Author(s): Frederick Tshibasu Tshienda*, Jean Mukaya Tshibola, Patrick Lebughe Litite*, Cynthia Minouche Bokumba, Nancy Moyo Kafundu, Michel Lelo Tshikwela, Wafa Mbarki, Tasnime Hamdeni, Mounir Sayadi, Luc Mokassa Bakumobatane, Antoine Tshimpi Aole, Hippolyte Nani Tuma Situakibanza, Jean- Marie Kayembe Ntumba, Jean-Jacques Malemba and Jean-Marie Mbuyi Muamba
Objective: Consist of making an inventory of the indications for lumbar spinal MRI in the diagnostic management of lumbar spinal pathologies in hospitals in Kinshasa and Brazzaville. About 302 patients.
Materials and Methods: This was a retrospective, documentary and multicenter study on 302 patients who underwent lumbar spine MRI examinations in 18 months in hospitals in Kinshasa and Brazzaville.
Results: The mean age of patients was 53.4 years. The most represented age group was 50 to 59 years old. The female sex was predominant (55.4%) with a ratio of 0.79. The majority of patients (68.2%) came from Kinshasa. Lumboradiculgia was the most represented indication (49.3%) followed by low back pain (48%). The majority of MRI examinations (91.4%) were performed without injection of contrast product. T1 and T2 weightings were performed in 100% of patients. Degenerative disc disease was found at (41.7%) and lumbar disc herniation at (27.2%). The MRI examination was normal in (47%) of the patients. Based on potentially clinically positive relevance, only 48.7% of our MRI diagnose were clinically positive. Age (p=0.000), lumboradiculgia (p=0.000) and specialist physician prescription (0.039) had a statistically significant relationship with clinically positive diagnosis.
Conclusion: The use of lumbar spinal MRI examination was inappropriate in our study; this opinion mostly corroborates the observations of the literature. A codification of lumbar MRI indications in the radiological exploration of lumbar spinal disorders would avoid abusive and expensive prescriptions for a study population with low economic income.
Since antiquity, the idea of observing the interior of the human body with Hippocrates, Archimedes and many others has always fascinated man [1]. The discovery of X-rays in 1895 by Roentgen with its applications in radiography and computed tomography; made it possible to observe the interior of the human body. And for a very long time, spine imaging was based on conventional radiology (radiography, myelography and arteriography). This is limited in interpretation by the overlapping of bone structures and its difficulty in exploring the spinal and para-spinal soft tissues [2]. The use of standard or digital radiography in the exploration of the lumbar spine has limited value. At the end of the last century, we witnessed the emergence of new crosssectional imaging techniques, in particular computed tomography (CT) and magnetic resonance imaging (MRI). The advent of MRI; non-irradiating technique of medical imaging using the physical properties of hydrogen has transformed the diagnostic approach to spinal pathologies thanks to its sensitivity, its better contrast resolution and its ability to carry out a multiplanar study of the spinal container and content. MRI is currently the gold standard in the combined exploration of spinal content and container, for the orientation of treatment and patient followup, including in children and pregnant women [3, 4]. If in 2013 and 2017, France alone had around 650 and 906 MRI machines installed throughout its territory; in Africa, on the other hand, in 2007, WERNER and Al, counted a total of 89 MRI machines distributed unevenly across the continent with a concentration of machines at both ends of the continent [5]. In the DRC, the first MRI device was installed in 2013 at the Cinquantenaire Hospital, ten months later the second device was installed; the country currently has ten devices. Perhaps the most common findings on MRI images are degenerative changes in the lumbar spine such as degenerative disc disease, Zygarthrosis, herniated disc and narrowed spinal canal. These findings, however, are common in symptomatic and asymptomatic adults and are weakly associated with low back pain [6-8]. Epidemiological studies have found that excessive imaging for back pain is associated with increased spinal medication and surgery [9]. In Africa and particularly in the DRC and Congo-Brazzaville [10,11]. A number of clinical guidelines or strategies, such as red flag marking, appropriateness criteria (ACR), radiological benefit management (RBM), and clinical decision support systems have been developed [12]. To improve the appropriate use of MRI examinations in the investigation of back pain. Despite decades of effort to transfer scientific knowledge to clinical practice, one to two-thirds of spinal MRIs have been found to be inappropriately prescribed in the U.S.A [13]. Little attention has been given to the exploration of lumbar spinal complaints in the health system of the DRC and Congo-Brazzaville; hence the need for the present study, consisting in establishing an inventory of the indications for lumbar spinal MRI in the diagnostic management of lumbar spinal pathologies in hospitals in Kinshasa and Brazzaville.
Nature of the Study: We carried out a documentary and descriptive study from March 2019 to March 2020, i.e. a period of twelve months, and from December 2020 to June 2021, i.e. a period of six months.
