Author(s): <p>Joanna Skillman*, Pratap Dutta, Peter K Kimani, Ian Leaver, Matthew Venus, David Wallace, Joseph Hardwicke and Christopher Imray</p>
Purpose: Does a non-invasive pulse oximeter probe accurately indicate limb ischemia with inflation of a tourniquet? How are the pulse waveform, perfusion index and oxygen saturations affected? Does pulse oximetry return to normal with restoration of blood flow? Are the findings similar, regardless of which probe is used? Methods: Single Centre, pilot, proof of concept study. Each volunteer staff member had two probes applied to both lower limbs and then to both upper limbs. One limb had a tourniquet applied (experimental limb). The pulse oximeter trace, perfusion index and oxygen saturations were recorded before tourniquet inflation (time point 0), at inflation (time point 1), just prior to deflation (time point 2) and after deflation when the waveform returned to a biphasic appearance (time point 3). Results: Changes in both pulse oximeter waveforms occurred within 45 seconds of tourniquet inflation, with flattening of the biphasic trace followed by complete loss of amplitude, which normalized on release of the tourniquet. Perfusion index values for the experimental arms and legs were statistically significantly smaller than the control sides during tourniquet inflation and exceeded baseline on deflation, due to reperfusion. Oxygen saturations were unreliable and did not reflect tourniquet inflation. Conclusion: Pulse Oximeter waveform and perfusion index provide a noninvasive, sensitive, responsive, available, repeatable, objective measure of vascular supply in the limbs in healthy volunteers, although oxygen saturation is not a reliable indicator of perfusion. Objective assessment using the pulse oximeter could aid clinical judgement in initiating early vascular intervention in limb injury.
The purpose of this study was to establish if the pulse oximeter probe could accurately diagnose compromise to the blood flow in the limb after application of a tourniquet. The clinical application of this proof-of-concept study could be applied to vascular compromise following an open fracture of the tibia or humorous or following dislocation of a native knee or ankle joint or in compartment syndrome.
Prolonged lack of blood flow leads to muscle death, which can cause loss of function, chronic pain, limb deformity and ultimately a higher chance of amputation. Accurate and fast diagnosis of vascular compromise followed by prompt surgical correction reduces the duration of muscle ischaemia, helping to prevent muscle death.
A cold, pulseless, pale limb has vascular compromise until proven otherwise, but in many cases the limb is neither completely normal (warm, with pulses and pink) nor completely devascularised. In these cases, clinical assessment of capillary refill and pulses are used to assess sufficiency of vascular supply. However, normal capillary refill does not exclude poor perfusion, neither are the pulses an accurate enough predictor of vascular injury [1,2]. The use of Doppler ultrasound was previously recommended in the BAPRAS/BOA (2009) guidance as an adjunct to help with the clinical diagnosis of limb ischaemia and absent pulses. However, in the new NICE guidance, 2016 specifically states not to rely on a Doppler signal to exclude vascular injury [3,4]. Neither guidance state that distal capillary refill time should be used when distal pulses are absent, due to the potential pooling of peripheral blood [3,4].
Invasive investigations such as angiography or CT angiography can provide images to diagnose vascular occlusion but sometimes result in delays to surgical exploration and therefore prolong ischaemia.
A simple, repeatable, non-invasive test in the form a pulse oximeter may help predict which patients should have immediate surgical exploration of the limb without the need for further vascular imaging. Vascular impairment requires immediate surgery and restoration of the circulation using shunts, ideally within 3-4 hours, with a maximum acceptable delay of 6 hours of warm ischaemia. The limb salvage rate decreases from 88% to 61% after 6 hours of warm ischaemia [5].
The pulse oximeter has been used as an adjunct in the management of supracondylar humeral fractures in children, which can affect perfusion of the forearm. Pulse oximetry waveform has been reported to provide high sensitivity in detecting vascular problems requiring surgical exploration and has been described in lower limb trauma, as a potential adjunct to clinical examination [6,7].
The Pulse oximetry in Limb Salvage (The PULSE Study) was a proof-of-concept study. The aim of the study was to investigate how the pulse oximeter trace, the perfusion index and oxygen saturations varied with tourniquet inflation. The PULSE Study was approved by Northwest/Haydock national research committee. IRAS project ID: 269444, protocol number JS 442219, REC reference 19/NW/0528, Sponsor UHCW.
