% below 30 years. Most of the patients (49.25%) were married, and 41.79% were single. A statistically significant relationship existed between marital status, age, education, and medical diagnosis (X2 =5.0, p=0.02, X 2 =11.2, p=0.00, X2 =5.33, p=0.02, respectively). Neurological medical conditions were the most predominant medical conditions found in the psychiatric settings used for the assessment with a value of 61.17 %. while surgical co-morbidities were the least rare presenting diagnosis in psychiatric settings, with a value of 2.98%.
Conclusion: Clinicians including the psychiatrist, in the multi-disciplinary team, must be aware of the risk of medical diagnosis encountered in neuropsychiatric settings, to reduce diagnostic errors, mitigate morbidity and ultimately improve the outcome of the organic conditions.
Physical illness in a psychiatric ward, its assessment, and management have been noted to be stressful and challenging [1]. Co-morbidity is a medical concept defined as the co-occurrence of mental and physical disorders within the same person, regardless of the chronological order in which they occurred or the causal pathway linking them [2].
Consultation-Liaison Psychiatry (CLP) is the study of these comorbidities between medical general conditions and psychiatric illnesses. The role of CLP is that of a link between psychiatry and other medical fields. Thus, the consultation-liaison psychiatrist can be referred to as the psychiatry’s ambassador in the general hospital setting [3,4]. The psychiatrist will usually be the medical expert in the unit and it is the responsibility of the psychiatrist to recognize and treat these psychiatric conditions, and also to develop good working relationships with the patients and the clinical team [5]. Current data indicate these guidelines, with the psychiatrists playing an integral role [5-7].
Recent studies on diagnostic error have not focused on patients who are being treated in mental health clinics or inpatient psychiatric units; however, past studies of psychiatric patients found that important medical diagnoses were missed in these patients as often as 40% of the time, depending upon the setting. Moreover, these medical diagnoses were not uncommonly the sole cause or a significant contributing factor to the patients’ presentations but non-specific psychological symptoms [8].
It is well established that the pathways that cause co-morbidity of mental and medical disorders are both complex and bidirectional [9]. Related to this is the fact that medical emergencies, some presenting as unusual or uncommon disorders among psychiatric patients, may receive delayed medical responses or remain undetected if medical emergency training and response are not in place, it has been reported that at an advanced age, serious medical and psychiatric illnesses usually coalesce [6,10]. An example of this is the fact that some admissions to most inpatient geriatric psychiatric care arise because of these coexisting medical problems [11]. Mental disorders are often associated with one or more chronic physical diseases and lead to even more aggravating physical consequences for patient health [12]. In a related study,
the number of people who receive initial emergency care increased their survival rate to 30% more than those who do not [10,13]. It is a matter of great concern that these medical emergencies, which sometimes cause diagnostic puzzles, may sometimes lead to negative patient outcomes, including death, among mentally ill patients [14]. It had been reported that these persons have a 2 to 3 times higher risk of dying from cardiovascular diseases than the general population [15].
A previous report stated that most deaths in persons with severe mental disorders are due to preventable physical diseases, especially cardiovascular disease, respiratory disease, and infections [16]. Overall, cardiovascular diseases, orthopedic conditions, chronic respiratory, gastrointestinal, and cancer diagnoses, had been noted to be the most prevalent co-morbid medical conditions, while immunologic conditions are said to be the least prevalent with co-morbid psychiatric conditions [7,16]. A study done at the outpatient clinic in Uyo Akwa Ibom Nigeria looked at only anxiety and depression co-occurring with medical conditions. It found out the distribution of medical disorders among respondents that were recruited for the study. Among those evaluated, 22.04% had cardiovascular disease(hypertension), 15.91% malaria, 14.28% gynecological disease (pelvic inflammatory disease), 7.75% digestive system disorder(peptic ulcer disease), 7.34% endocrine disorder (diabetes mellitus), 6.93% musculoskeletal disorder (osteoarthritis), 5.71% psychological disorders, 4.08% Urology (benign prostatic hyperplasia), blood and immune disorder(human immunodeficiency virus/acquired immunodeficiency syndrome) and respiratory disorder (upper respiratory tract infection), 2.4% skin disorders, 1.22% neurological disorders, and 0.81% ear, nose and throat disorders. Respondents that were diagnosed with hypertension had a