This is a multicenter study conducted simultaneously in Kinshasa at the NGALIEMA Clinic and in Brazzaville at the COGEMO Medical-Surgical Clinic in the radiology departments. The latter have an average daily attendance of 55 patients. At the Ngaliema clinic, we used a Philips brand MRI machine, ACHIEVA type, closed field with 1.5 Tesla permanent magnet manufactured in 2012, acquired in 2014 and put into service in 2016. On the other hand, at the Medico-surgical clinic (COGEMO) of Brazzaville, we used a HITACHI brand MRI device, Type AIRIS COMFORT II, open field with 0.35 Tesla permanent magnet manufactured in 2004, commissioned in 2006 and acquired in 2016. As exploration protocols: The different protocols were adapted to the pathology sought, but generally the standard protocol for MRI examinations of the lumbar spine comprising sagittal T1 spin echo (SE), T2 spin echo (SE), T2 STIR and axial T2 spin echo sequences. A slow direct intravenous injection of 0.1 mmol/kg or 0.2 ml/kg of Gadolinium was sometimes used in some patients to study the enhancement kinetics of the lesions observed. The duration of the examination was generally 20 to 30 minutes. The usual precautions and the various contraindications were strictly applied before any MRI examination.
were included in the present study; any male or female patient, aged at least ten to ninety years, of Congolese nationality (from the DRC and Congo Brazza) who has performed a lumbar spinal MRI and whose reports include all the variables interests sought; among other things: the complete identity of the patient, the anthropometric parameters (age and sex), the indication for the examination, the detailed radiological semiology as well as the conclusion. The following were not excluded in the present study: any patient with an incomplete file or not having MRI images on the PACS systems, any patient aged under 10 years or over ninety years old, at the end of having been outside the period.
Data collection was carried out on the basis of photocopied reports of lumbar MRI examinations carried out during the study period as well as the D.V.D of the images engraved for each patient from their archiving system , including IQ-Views on behalf of Brazzaville and Vision PACS on behalf of Clinique Ngaliema. The data was recorded and processed in a Microsoft Excel 2013 file. The parameters studied were: socio-demographic characteristics of the study population, indications for lumbar MRI examinations, MRI diagnoses, exploration technique and the profile of prescribing physicians. 2.5 Operational definitions.
Were considered to be: A normal MRI: Mild disc degeneration: less likely to produce clinical symptoms [14]. Were considered to be: Pathological MRI: Disc degeneration Disease: (degenerative disc disease): significant decrease in disc signal intensity, significant disc narrowing or disc bulging with or without compression of the nerve root or dural sheath such as evaluated on the T2 axial sequence. Disc herniation: focal disc protrusion from the nucleus pulposis through the uni or bilateral annulus fibrosis, with or without root compression. Foraminal disc herniation: was judged from a sagittal image with significantly narrowed intervertebral foramen and nerve root compression. Lumbar spinal canal stenosis: This is an acquired or congenital narrowing of the central spinal canal or lateral recesses. Central stenosis: antero-posterior diameter less than half that of the underlying stage. Lateral recess stenosis: narrowed lateral recess with compression of the nerve roots Foraminal stenosis: narrowing of a conjugation foramen likely to cause compression of the nerve root. Spondylolisthesis: sliding of the upper vertebra relative to the lower vertebra on sagittal views. Spondylodiscitis: significant modification of the IVD signal, of the vertebral bodies with or without structural damage, more or less associated with an abscess of the paraspinal soft tissues. Zygarthrosis: degenerative rearrangements of the posterior articular apophyses with hypertrophy of the articular masses and narrowing of their joint spaces. Spinal and intraspinal tumours: bone, epidural, intra-dural extra-medullary and intra-medullary tumours. Vertebral fractures: only fresh vertebral fractures were included with decreased signal intensity on T1 and increased signal intensity on T2. Fat deposits: defined by fatty degeneration of the spongy bone. Zygapophyseal and dural sac cysts: which are fluid signal tumor formations (hypo T1 and Hyper T2) as well as bone angiomas: were considered as incidentaloma, therefore excluded from the present study. All available MRI images were evaluated from the IQ-Views archiving system and Vision PACS to make the final diagnosis at lumbar spine MRI. Definition of the potentially and clinically positive diagnosis: the diagnosis was classified as potentially and clinically positive, before any compression of the root or the dural sheath that may require clinical interventions. The following were defined as potentially positive from a clinical diagnostic point of view: conflictogenic degenerative disc disease, zygarthrosis with osteoradicular conflict, conflictogenic disc herniation, lumbar spinal canal stenosis, spondylolisthesis, spinal and intra-spinal tumours, spinal infections(spondylodiscitis), axial spondyloarthropathy, as well as fresh vertebral fractures. Were defined as potentially clinically diagnostically negative; any situation outside of those listed above.
The data collected was analyzed and processed using SPSS 27.0 software. The different data were subjected to a univariate, bivariate and multivariate analysis. With regard to the univariate analysis, the data were summarized in the form of tables or graphs for the categorical variables and the mean and its standard deviation or the median and its interquartile range depending on whether the distribution is symmetrical or not. In addition, for the bivariate analysis, the Pearson or Fisher exact Khi2 test was used to establish the relationship between the clinically potentially positive diagnosis and the variables retained in the study at the 5% threshold depending on whether the frequencies observed are greater than 5 or not. Finally, for the multivariate analysis, binary logistic regression was used to identify the factors associated with the clinically potentially positive diagnosis.
