Author(s): <p>Nijanth Manohararaj, Nicodemus Edrick Oey, Ei Mon Zaw, Chen Jing and Kappaganthu Venkatesh Prasanna*</p>
In terms of mortality and morbidity, spinal cord injury (SCI) is the second most frequent severe traumatic event globally, behind traumatic brain injury. SCI causes physical, psychological, social, and financial dysfunction not only to patients but also to their families. This review aims to highlight the most common potentially reversible medical issues faced by patients affected by SCI in the community so that they could be addressed early at the primary care level. In this narrative review, the leading causes of morbidity following SCI including cardio-pulmonary complications, bowel, and bladder-related complications and autonomic dysreflexia are presented with recommendations for their management. We explore the management of bone health-related, pressure injury-related complications and psychosocial aspects of care, and present recommendations to improve the quality of life of patients with SCI. Early detection and management of complications of SCI at the primary care level will help reduce the financial costs and psychosocial burden of this major cause of long-term disability.
Spinal cord injury (SCI) is the second most common severe traumatic event after traumatic brain injury in terms of mortality and morbidity worldwide [1-3]. SCI causes physical, psychological, social, and financial distress not only to patients but also to their families [4]. With an estimated global prevalence of SCI reported to be between 236 and 1,009 per million [5], SCI has a massive negative impact on national health resources: in the United States alone, the burden of SCI is estimated to cost about 2.09 billion USD per annum or approximately USD 30,770 - USD 62,553 per person per year as of 2016 [6]. Though the functional outcomes post-SCI have been predicted with some degree of success, the management of its complications is complex and wide-ranging [7,8]. With the advent of medical and technological advances in the past few decades, life expectancy after SCI has shown dramatic improvement, necessitating better management of its myriad complications in the chronic phase as the patient ages with the disease [9].
The leading causes of morbidity following SCI are potentially reversible complications such as pneumonia, obstructive uropathy, and pressure-related injuries [10]. In a recent systematic review, SCI complications were associated with the highest incremental effect in direct cost burden [11].
As most post-SCI complications can be effectively managed by primary care physicians, especially in regions where the physiatrist or board certification in SCI does not yet exist, awareness of this topic to optimally manage this group of patients is crucial. It is thus imperative that primary and tertiary care physicians act in a coordinated manner, throughout the acute rehabilitation period through the chronic post-discharge follow-up period which may be months to years’ post-injury, to minimize complications and maximize patients’ quality of life.
This narrative review aims to highlight the most common medical issues faced by all SCI patients, whether traumatic or non-traumatic, in the chronic phase in the community so that they could be recognized and dealt with early to reduce the high financial costs and psychosocial burden of this major cause of long-term disability.
The International Spinal Cord Injury Society (ISCoS) and the American Spinal Injury Association (ASIA) recommend that the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), formerly known as the ASIA Impairment Scale or AIS, be done as early after the injury as possible and then at regular intervals throughout the acute hospital stay. This enables accurate prognostication and formulation of management plans for the individual patient [12]. In addition, both ISCoS and ASIA recommend documenting autonomic functions namely bladder function, bowel output, blood pressure changes, and heart rate. A comprehensive approach to measuring multi-domain impairment is of paramount importance to provide holistic patient care [13].
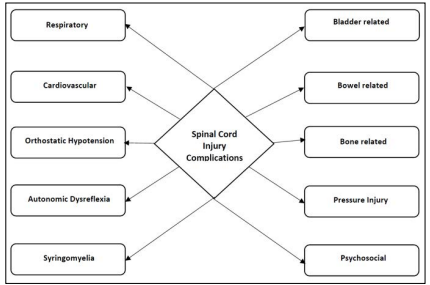
Figure 1: Summary of important complications post Spinal Cord Injury
Respiratory complications following spinal cord injury are one of the leading causes of morbidity and mortality post-SCI. Impaired mechanics of ventilation, poor cough, increased secretions and bronchospasm predispose to atelectasis, pneumonia, and exacerbations of respiratory failure [14]. Prevention of respiratory complications must start immediately and independently of the level of spinal cord injury, with red flags that may necessitate specialist referral listed in Table 1.