p-value of 0.016 for anxiety and 0.025 for depression. Similarly, respondents with HIV/AIDS had a p-value of 0.006 [17]. The complexity of physical co-morbidities from clinical practice usually makes hospitalization imperative and thus requires intensive medical treatments combined with evidence-based psychosocial and behavioral interventions [18]. Tests are sometimes limited and may be indicated (18, X, Beck, and Steenstra, 2015). If more complex or rapid tests are needed to exclude a serious diagnosis, the patient is transferred to the emergency department or referred to other centers which may be time-consuming [20]. Medical assessment among this category of mentally ill patients in psychiatric settings is usually done by history, physical examination, and often brain imaging and laboratory testing [21]. This medical assessment of patients with mental symptoms seeks to identify physical disorders mimicking mental disorders, physical disorders caused by mental disorders or their treatment, and physical disorders accompanying mental disorders [22]. Patients typically should have pulse oximetry, fingerstick glucose testing, measurement of therapeutic drug levels, urine drug screening, blood alcohol level, complete blood count, urinalysis, HIV testing, Serum electrolytes (including calcium and magnesium), blood urea and creatinine, Erythrocyte sedimentation rate or C-reactive protein [22]. Imaging tests include Brain CT, Brain MRI, Thyroid function tests, Chest x-ray, Blood cultures, and Liver Function tests [23]. Conversely, a previous study demonstrated that patients presenting with a current primary psychiatric complaint and diagnosis or a previous psychiatric history and normal medical history and physical exam, have a very low likelihood of clinically significant laboratory findings [24].
The psychiatrist, must, therefore, have a high index of suspicion for co-morbidity when assessing patients and most specifically when decisions are made about treatments because the psychiatric treatments may also affect the medical conditions [6,24,25]. This leads to process-based integration, which is conceptualized as integrated care, resulting in a fluid, interdisciplinary approach that generates benefits for the whole patient, and ultimately improves outcomes [25].
However, little is documented, on the uncommon current mental disorders diagnosed in patients receiving psychiatric care in hospital settings, especially in South-South Nigeria. The objective of this study was to characterize uncommon medical disorders and presentations, their diagnostic profiles, and co-existing with patients undergoing psychiatric care in hospital settings in SouthSouth Nigeria between July 2021-July, 2022 The purpose of this paper is to demonstrate the need for integrating medical care in psychiatric facilities, with psychiatrists playing an integral role in this multi-disciplinary approach of integrated care, which determines the success of medical response and outcome strategies.
The study locations are the Federal Medical Center, Yenagoa, and the Military Hospital, Port Harcourt. Federal Medical Centre Yenagoa, also known as FMC Yenagoa, is the biggest and outstanding Hospital in the heart of Yenagoa, Bayelsa State, Nigeria. The services offered range from mother and child delivery to Optometric, Ear Nose, and Throat (ENT), Orthopedic, Mental Health, etc. The Military Hospital, Port Harcourt, formerly called Delta Clinic. is an Armed Forces health facility in New GRA, Port Harcourt local government area, Rivers State, Nigeria. The hospital is being upgraded to the level of a tertiary health facility, providing specialist services of medicine in multiple disciplines, including Mental Health. The third location was ACRA specialist Clinic, a private specialist psychiatric service center, offering specialist psychiatric services in Bayelsa and Akwa Ibom states.
The research team conducted a cross-sectional descriptive study that examined diagnostic profiles of a sample of 134 psychiatric patients that received medical or surgical care over a one-year (July 2021-July, 2022).
Participants were psychiatric in and outpatients, who were 5 years and older, seen, admitted, and diagnosed at 3 psychiatric centers, namely, ACRA Specialist Clinic, Military Hospital, Port Harcourt, and Mental Health Department of Federal Medical Center, Yenagoa, in Akwa Ibom, Rivers, and Bayelsa respectively, all in South-South, Nigeria, who had co-existing medical conditions and disorders, between the study period, were evaluated. Those without co-morbid unusual medical conditions were excluded.
Cross-sectional descriptive study
The non-probability sampling method, called convenience sampling, which is allowed in clinical research, was used, in which patients were recruited, based on their availability and accessibility.
The Federal Ministry of Health, National Health Management Information System Health Facility Daily Attendance Register (Version 2013) was used to review the patients in terms of outpatient, inpatient, specialist medical care, and psychiatric diagnosis.