The clinical scenario of reduced blood flow to the limb was simulated by applying and inflating a tourniquet (Brand Name: ANETIC AID AT4 Electronic Tourniquet System 40080, Company Name: Anetic Aid Ltd, Havant, Hampshire UK) and occluding the blood flow for a short (90 second) interval. The pulse oximeter trace, perfusion index and saturations were recorded simultaneously on both the Masimo (Brand Name: MASIMO Rad97 Model: 9738, Company Name: MASIMO CORPORATION Irvine CA 92618 USA) and Phillips pulse oximeter probes (Brand Name: PHILIPS Intellivue Pulse Oximetry Module M1020B #A01 SpO2 Module with Model: 862112, Company Name: Philips Medizin System Böblingen Gmbh.) attached to the relevant display systems (Brand Name: PHILIPS Intellivue MX800 Patient Monitor, Model: 865240, PHILIPS Intellivue Multi Measurement Server X2, Model: 865039, Company Name: Philips Medizin System Böblingen Gmbh). Masimo and Philips probes were both used in the limbs without the tourniquet (control limb) and with the tourniquet (experimental limb) to allow comparison / equivalence between the 2 testing systems simultaneously
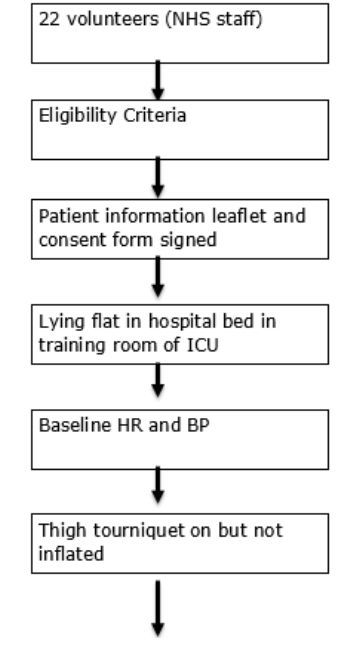
Participants were volunteer members of staff at a single Centre. They were invited into the test room, eligibility assessed, and participant information sheet provided. Inclusion criteria: volunteer members of staff, all ethnicities, aged 18 years or above, male and female, able and willing to provide informed consent. Exclusion criteria: peripheral vascular disease, diabetes, heart disease, kidney disease, previous venous thromboembolism, lower limb injury, pregnancy, under the age of 18 years, unable to provide informed consent.
There were 22 participants and each participant contributed to both control and experimental sides (left and right sides) and hence provided both control and experimental outcomes. (See Appendix for flow chart of study).
Volunteers were warned of transient discomfort associated with the tourniquet inflation and for the period of the time the tourniquet was inflated and that they may experience a‘rush of blood’, feeling back into the limb after the tourniquet was released. However, the same tourniquets are used routinely in surgery for more than one hour, without any long-term consequences.
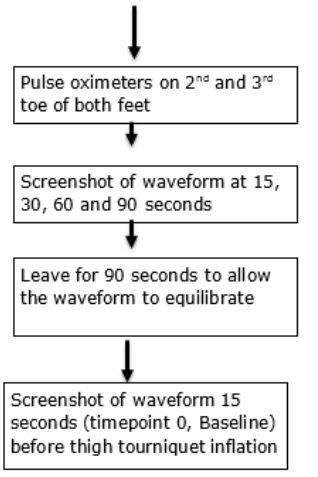
The volunteer lay on the couch and a baseline pulse and blood pressure were recorded. Hand dominance and gender were recorded. A tourniquet was applied to one thigh and the Masimo and Phillips probes applied to the second and third toes of both the experimental limb and the control limb. The pulse oximeter trace, perfusion index and saturations were recorded. The tourniquet was inflated to 300 mmHg (which exceeded the systolic blood pressure by >100 mmHg in all volunteers). The pulse oximeter trace was recorded continuously. The perfusion index was recorded before inflation (time point 0 = baseline), at the point the oximeter waveform lost its amplitude (time point 1= during inflation, trace lost), during inflation (minimum value) before release of the tourniquet (time point 2) and after deflation (time point 3).
This procedure was repeated on the upper limbs with the inflation pressure set to 250mmHg. All equipment was carefully cleaned between participants. All investigations were carried out before COVID-19 arrived in the UK (January 2020).
At the end of the data collection, data were downloaded (pulse rate, saturations, and perfusion index) for the whole time period from the central workstation in Intensive care, including a print off of the pulse oximeter trace and perfusion indices and oxygen saturations. Perfusion index was calculated as the ratio of the pulsatile blood flow to the non-pulsatile blood in peripheral tissue.
We summarised gender composition and other categorical participants’ characteristics using count and percentages. Pulse, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were summarised by reporting appropriate measures for continuous data such as mean, median and interquartile range.
The pulse oximeter traces were examined for changes in response to tourniquet inflation and deflation. We explored perfusion index values by plotting individual participant profiles across timepoints 0 to 3. We also reported count and percentages of perfusion index values equal to zero.
