Author(s): Amit Sharma*, Devesh Chauhan, Ashish Ranjan and Rushiraj Shinde
It is quite common in the practice of a pulmonologist to come across patients having pulmonary symptoms in the background of chronic kidneydisease (CKD). This is also owing to the fact that advances in the medical field such as haemodialysis result in significant prolongation of survival in these terminally ill patients. However, this leads to emergence of a newer plethora of systemic manifestations which require further investigation and management.
It is quite common in the practice of a pulmonologist to come across patients having pulmonary symptoms in the background of chronic kidney disease (CKD). This is also owing to the fact that advances in the medical field such as haemodialysis result in significant prolongation of survival in these terminally ill patients. However, this leads to emergence of a newer plethora of systemic manifestations which require further investigation and management.
The lungs are almost always affected in CKD due to pulmonary oedema (PE) which may have a heterogenous basis. Apart from the deranged oncotic pressure dynamics across the capillaries in such cases, toxin induced damage to the endothelial capillaries may also play a significant part in the accumulation of fluids in the lungs causing dyspnoea and distress to the patient [1]. To make matters worse, this fluid retention may be unresponsive to diuretics [2].
Pulmonologists are frequently receiving referrals from the Nephrologists in solving the conundrum of respiratory signs and symptoms (which are now more frequent) caused by the renal dysfunction and/or haemodialysis. Because of better survival, there may be novel thoracic radiological manifestations which may baffle the Chest Physician [3].
Chest-X-Rays of these patients may reveal a bat-wing pattern (peri-hilar infiltrates and sparing the peripheries) and cardiomegaly is usually absent. There may be numerous atypical presentations in the Chest radiographs of the CKD patients. Pleural effusions are very commonly seen and such patients are often referred to the Pulmonologist to rule out a tubercular aetiology, especially in the context of India where Tuberculosis (TB) is endemic. However, for a pulmonologist this represents a diagnostic challenge.

Figure 1: Uremic Pulmonary Edema
Moreover, the pulmonary manifestations of uraemia are not limited to pleura. With the widespread availability of Dialysis, CKD patients’ survival rates have improved considerably and due to this, more and more differing pictures in the lungs have emerged. Typical consolidation of a Pulmonary lobe which was almost completely consistent with Pneumonia turned out to be renal induced pulmonary oedema which responded very well to dialysis. The same authors demonstrated renal induced Pulmonary oedema mimicking malignant metastatic nodules as well as fungal infection [4].
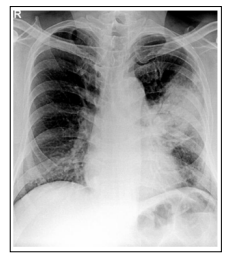
Figure 2: Uremic Pulmonary Edema Mimicking Consolidation

Figure 3: Uremic Pulmonary Oedema Mimicking Metastatic Nodules
Respiratory symptoms are common in CKD patients especially those who are undergoing dialysis. This may invariably lead to a chest radiograph being performed which opens the pandora’s box for the patient as well as the attending nephrologist, radiologist and the pulmonologist to whom the patient is referred. As mentioned above pleural effusions are commonly seen and are usually characterised by cough, fever and chest pain but breathlessness is not common. Pleural fluid may be Haemorrhagic or serosanguinous, lymphocytic exudate. Such effusions commonly disappear if the frequency of Dialysis is increased [5].
Involvement of the lungs is also quite commonly seen. A study which utilized Computed Tomographic (CT) of the lungs of such patients demonstrated atelectasis of the lungs as the most common finding, seen in 79.7% of cases. Lung fibrosis, pleural effusion and ground glass opacity was seen in 50%, 45.3% and 45% respectively [6]. This study also provided valuable inputs regarding the Cardio-vascular system with Cardiomegaly in 59.3% and enlarged pulmonary artery in 29.7% of the patients [7].
CKD patients undergoing haemodialysis are also prone to respiratory infections because of their immune compromised condition, most commonly due to Staphylococcus Aureus (27%) and Mycobacterium Tuberculosis (13%) as per the following studies [8]. These may show up radiologically as consolidation, mostly patchy but there may be well-defined lobar opacity in few cases. The sputum should be obtained in these patients which may be stained for Acid fast bacilli (AFB) and put up for pyogenic and mycobacterial cultures, so that proper antibiotic or anti-tubercular treatment may be initiated.
The administration of antibiotics is also challenging as certain drugs cannot be administered such as the aminoglycosides and for many other drugs, the dosage or frequency of administration needs to be reduced. For instance, the daily dosage of ethambutol, an anti-tubercular drug, may be given thrice weekly after dialysis in such patients because of the fact that ethambutol is eliminated from the body by renal clearance physiologically
The treatment of the pulmonary manifestations of CKD patients on dialysis such as pleural effusion and pulmonary oedema, which may manifest as a bat-wing appearance centrally and with hyperlucent periphery along with ground glass appearance and at times as consolidation and nodular opacities, may simply be done by increasing the frequency of the haemodialysis, which usually clears the Lungs. A patient’s non-compliance regarding fluid restriction may also be an underlying factor for Pulmonary Oedema in such patients’ which needs to be addressed diligently.
Pleural effusions in such patients should also alert the pulmonologist to be vigilant about pericardial effusions because non-resolution of such effusions may lead to fibrinous pericarditis and/or pleuritis. This may ultimately form a fibrous peel around the lungs and the heart leading to restrictive heart and/or lung disease which can cause Congestive heart failure and disabling dyspnoea due to restrictive Pulmonary volumes. Surgical removal of the rind in such cases may be the only option for such patients.
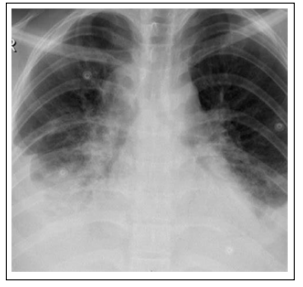
Figure 4: Uremic Right Sided Pleural Effusion
However, some radiological signs such as pleural effusion, consolidation and persistent cough not responding to the increased dialysis may also be due to underlying infection such as Tuberculosis which is endemic in our country. Tapping of pleural fluid showing increased levels of adenosine deaminase (ADA) may necessitate the initiation of Anti-Tubercular therapy (ATT). In cases of cough, fever and/or expectoration, sputum examination may reveal the presence of Mycobacterium Tuberculosis (MTB) either by direct staining, genotypic (cartridge- based nucleic acid amplification test - CBNAAT) and phenotypic (liquid culture) methods. Amongst the major anti-tubercular drugs, aminoglycosides (Streptomycin, Amikacin etc.) are contra-indicated due to their known nephrotoxic potential. Ethambutol is cleared by the kidneys and decreased frequency of dosing as described earlier should be adhered to.
To conclude, because of increased longevity of CKD patients due to widespread availability of dialysis facilities, novel patterns of thoracic clinico-radiological are emerging which prove very challenging to the Pulmonologists and a liaison between the nephrologist, radiologist and pulmonologist should be maintained for optimum management of this group of patients.