The Mental Health Units in the centers provided psychology services that include screenings, standardized clinical evaluations, neuropsychological rehabilitation, and consultation-liaison (C-L) services across the designated centers across the South-South region of Nigeria. The medical team is coordinated by a physician and a psychiatrist. The clinical team’s liaison services involved the administration of routine standardized medical clinical evaluations for all patients in the psychiatric wards or outpatient clinic with cardiovascular illnesses (b) Endocrine disorders, (c) Immunologic, and (d) Neurologic conditions and Central nervous system conditions. Additionally, the medical officers in the medical team-initiated consults as requested by visiting consultant physicians, regardless of the inpatient unit to which the patient was admitted. The research team analyzed sociodemographic profiles, current ICD-10 psychiatric diagnoses, and unusual medical diagnoses made at patients’ bedside during the standardized clinical evaluation
These patients’ medical and psychiatric diagnoses were arrived at after clinical evaluation on presentation and gave informed consent for data collection within the study period. The standardized clinical evaluation entailed a mental status examination, an exploration of psychological and emotional symptoms, a review of past physical and mental illness history, and a review of social functioning. Additionally, a review of laboratory results, medications, and physician and nurse progress notes was conducted to aid in ruling out organic causes of possible mental aberrations. The clinical team performed the standardized clinical evaluation at the patient’s bedside. If warranted, the clinical team made a current DSM-5 diagnosis and a corresponding brief treatment plan was implemented for the duration of the patient’s hospital stay.
Questionnaires generated by the clinical team were used to collect the following biopsychosocial variables: age, biological sex, marital status, level of education, and occupation/employment status.
ICD-10 medical diagnoses were obtained from specialist reviews performed by consultant physicians from the medical team.
This study used SPSS 27 (IBM Corp) to perform data analysis. Data preparation and exploration procedures were conducted, and data were examined for errors and quality. Descriptive analysis was conducted for data analysis. Frequencies and proportions were used. Chi-square tests were conducted. Chi-squared tests of independence were conducted to assess associations between the diagnosed medical disorders and select sociodemographic indicators Probability value of p<0.05 was considered significant.
These datasets generated and/or analyzed during the current study are not publicly available because it was used under license, and also due to ethical restrictions clearly stated in the ethical approval letters gotten from the study centers. However, the data are available from the corresponding author on reasonable request, and with the approval of the authorities of the three centers used for the study.
The study was fully approved by the ethical committees of the Military Hospital Port Harcourt, Federal Medical Center, Yenagoa, and ACRA Specialist Clinics. Access of researchers to participating hospitals was approved by the Research and Development departments of each of them. Written consent was obtained from each participant who expressed interest to take part in the study. Informed consent was obtained from all participants included in the study. For participants less than 18 years, according to the child rights act, informed consent was obtained from a parent or legal guardian, as a pre-condition for study participation. The consent form was approved as part of their full approval of the study. Every author certifies that the study was performed following the ethical standards set by the 1964 Declaration of Helsinki and its later amendments.
Sociodemographic characteristics as depicted in Table 1, showed that out of the 134 patients reviewed within the study period of July 2021-July, 2022, there was a preponderance of females with a frequency of 66.4% as compared to 33.6% for males. The most predominant age range was 10-19 years with 57 (42.5%) patients and 78.6% below 30 years. Most of the patients (49.25%) were married, 41.79% were single, and 8.95% of participants were separated or divorced. Most patients (27.6%) were from the Ibibio/ Annang/Efik tribe and 46.5% and 38% of participants, had primary levels of education respectively. Table 2, shows the frequency of distribution of the uncommon medical disorders found among the study participants. PNES was the most uncommon disorder with a frequency of 25 (18.65%), followed by infections (herpes simplex, hepatitis syphilis) with a frequency of 14 (11.44%). Priapism and Urinary retention were the least disorders noted with a frequency of 1 (0.74%) each respectively. Figure 1, is a Pie chart showing diagnostic profiles of uncommon medical disorders in groups. The neurological disorders sub-group was the most prevalent while the surgical disorders sub-group was the least prevalent.