At inflation we compared control and experimental sides perfusion index data using nonparametric Wilcoxon signed-rank tests. Nonparametric tests were used because during inflation, perfusion index values were mostly equal or close to zero and so they were not normally distributed. To assess whether at deflation perfusion index values revert to baseline values, we fitted linear mixed models that included baseline and deflation data. The models included a random effects term for participant and fixed effects terms for group (control or experimental), time point (baseline or deflation) and group-time point interaction.
A scatter plot was used to assess visually whether Phillips and Masimo values were similar. For the control sides at all time points and experimental sides at baseline and at deflation, we compared the means for the Phillips and Masimo perfusion index values using paired t-tests. We quantified the associations using Pearson’s correlation together with 95% confidence interval (CI) and intraclass correlation coefficient (ICC). For experimental sides, at inflation when trace was lost (timepoint 1) and during inflation (timepoint 2), because most values were close to zero, we compared Phillips and Masimo perfusion index values using Wilcoxon signed-rank tests. We quantified the correlation using the Spearman’s and Kendall’s correlations as there did not seem to be a linear relationship.
We analysed arms’ and legs’ data separately. Also, except when comparing Phillips and Masimo perfusion index values, we analysed Phillips and Masimo data separately.
All hypothesis tests were performed at 5% significance level. The figures were produced in R statistical program while models used to test hypotheses were fitted in SPSS (IBM, Chicago IL, USA).
Data were secured on a secure computer on the trust server. This was password protected and the excel spreadsheet (Microsoft corporation, Redmond, Washington, USA) was password protected.
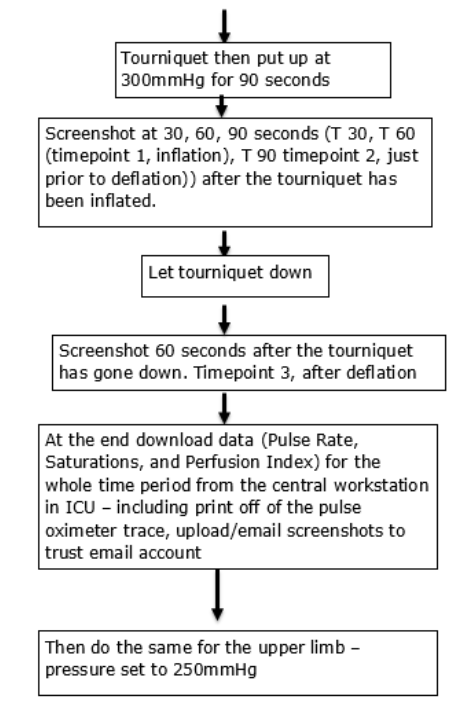
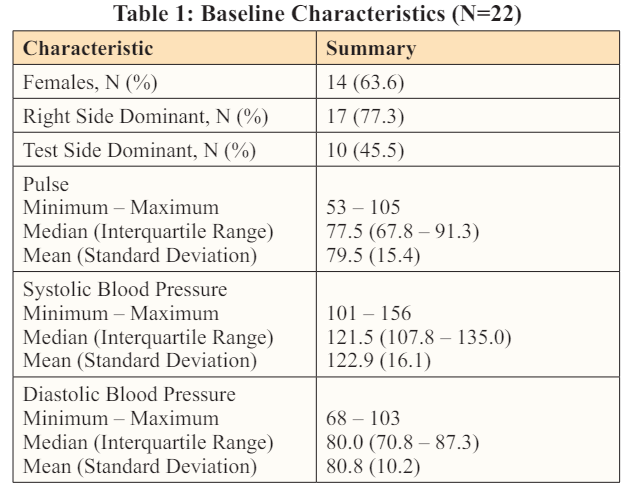
All respondents identified as female or male and there were more females (63.6%). There were no missing data. The right side was dominant for most participants (77.3%) with the dominant sides forming 45.5% of the test sides. The interquartile ranges (IQRs) for pulse, SBP and DBP were 67.8-91.3, 107.8-135 and 70.8-87.3, respectively (Table 1).
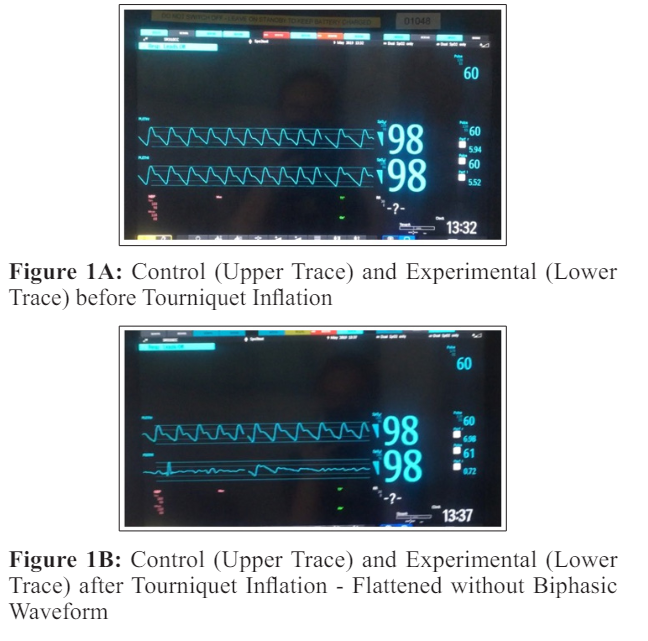
In both the arms and legs, the pulse oximeter trace initially showed a biphasic appearance (Figure 1a) prior to tourniquet inflation. As the tourniquet was inflated, the trace became monophasic and then lost amplitude completely (Figure 1b), which was the first change seen within 10 - 45 seconds of tourniquet inflation.