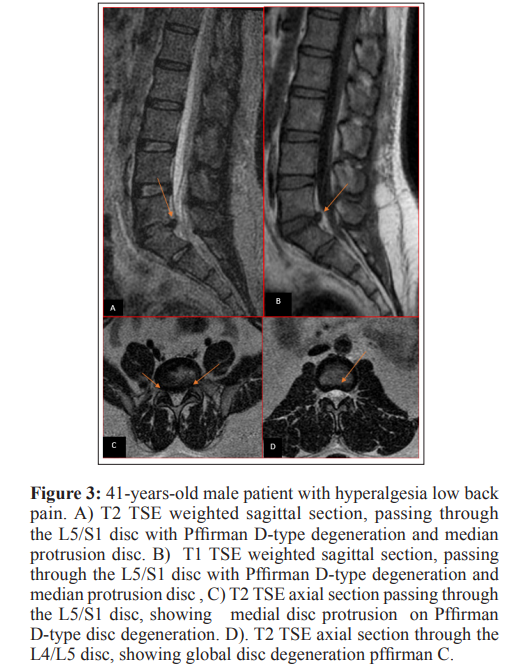
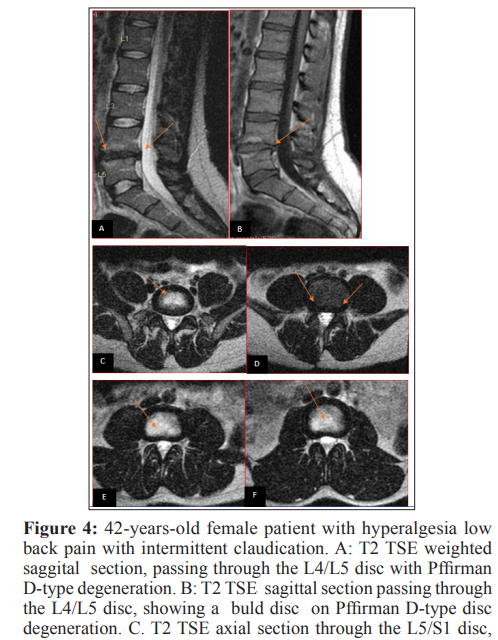
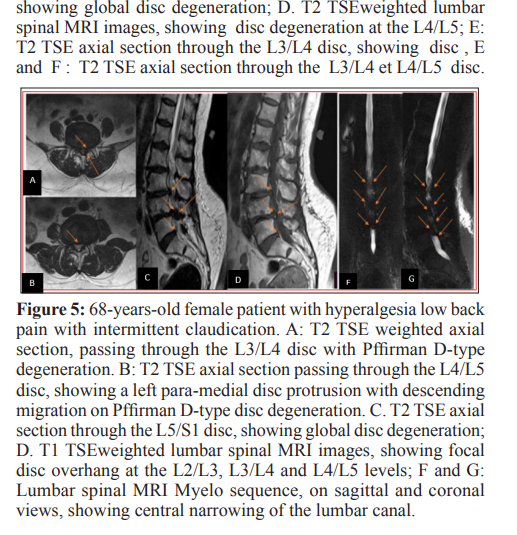
In relation to sociodemographic characteristics, three hundred and twenty lumbar spinal MRIs were recorded during the study period, including 44.4% men and 55.6% women, i.e. a sex ratio of 0.79% (Figure: 1 and Table I). The age of the patients ranged from 10 to 91 years with an average age of 53.4 years; a standard deviation of 13.9 years. The 50-59 age group was the most represented with 27.2% (Table I, Figure 2). The majority of women were between 40 and 49 years old, i.e. 26.2% of all women (Table I). In addition, 33.6% of men are between 50 and 59 years old (Table I). Regarding the origin of the patients; nearly two-thirds of the patients (61.3%) came from Kinshasa and 38.7% from Brazzaville (Table III). As for the indications for lumbar spinal MRI, it should be noted that clinically: 49.3 % of patients were referred for lumboradiculalgia; among these patients: 41.7% presented isolated lumboradiculalgia and 7.6% presented lumboradiculalgia associated with deficit neurological disorders, such as neurogenic claudication, followed by low back pain in a proportion of 48% including 1.3% associated with deficit neurological disorders ( Table II) Of all the women, 44% had isolated lumboradiculalgia and 7.7% lumboradiculalgia associated with deficit neurological disorders. In addition, of all the men: 38.8% had isolated lumboradiculalgia and 7.5% lumboradiculalgia associated with deficit neurological disorders (Table II). Referring to the technical data; it turns out that more than three quarters (91.4%) of lumbar spinal MRI examinations were performed without injection of the contrast product (Table III). In addition, T1SE, T2SE and T2 STIR weighted sequences were performed during all MRI examinations. The majority of physicians prescribing lumbar spinal MRI examinations in this series were specialist physicians (63.1%) (Table III). Regarding the diagnostic interpretation according to the MRI diagnostic criteria set in this study, we noted a predominance of normal MRI examinations around (47%), followed by degenerative disc disease (41.7%) including 79% conflicting and 21% non-conflicting (Table IV) and herniated disc (27.2%) including 89% conflicting and 11% non-conflicting (Table IV). In the majority of cases the degenerative disco-vertebral changes were conflicting (79%) and therefore potentially clinically significant. Based on potential clinical relevance, using our definition of potentially clinically positive diagnosis, only 48.7% of all lumbar spine MRI scans were considered potentially clinically positive diagnosis (Tables: V-VI). The remaining 51.3% results were considered clinically negative (Table V-VI). Analysis of factors associated with the rate of potentially clinically positive diagnoses; shows that the majority of patients, i.e. 30.6%, whose age is between 50 and 59 years old, had obtained a potentially clinically positive diagnosis (Table V-VI). In addition, there was a statistically significant relationship between age and potentially positive diagnosis (p=0.000) (Table V-VI). As for gender, in our entire series, 52.4% of women had a potentially clinically positive diagnosis (Table VI). Furthermore, there