| Variables | Frequency (n=134) |
|---|---|
| Sex | |
| Male | 45 |
| Female | 89 |
| Marital Status | |
| Single | 56 |
| Married | 66 |
| Divorced/Separated | 12 |
| Age | |
| ≤10 | 3 |
| 10-19 | 57 |
| 20-29 | 32 |
| 30-39 | 199 |
| 40-49 | 14 |
| ≥50 | 9 |
| Religion | |
| Christianity | 125 |
| Islam | 7 |
| Traditional Religion | 2 |
| Education | |
| Primary | 51 |
| Secondary | 65 |
| Tertiary | 12 |
| No Education | 6 |
| Tribe | |
| Ijaw | 52 |
| Ibibio/Annang/Efik | 37 |
| Ibo | 29 |
| Others | 16 |
There was a statistically significant relationship between marital status, age education, and medical diagnosis (X2 =5.0, p=0.02, X 2 =11.2, p=0.00, X2 =5.33, p=0.02, respectively)
| Unusual Medical Disorders | Frequency (n=134) |
|---|---|
| Psychogenic non-epileptic seizures (PNES). | 25 |
| Skin adverse drug reactions (Erythema multiforme, scrotal steatocytomas, urticarial reactions, Steven Johnsons syndrome) | 11 |
| Septic Shock | 4 |
| Hypovolemic shock | 9 |
| Cervical Dystonia | 5 |
| Tics (Motor and vocal) | 12 |
| Urinary retention | 1 |
| Priapism | 1 |
| Neurogenic shock | 6 |
| Young-onset Hypertension | 3 |
| Post-concussion syndrome | 8 |
| Subdural Hematoma | 3 |
| Amnesia (Anterograde and retrograde). | 4 |
| Maturity onset diabetes of the Young | 2 |
| Infections (Herpes simplex, Hepatitis, syphilis) | 14 |
| Systemic Lupus Erythematosus | 4 |
| Hyperthyroidism | 4 |
| Trigeminal Neuralgia | 7 |
| Narcolepsy | 10 |
| Total | 134 |
Figure 1 below shows that neurological medical conditions were the most predominant medical conditions found in the psychiatric settings used for the assessment with a value of 61.17 %. while surgical co-morbidities were the least presenting diagnosis in the psychiatric settings with a value of 2.98%.
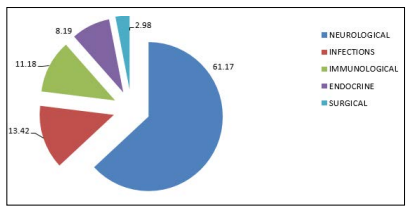
Figure 1: Pie Chart Showing Diagnostic Profiles of Uncommon Medical Disorders in Groups
This result agrees with the fact that physical disorders can mimic mental disorders and therapists should learn to recognize and unmask the psychological presentation of medical disorders [26]. A related study agrees with this, concluding that non-specific behavioral and mood alterations may represent the very first and, occasionally for prolonged periods, the one single and exclusive sign of an undetected physical illness, sometimes causing a delay in diagnosis [27]. These masked physical conditions. as was the case over the study period, frequently mislead the clinicians and sometimes obliterated any further medical consideration, resulting in misdiagnosis and sometimes inevitably, leading to the misapplication of treatment modalities [28]. Given this, the findings also agreed with the long-established fact, that the variability of a disease presentation, makes the process of clinical diagnosis challenging, even when there are laboratory results that will rule out a particular diagnostic entity [29]. Study findings are also consistent with an earlier report that showed that even when patients’ problems appear psychological, an underlining physical disorder may be the causative factor because of the non-specificity of psychological symptoms [26,29]. This may be because most people sometimes tend to think of the mind and body as separate entities. In contrast to this, however, is the fact that the mind and body are interconnected [30]. This, therefore, makes it imperative for clinicians to be aware that there will be a potpourri of diseases, many uncommon, which may be encountered in the course of their practice in a general medical or neuropsychiatric setting [31,32]. Therefore, knowledge acquired from meticulous case analyses and differential diagnosis requirements is expected to stimulate curiosity and makes clinicians think beyond the old and mundane requirements of daily practice, to avoid or reduce incidents of missed diagnosis [32]. It is worthy of note that neurological disorders formed the majority of the uncommon physical illnesses found among psychiatric patients in this study, showing that many undetected nervous system disorders require clinical care by physicians and other healthcare professionals, including psychiatrists [33]. Recent research reports that an unusual surge of new-onset tics in patients with no prior history of these disorders had been tied to psychological stress and even stress due to the Covid-19 pandemic [34].