For both pulse oximeter probes, the perfusion index values were significantly lower in the experimental compared to control arms and legs during inflation (timepoint 1) at p<0.001 (Table 2, figures 2, 3, 4, 5).
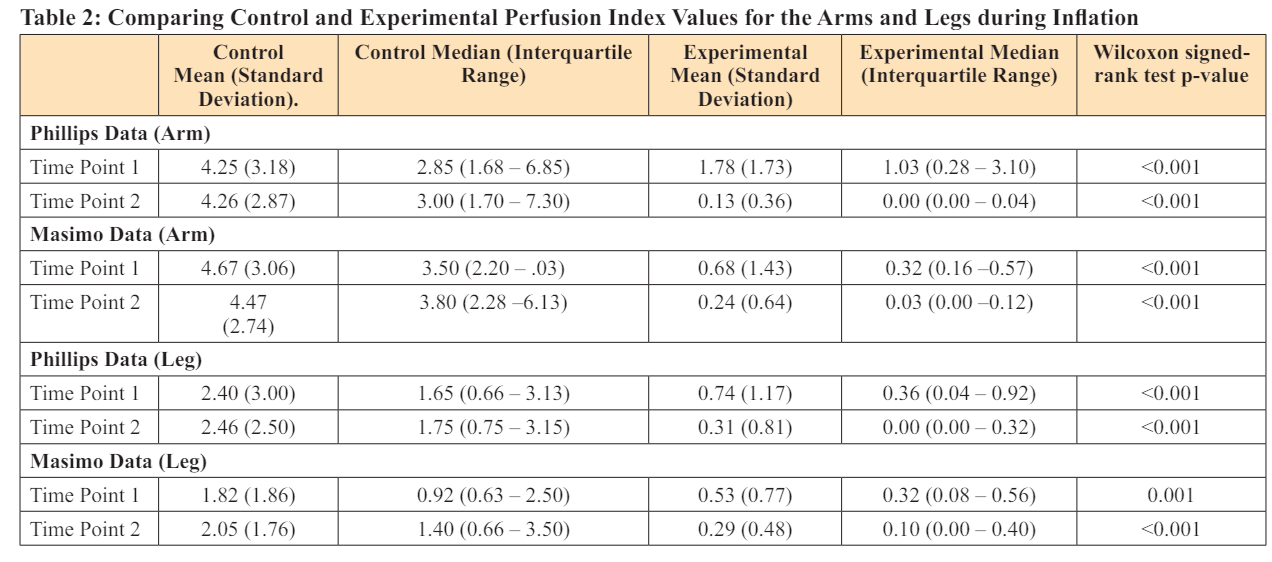
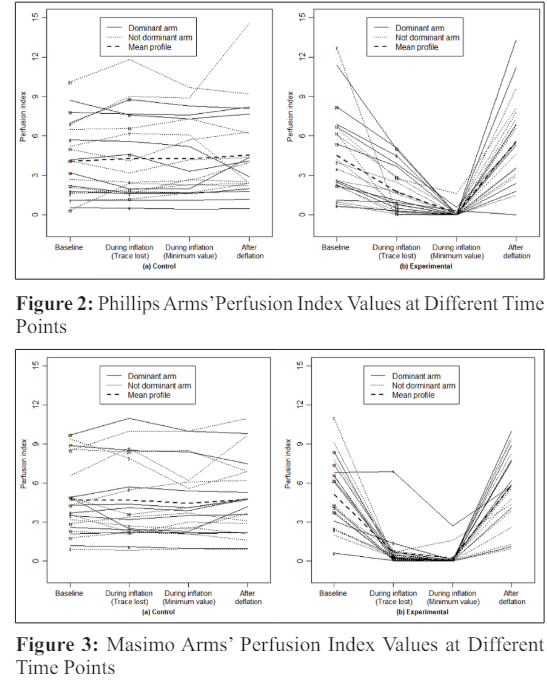
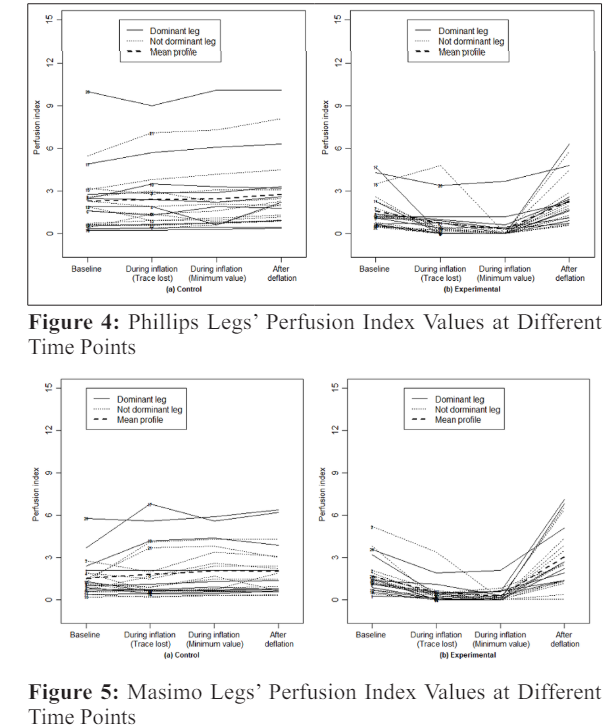
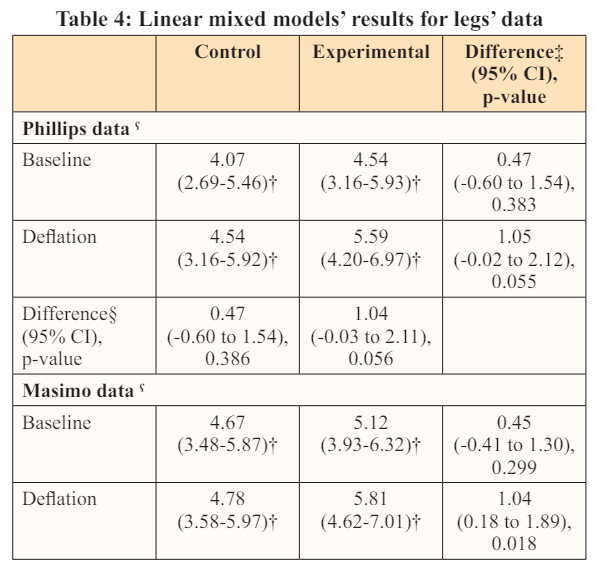
All the perfusion index values for control limbs are relatively equal across the time points for each participant. In the experimental limbs, Masimo values decreased quicker but Phillips minimum values are closer to zero. Masimo probes mirrored the decrease in perfusion quickly after tourniquet inflation, whereas the Phillips probes tended to have a slower responsiveness and then to record no perfusion. Compared to baseline values, experimental limbs tended to have larger