is no statistically significant link between sex and potentially clinically significant diagnosis (p=0.161) (Table VI). In relation to the indications, 76.9% of the patients in our study referred for lumboradiculalgia (61.9% isolated and 15% associated with deficit neurological disorders) had a potentially clinically positive diagnosis (table V-VI). There is a statistically significant relationship between lumboradiculalgia and potentially clinically positive diagnosis (p=0.000) (Table V-VI). Regarding origin, 66% of patients from Kinshasa had a potentially clinically positive diagnosis (Table V-VI). There is no statistically significant link between the origin of the patients and the potentially clinically positive diagnosis (p=2.247) (Table V-VI). For the profile of prescribing physicians, it was noted that 66.7% of patients referred by specialist physicians had a potentially clinically positive diagnosis (Table V-VI). Specialist prescribers were statistically significantly associated with a higher rate of potentially clinically positive lumbar MRI results (p=0.039) (Table V-VI). factor associated with potentially clinically positive diagnosis (Table V). Indeed, there is 10 times more chance for the patient with radiculalgia to have a potentially clinically positive MRI diagnosis compared to those with low back pain (OR=10.179; p=0.008) (Table V). In addition, there is 84 times more chance for the patient with lumboradiculalgia to have a potentially clinically positive MRI diagnosis compared to those presenting with low back pain (OR=84.238; p=0.000) (Table V). There is 11 times more chance for the patient presenting low back pain associated with deficit neurological disorders to have a potentially clinically significant diagnosis compared to those presenting isolated low back pain (OR= 11.091; p=0.000); this may be due to the fact that most of the deficit neurological disorders in our series were related to a narrowed spinal canal which is a clinically significant diagnosis (Table V).
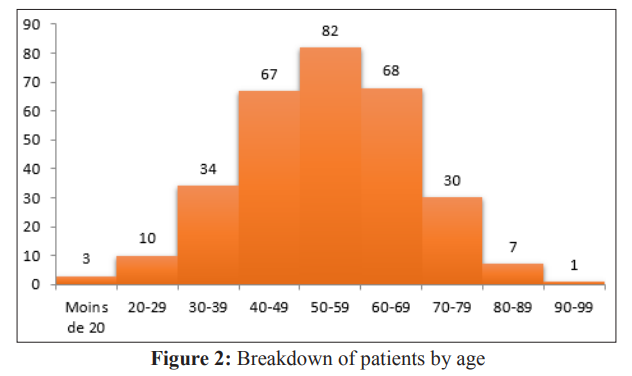
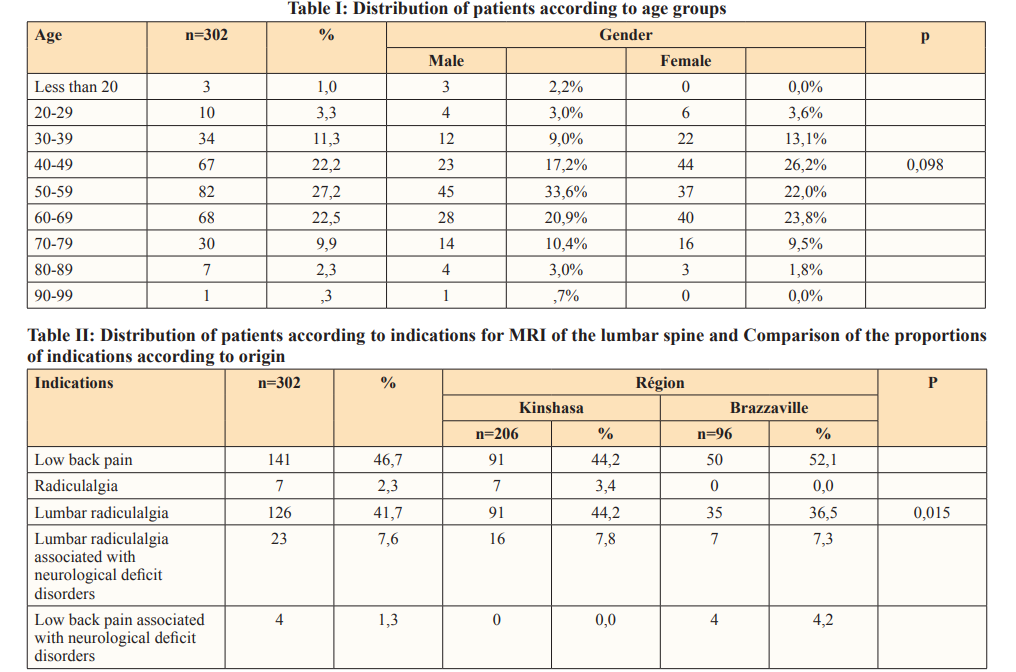
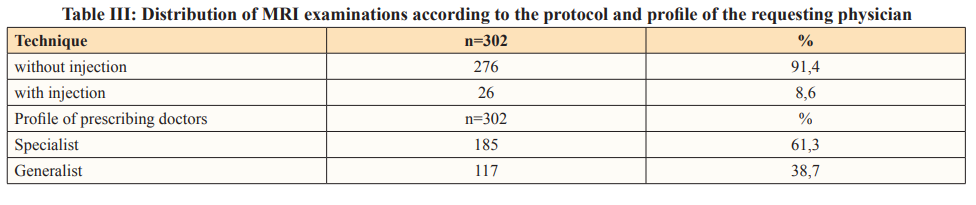
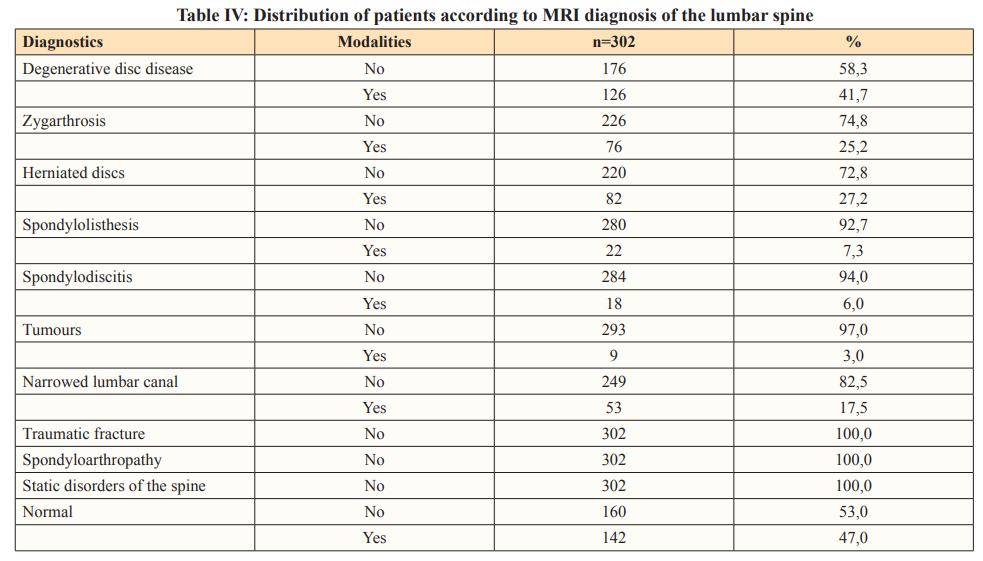
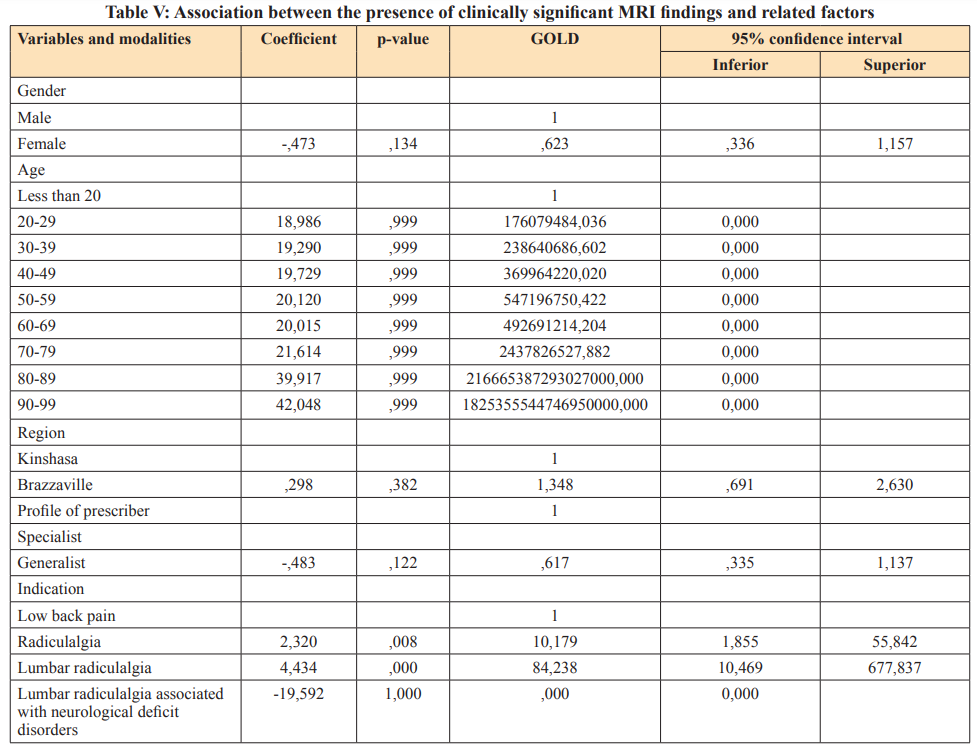
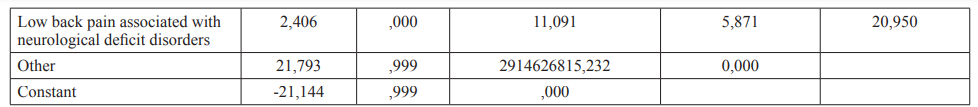
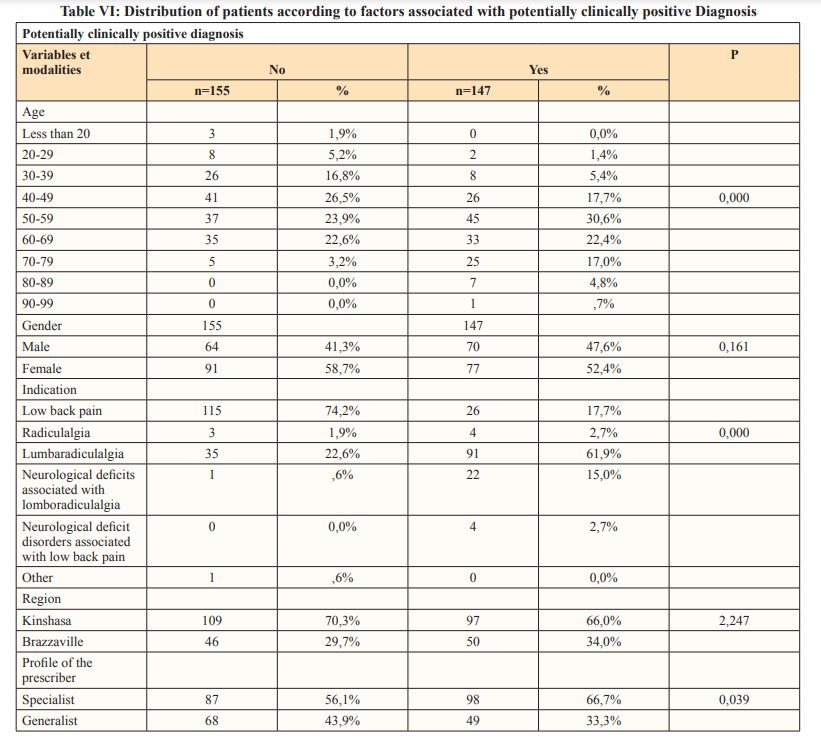
Methodological approach: the present study is a retrospective survey whose interest was to make an inventory of the indications for lumbar spine MRI in the diagnostic management of lumbar spine pathologies in hospitals in Kinshasa and Brazzaville. Sociodemographic profile. Sex: the distribution of patients by sex shows a predominance of the female sex with 55.4% against 44.6% male, i.e. a sex ratio of 0.79. Data from the literature also show a female predominance, like Gourmelin in France, who reported a sex ratio of 0.79 [15]. Our results are similar to those of Kpadonou in Benin, Ntisiba in Congo and Solange in Cameroon [16–18]. Debbabi in Tunisia and Raid in Morocco also found a female predominance among health workers, respectively at 51.6% against 48.4% for men and 73.8% against 26.1% [19,20]. This clear female predominance in all these series could be linked to the great arduousness of the tasks developed to women in the two countries, associated with the