The finding of priapism as an uncommon finding is in keeping with previous studies that reported it as an infrequent, rare, and serious adverse event of antipsychotic medication use which requires emergency evaluation and intervention because of its serious longterm complications which include erectile dysfunction [35,36]. A study showed that urinary retention was reported in patients on some Atypical or typical antipsychotics, tricyclic antidepressants, and selective noradrenaline reuptake inhibitors, with improvement, noted on discontinuation or dose reduction of the drugs causing the Urinary retention [37]. In this study, surgical emergencies, including priapism and urinary retention, were the least prevalent. This may be explained by the fact that surgical side effects of medications used in neuropsychiatric settings are either rare or the diagnosis is promptly referred because of the potential adverse outcome or danger such diagnosis usually portend [31,36].
The finding of Systematic Lupus Erythematosus (SLE), as an uncommon presentation in this study, agrees with the finding in a related study that psychiatric symptoms can be a manifestation of SLE, involving the central nervous system. The mechanism implicated in neuropsychiatric manifestations involves vascular injury mediated by antiphospholipid antibodies or immune complexes and autoimmune/inflammatory reactions accompanied by increased blood-brain barrier permeability [38]. These expressions of psychiatric manifestations have been considered to be associated with disease activity, side effects of medications, and/or psychosocial stresses from the chronicity of the disorder, via mechanisms that have not been fully understood [38,39]. Psychogenic Non-Epileptic Seizures (PNES) were the most prevalent neurological disorder found in this study. However, despite advances in establishing an accurate diagnosis and evidence-based treatments, recent knowledge about PNES has not been well translated into clinical practice, leading to long diagnostic delays, poor prognosis, and outcomes [40]. PNES had been reported as a complex neuropsychiatric disorder that needs careful psychiatric assessment and psychiatric comorbidities need to be carefully assessed [41]. A previous study had reported a nineyear delay in establishing the correct diagnosis of PNES, making it imperative that clinicians be aware of factors that maintain and perpetuate the symptoms [41].
The implication of these findings for clinicians is that non-specific behavioral and mood alterations often represent the very first and occasionally for prolonged periods, the one single and exclusive sign of an undetected physical illness. Flagrantly and convincingly “psychological” on presentation, such masked physical conditions frequently mislead the examiner and obliterate any further medical consideration, resulting in misdiagnosis and thus, inevitably, in treatment gone astray [28]. Recent studies have found that any individual with a “psychiatric history” or with “presenting symptoms in the sphere of mental functioning and behavior” is especially prone to experiencing a diagnostic error [42]. Diagnostic errors in primary care have harmful consequences for patients/ caregivers, practitioners, and health systems [43,44]. This is important because preventable harm may occur when undiagnosed conditions remain untreated. It is, therefore, necessary to alert all psychiatrists, to have a high index of suspicion in their routine clinical practice to be able to detect these uncommon syndromes. It also means that improving the diagnostic process is possible and presents a moral, professional, and public health imperative [45]. Furthermore, it is advised that it is helpful for clinicians to be aware of the possibility of “premature closure,” the tendency to stop investigating once you have come upon a diagnostic hypothesis but before that hypothesis has been fully proven [46]. This is an especially easy error to make when a medical condition has a long prodromal period without symptoms that are specific enough to make a clear medical diagnosis [19,47-49].
The study stresses the presence of uncommon medical diagnoses in psychiatric settings, sometimes causing diagnostic puzzles. Thus, there is, therefore, a need to sensitize mental health professionals about recognizing these unusual medical comorbidities and their prompt treatment via liaison with physicians and a teamwork approach with other medical staff. This is of utmost importance since even General Practitioners (GPs) see people with uncommon or rare medical conditions and some of these conditions are also present in psychiatric settings. Therefore, both categories of clinicians have a crucial role in making appropriate referrals, coordinating care, supporting families, and linking them with psychosocial and other supports.
Psychiatrists rely on hospital systems to optimize diagnostic endeavors. Therefore, medical or healthcare institutions need to make available, effective communication and referral systems to allow collaboration with the multidisciplinary management team to optimize the care of the patient and to allay the fears of his or her family. It is also necessary to ensure adequate provision of modern health information technology equipment, reliable laboratory services, and access to library resources. There is also the onerous need for expert second opinions, which should be emphasized. A multidisciplinary approach to management is, therefore, strongly advocated. The ultimate goal in all these protocols is making concerted efforts, which are geared toward reducing diagnostic error rates, within the best means possible.
A small sample size because of difficulties in finding the sample with the right characteristics and parameters will affect the study findings’ generalizability. The use of convenient sampling in data collection is also known to be prone to bias. An oversight level to avoid bias was established by referring the work to peer review and the different ethics committees.
The author confirms that there is no conflict of interest.
None declared.