increases in perfusion index than control limbs after deflation which would be consistent with the known phenomenon of hyperperfusion after a period of ischaemia (timepoint=3)(Phillips, difference=1.05, p=0.055; Masimo, difference=1.04, p=0.018) (Table 3 and 4).
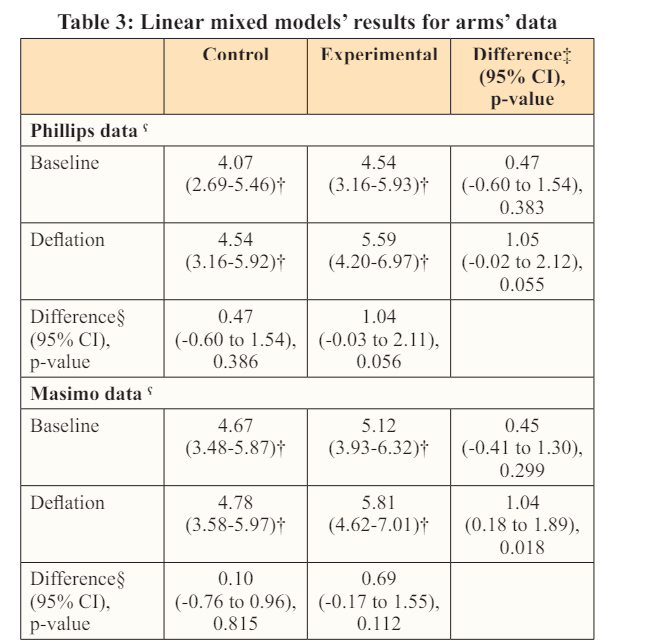
CI = Confidence interval; Separate models; † Mean (95% CI); ‡ Experimental - Control; § Deflation - Baseline
Oxygen saturations were initially 98 - 100% prior to tourniquet inflation. In some cases saturations were recorded for several seconds beyond the loss of the amplitude of the trace, at normal or reduced values (70 - 98%) but were then unrecordable during tourniquet inflation and returned to normal after deflation. Saturations were a less reliable indicator of tourniquet inflation than the pulse oximeter trace or the perfusion index.