great multiparity without forgetting their morphotype characterized by lumbar hyperlordosis; which may justify the high frequency of lumbar spinal complaints in women, African women in particular. However, these results differ from those of Millogo in Burkina Faso where the male sex predominated with 66.1% against 33.8% for women [21]. This discrepancy could be explained by the fact that the study population of Millogo consisted mainly of workers dedicated to heavy work handling the local factories. The majority of our patients were between 40 and 49 years old. These data are similar to those in China [22]. This could be explained by the fact that women in this age group considered to be active consult the doctor relatively more in the face of complaints considered to be more or less bothersome or persistent than much older women. Age: It appears from this study that the average age of the patients was 53.4 years with extremes of 10 years and 91 years. Of the 302 patients included, 82 (27.2%) were in the age group of 50 to 59 years. These results are similar to those found by in the Netherlands who respectively reported an average of 52.7 years with extremes of 3 to 100 years and 49 .9 years with extremes of 19 and 80 years [22,23]. Our data are also close to those in Togo who reported that the age group of 50 to 59 years was the most represented in 29.3% [24]. Our results are however different from those in Denmark who reported a mean age of 41.6 years with extremes of 18 and 60 years [25]. This discrepancy is explained by a difference in the methodological approach; indeed, if we conducted our study within the general population, the latter had as its source population elite riders from the city of Zurich, assumed to be sportingly active young adult subjects. Origin: The majority of patients in our series, 206 or 68.2%, came from Kinshasa. This can be explained by the fact that the duration of the study in Kinshasa was longer or shorter than that of Brazzaville, thus determining the different sample sizes. Indications for MRI of the lumbar spine. Clinically, it was reported in our study that lumboradiculalgia constituted the most predominant indication with 49.3% of which 41.5% in their isolated form, 7.5% associated with neurological deficit disorders, followed by low back pain. With 48% including 46.7% in their isolated form and 1.3% associated with neurological deficit disorders and radiculalgia with 2.3%. Our results are close to those in Sweden who reported in their series a predominance of lumboradiculalgia with 43% [26]. However, our data are different from those found in the series by in China, which places low back pain in first place with 40%, followed by lumboradiculalgia with 27.7% [22]. This difference could be explained by a lack of in-depth physical examination aiming to objectify lumboradiculalgia by resorting in particular to root stretching tests on the part of the prescribing physicians in our series. Our results are lower than those found by Tshibasu F in D.R. Congo who reported in his series an overall rate of lumboradiculalgia at 73.2% in all its clinical characteristics [27]. This difference could be justified by the fact that the latter’s study population only included patients with lumbar disc herniations. Epidemiological