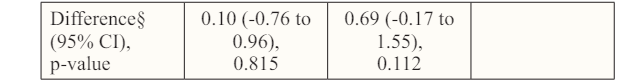
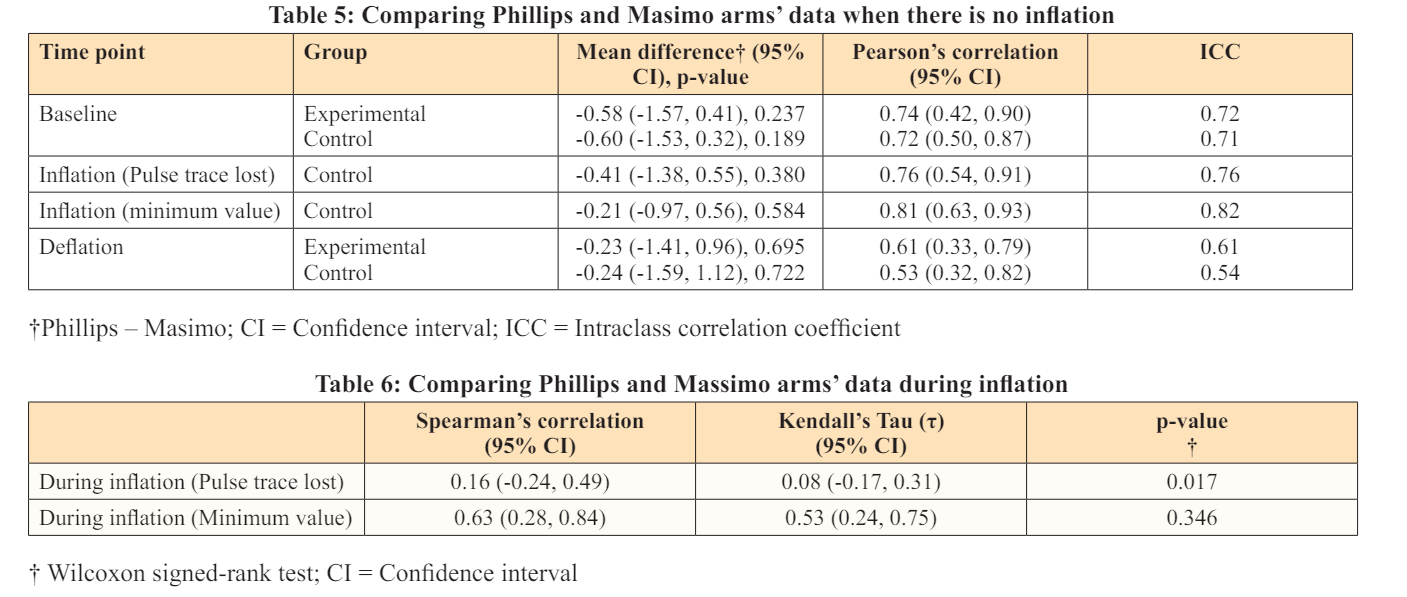
Comparing the two types of probe: Phillips and Masimo perfusion index measurements showed strong agreement for control limbs (Figure 6), indicating that they are clinically interchangeable, when there is no vascular compromise.
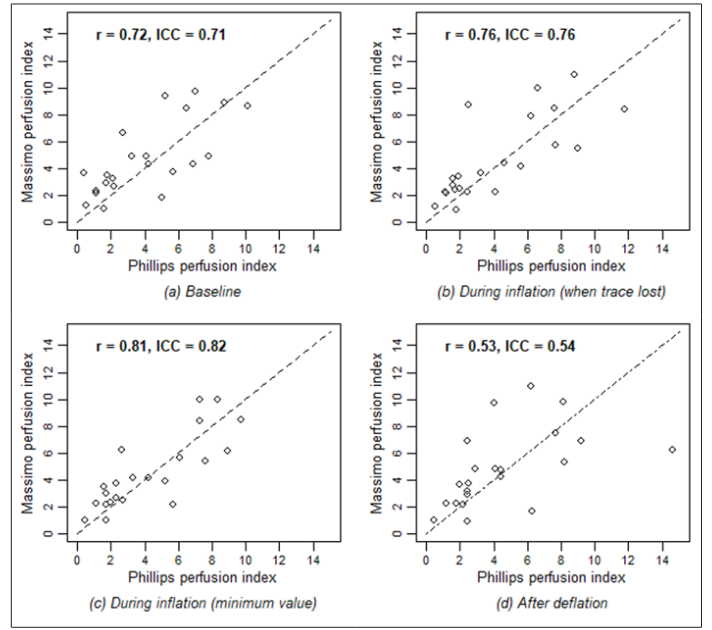
Figure 6: scatter plots for control sides phillips and masimo arms perfusion index values at different time points. The dashed line is the line of equal phillips and masimo values
The Masimo perfusion index reacted more quickly to the tourniquet inflation so at time point 1, there does not seem to be relationship between Phillips and Masimo perfusion index values in the experimental limbs (Figure 7 and Tables 5,6)
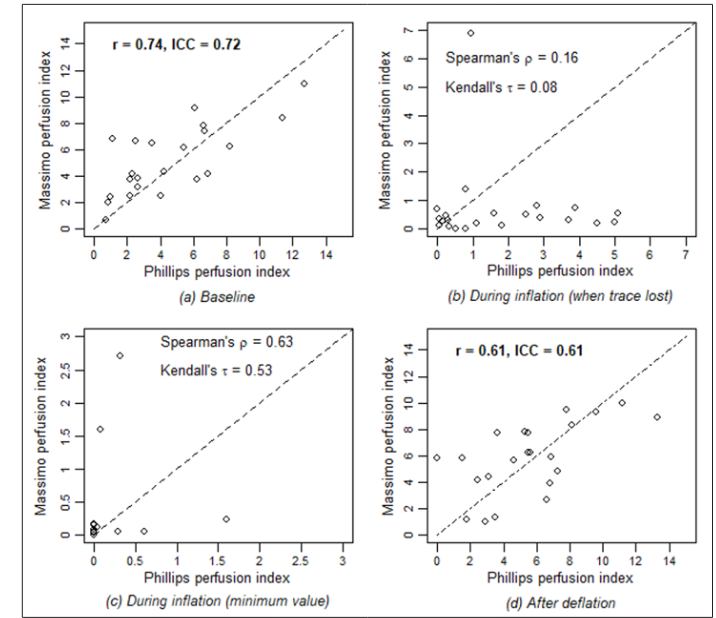
Figure 7: Scatter plots for experimental sides phillips and masimo arms perfusion index values at different time points. The dashed line is the line of equal phillips and masimo values
Also, the Phillips and Masimo values are statistically different (p=0.017) and Spearman’s correlation and Kendall’s Tau (t) are small with the confidence intervals including zero so that there is no agreement between Phillips and Masimo perfusion index values when the biphasic trace is lost. However, before deflation (timepoint 2), both Massimo and Phillips perfusion index are close to zero, therefore the Phillips and Masimo values are not statistically different (p=0.346) and both Spearman’s and Kendall’s correlations indicate moderate association. (Figures 8, 9 and Tables 7,8).
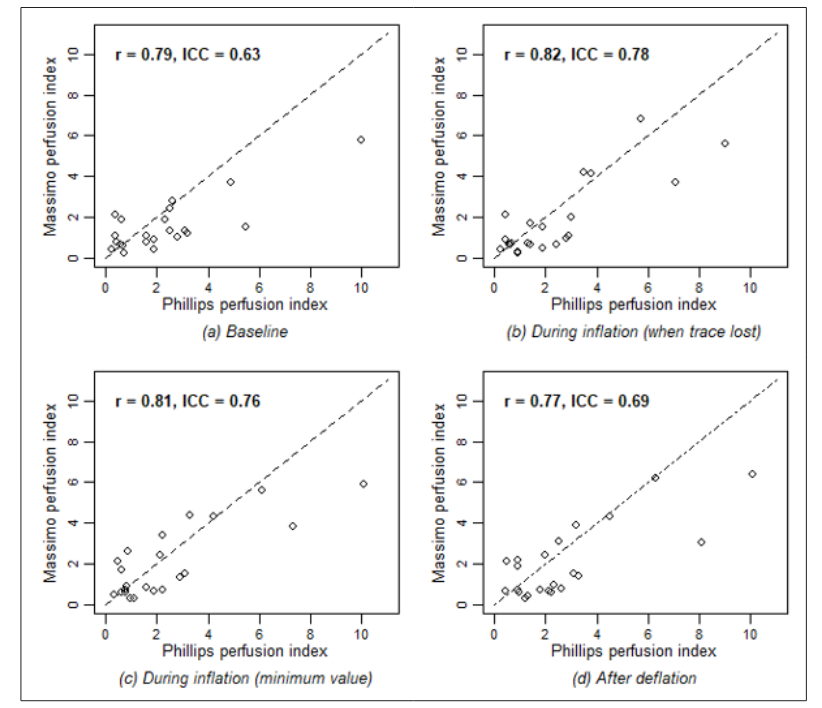
Figure 8: Scatter plots for control sides Phillips and Masimo legs’ perfusion index values at different time points. The dashed line is the line of equal Phillips and Masimo value
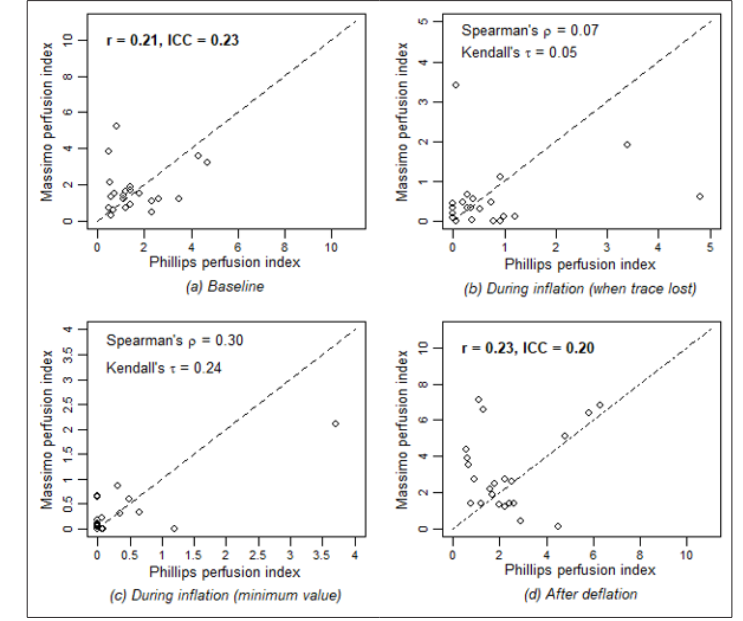
Figure 9: Scatter plots for experimental sides phillips and masimo legs’ perfusion index values at different time points. Dashed lines are lines of equal phillips and massimo value

The PULSE Study has demonstrated that the pulse oximeter trace is quickly responsive to changes in perfusion of the upper and lower limb, when it is manipulated by tourniquet inflation. The normal biphasic trace is lost first with 10 - 45 seconds of tourniquet inflation. This finding is consistent with observations in supratrochlear humeral fracture in children associated with complete division / occlusion or intimal damage to the vessel requiring surgical intervention. This study has shown that changes or absence of the biphasic waveform, when compared with the contralateral normal limb is a good indicator of vascular compromise.