studies specifically investigating the population affected by lumboradiculalgia are rare and do not allow a comparison to be made with the data collected in this study. Only the overweight tendencies seem to correspond to the data found in the literature. Nevertheless, a review of the epidemiological literature in 2008 reported a lifetime prevalence of lumboradiculalgia ranging from 1.2% to 43% [28]. Of the 149 patients (49.3%) referred to MRI of the lumbar spine for lumboradiculalgia, 43 (28.8%) were between 50 and 59 years old and 87 (51.7%) were female versus 62 (46.3%) male. This female predominance in lumboradiculalgia could be explained by the fact that most African women are housewives and therefore subject to a sedentary life exposing them to excess weight which is one of the risk factors linked to the occurrence of lumboradiculalgia. These data are contrary to those in France, which reported in its series a male predominance of 55.7% against 44.3% of women [28]. This discrepancy can be explained by the difference in lifestyle in relation to the socio-professional profile of women in these two contexts.
In Togo in their study on the prevalence of neuropathic pain in patients suffering from common lumboradiculalgia also reported that the age group of 50-59 was the most represented in 29.3% [24]. Technique and protocol of MRI examinations. It appears from our study that the MRI examinations without injection of the contrast product were more represented and the T1SE, T2SE and T2STIR sequences were performed during all the examinations. Our data are similar to data from the literature which report that the injection of the contrast product during MRI examinations was reserved only for special cases, in particular when a tumor or infectious disease was suspected. MRI diagnosis; It appears from our study that normal MRI was commonly found followed by disc degeneration and then disc herniation. Our results are similar to those in China [22]. However, the data of our series are contrary to those of the literature which reports degenerative disc disease as the most frequent diagnosis in MRI of the lumbar spine and to those found in the series in the Netherlands which reported only 6% of normal results [23]. This discrepancy could be explained by the methodological difference with regard to the criteria for defining the MRI diagnosis used in our series; indeed, if in our series mild to moderate discovertebral degeneration was considered normal, in the literature and in the series of authors cited above, all degenerative anomalies, whether mild or moderate, are considered to be pathological. Factors associated with clinically positive MRI diagnosis. Sex; In this series, the female gender was predominant with a ratio of 0.79. Despite this female predominance, female sex was not significantly associated with clinically positive MRI diagnosis (p= 0.161). Our data differ from those in China [22]. Who reported a statistically significant relationship between gender and clinically significant MRI diagnosis. This difference could be explained by the larger study population in the series China [22]. Age: the majority of patients in the age group of 50 to 59 years most represented in our study, i.e. 30.6%, had a potentially clinically significant MRI diagnosis. Our data reveal that an age trend had a statistically significant relationship with a high rate of clinically positive diagnoses (p=0.000). The same observation was made [22]. We do not have any literature data on this. Indications: Clinically, the data from our study reported that lumboradiculalgia was the predominant indication for MRI examinations of the lumbar spine, followed by low back pain, neurological disorders deficits and radiculalgia. Moreover, in our series, apart from low back pain, all the other complaints that indicated MRI examinations with a clear predominance of lumboradiculalgia were factors significantly associated with the existence of the clinically positive MRI diagnosis (OR=84,238, p= 0.000). Indeed, there is 84 times more risk for the patient with lumboradiculalgia to have a potentially clinically positive MRI diagnosis compared to those presenting with lumbago (OR=84.238; p=0.000). In addition, there is a 10 times greater risk for the patient presenting with radiculalgia to have a potentially clinically positive MRI diagnosis compared to those presenting with low back pain (OR=10.179; p=0.008). Finally, there is 11 times more risk for the patient presenting low back pain associated with deficit neurological disorders to have a potentially clinically significant diagnosis compared to those presenting isolated low back pain (OR= 11.091; p=0.000). These data are similar to those. in China [22]. Who reported in their series a statistically significant association between lumboradiculalgia (OR= 18.423, p=0.002), radiculalgia (OR = 14.326, p=0.083) and neurological deficit disorders (OR=12.214, p=0.001) at a high rate of clinically positive MRI diagnosis; moreover, the low back pain was not related to it [29]. In Great Britain also reported in their study on the clinical presentation of low back pain and association with risk factors according to the results of magnetic resonance imaging that low back pain and neurological deficit disorders were all two significantly associated with deviation/compression of the nerve roots (OR=2.5; OR=1.8), therefore with a significantly positive MRI diagnosis. Most of the studies, especially those [30–32]. Confirm that the presence of lumboradiculalgia and deficit neurological disorders were factors associated with the existence of a clinically positive MRI diagnosis. Origin: Our study shows that there were more patients from Kinshasa than from Brazzaville. Furthermore, the origin of the patients was not a factor statistically associated with the clinically positive MRI diagnosis (p=2.247). Profile of prescribing physicians. Of all the patients in our series, the majority were referred by medical specialists against a minority referred by general practitioners. In addition, there is a statistically significant relationship between specialist prescribing physicians and clinically positive MRI diagnosis (p=0.039). These data are contrary to those found in the Netherlands [23]. Where general practitioners were significantly associated with clinically positive MRI diagnosis. This discrepancy could be explained by the fact that in the series of these last authors, all the doctors prescribing MRI examinations of the lumbar spine were general practitioners.