The perfusion index is reduced during tourniquet inflation on both Masimo and Phillips pulse oximeter probes within 90 seconds of tourniquet inflation. Phillips pulse oximetry calculates perfusion by Fourier artefact suppression technology (FAST), which provides a numerical value for the pulsatile portion of the measured signal, with guidance that values of <0.3 are suboptimal, 0.3 - 1 acceptable and > 1 optimal. The Masimo probe uses the ratio of the pulsatile to the static blood in the peripheral tissues through signal extraction technology (SET) using 5 difference parallel algorithms, and an increase can indicate peripheral dilatation [8]. Ranges are given as 0.02% very weak to 20% very strong. In the clinical setting, reduced perfusion index would also indicate likely reduced perfusion and any effects of resuscitation, temperature, peripheral vasodilatation are likely to have similar effects on both limbs, so comparing the normal to the injured limb may help to control for these confounding factors. Our findings show that the Masimo probe responds more quickly, but the Philips measurements are closer to zero. However, in a clinical scenario, either probe will give the treating clinician an indication that perfusion is not normal, and that surgical assessment and exploration may be required.
The oxygen saturation is a less reliable indicator of reduced perfusion. It can be maintained for 30 - 60 seconds after tourniquet inflation and then may be unrecordable. It therefore should not be relied upon to give any indication about the adequacy of the circulation.
The methodology has been shown to be effective and repeatable in volunteers in this study. However, it has not been used in those with injuries, who may have confounding factors such as inadequate resuscitation and reduced circulating volume, hypoxia due to concurrent thoracic or abdominal injuries, anaemia or inadequately reduced fractures, vascular occlusion due to dislocation or intimal damage or compartment syndrome. However, this study has demonstrated the effectiveness of the pulse oximeter trace and perfusion index in diagnosing reduced perfusion quickly and noninvasively. Application of the pulse oximeter in clinical situations is planned for the primary assessment and management of the patients with lower limb injuries, dislocations or compartment syndrome. The technology is widely available in the resuscitation area of the Accident and Emergency department, in intensive care and in the operating theatre.
Clinical application of these findings may be useful in the assessment of potential vascular compromise in patients wih tibial injuries, compartment syndrome and native joint dislocations.
Thank you to all kind colleagues who gave up their time to contribute to this study.