In Great Britain in their study on the diagnostic yield of MRI of the lumbar spine requested by general practitioners in comparison with specialist hospital clinicians reported a similar rate in the two groups [33]. This balance can be explained by the probable existence of adequate, widespread and continuous professional training, particularly in the management of spinal disorders.
Conclusion: It appears from this study that the majority of indications for lumbar spinal MRI examinations were inappropriate, due to the relatively low rate of clinically positive MRI diagnoses (48.7%). Most of the patients in our study were female (55.4%) with a ratio of 0.79, included in the age group of 50-59 years (27.2%), coming from Kinshasa. Lumboradiculalgia (49.3%) was the most common reason for indicating lumbar spinal MRI. As for requesters, the majority of request forms for lumbar spine MRI examinations came from specialist physicians The profile of prescribing physicians had a statistically significant relationship with a potentially clinically positive MRI diagnosis, however the rate of clinically negative MRI diagnosis was similar among medical specialists just as among doctors generalists. The majority of our MRI examinations had been carried out without injection of the contrast product. The most common diagnosis in our study was represented by degenerative disc disease. All indications except isolated low back pain were factors associated with clinically significant MRI diagnosis. Finally, it is important to recall not the diagnostic means in the face of spinal complaints, but also to remind clinicians of the different indications for lumbar spinal MRI in order to offer them in-depth knowledge in the end to allow them an efficient use of lumbar spine MRI.
Limitation of the Study: As a first limitation; we noted: - the use of a low-field MRI device (0.35 Tesla); indeed, the COGEMO Medico-surgical center which constituted our study framework in Brazzaville uses a 0.35 Tesla MRI device, with the corollary of a reduced spatial resolution; likely to compromise the fine detail of the Protection of Human and Animal: Rights The authors declare that this study did not involve experiments on patients, subjects, or animals. Confidentiality of Data: The authors declare that this study does not contain any personal data that could identify the patient or subject. Funding of the Study this study did not receive specific funding from any public or private institution.
Funding of the Study: This study did not receive specific funding from any public or private institution. Conflict of Interest Statement: All the authors do not have any possible conflicts of interest he images. These data are similar to those found by in China [22]. As a second limitation, we noted the great heterogeneity of the populations studied, including methodological differences that could negatively influence the results.
Contribution of our Study to Knowledge: This study is a retrospective survey with the mission of making an inventory not only of the indications, but also of the various lumbar spinal pathologies in hospitals in Kinshasa and Brazzaville. It is a first to highlight the relevance of the use of lumbar spinal MRI in the two capitals of two countries closest to the world. It not only revealed the overuse of lumbar spinal MRI in the two respective countries, but it made it possible to inventory the various lumbar spinal pathologies in hospitals in two cities.
Contribution and Responsibility of the Authors: 1. Frederick Tshibasu Tshienda: writing and proofreading. 2. Patrick Lebughe Litite: writing and proofreading, 3. Jean Mukaya Tshibola: writing and proofreading. 4. Michel Lelo Tshikwela: writing and proofreading, 5.Fidèle Nyimi Bushaba: proofreading, 6.Wafa Mbarki: proofreading, 6. Tasnime Hamdani: proofreading, 7.Mounir Sayadi: proofreading, 8. Hippolyte Nani Tuma Situakibanza: proofreading, 9. Luc Mokassa Bakumobatane: proofreading, 10. Jean-Jacques Malemba: writing and proofreading, 11.Jean-Marie Mbuyi Muamba, writing and proofreading.
Tables and figures: Figure I: Breakdown of the study population by gender, Figure II: Breakdown of patients by age, Table I: Breakdown of patients by age group; Table II: Distribution of patients according to indications for MRI of the lumbar spine and comparison of the proportions of indications according to origin; Table III: Distribution of MRI examinations according to the protocol and the profile of the requesting physician; Table IV: Distribution of patients according to MRI diagnosis of the lumbar spine; Table V: Association between the presence of clinically significant MRI findings and related factors. Table VI: Distribution of patients according to the factors associated with the potentially clinically positive diagnosis.