Table 1: Red flags for respiratory complications [15].
| Red flags for respiratory complications |
|---|
| • Shortness of breath and/or tightness in chest |
| • Decreased effort tolerance |
| • Decreased ability to clear secretions |
| • Haemoptysis, loss of appetite & weight loss |
| • Snoring with early morning headache and daytime somnolence |
| • Increased frequency of respiratory tract infections |
| • New leg swelling |
SCI is associated with 2-5 times greater prevalence of sleep disordered breathing than the general population: a group of conditions of which the most common is obstructive Sleep Apnea (oSA) [16]. obesity, increased nuchal thickness, snoring, apneic episodes, headache on waking, and daytime sleepiness are features of oSA, and when detected require referral to a specialist for further evaluation in the form of overnight oximetry or polysomnography. The appropriate treatment strategy may include positive airway pressure devices, and/or adjunctive treatments. Recommendations for the management of respiratory complications post-SCI:
• Chest Physiotherapy - along with the encouragement of deep breathing, frequent changes of position, and postural drainage of secretions
• Cough assist device to aid with coughing/expectoration of sputum
• Non-invasive ventilation, invasive ventilation and tracheostomy care
• Phrenic nerve or diaphragmatic pacing is an option for those unable to wean off ventilatory support
• Vaccinations against influenza and pneumococcus for all SCI patients
• Assessment for oSA/Sleep-disordered breathing and appropriate referrals to the Respiratory or otolaryngology specialist
With improved long-term survival, coronary artery disease (CAD) has become an important complication in the post-SCI phase [17]; hence, early identification and control of modifiable risk factors are vital. SCI patients particularly have reduced exercise capacity and cardiovascular fitness. They are at increased risk of coronary artery disease with a possible atypical presentation of acute coronary syndrome. Dyslipidemia, type 2 diabetes mellitus and changes in body composition (increased relative fat mass) influence the progression and severity of cardiovascular disease [15]. Peripheral vascular disease with delayed and complicated presentations given the lack of claudication is a concern. Bradycardia, hypotension and other drug-related cardiovascular side effects have to be carefully sought after especially by primary care physicians.
Recommendations for the management of cardiovascular complications post-SCI:
• Screening for cardiovascular risk factors early (preferably at age 45) and at regular intervals (at least yearly) • Weight management
• Smoking cessation counselling
• Consider practical exercise options like hand-crank ergometry, hand cycling, swimming, and functional electrical stimulation of muscles [18].
• Body weight-supported treadmill training has been reported to improve glucose regulation and reduce the incidence of cardiovascular morbidities
orthostatic hypotension (oH) is defined by a decrease in systolic blood pressure of >20mmHg or diastolic blood pressure of >10mmHg upon a change in body posture: usually from sitting to standing or from lying to standing. oH affects up to 74% of SCI patients, and is often associated with disabling symptoms such as light-headedness, blurred vision, and fainting, thus impeding patients’ ability and willingness to undergo rehabilitation [19]. Low sympathetic output, lack of reflex vasoconstriction, pooling of blood in the viscera and lower limbs are amongst the chief causes of oH post-SCI [20]. other contributing factors to oH include hypovolemia, hyponatremia, and cardiovascular deconditioning due to prolonged bedrest, which is corroborated by the fact that the prevalence of oH is greater in patients who sustained higher cord lesions, with tetraplegics experiencing greater reductions in blood pressure than paraplegics [21].
Recommendations for the management of orthostatic Hypotension:
• Non-pharmacological strategies:
o Adequate hydration and appropriate salt intake
o Abdominal binders
o Compressive calf stockings
o Slowed approach to change in posture
• Pharmacological strategies:
o Fludrocortisone, a mineralocorticoid induces sodium reabsorption and enhances the sensitivity of blood vessels to circulating catecholamines [22], with a starting dose of 0.1mg daily, adjusted at weekly intervals.
o Midodrine, a selective alpha-1 adrenergic agonist,can be used in the management of symptomatic oH [23]. Due to its shorter half-life of 25 min, Midodrine is usually given three times daily with a starting dose of 2.5mg, titrated to clinical response, up to a maximum of 30mg/day
o Medications such as ergotamine, ephedrine, and droxidopa have not been supported by current literature.
Autonomic dysreflexia (AD) is a potentially life-threatening complication of SCI which has a higher chance of occurring in patients whose lesions are at or above the T6 level [24]. The mechanism is thought to start with a nociceptive stimulus below the level of injury, causing excessive reflex sympathetic activity and severe vasoconstriction leading to uncontrolled blood pressure (BP). Secondary parasympathetic activity (elevated BP sensed by aortic/carotid baroreceptors) in turn produces vagal activation which does not transmit past the level of injury, resulting in bradycardia and vasodilatation above the injury level, which is often insufficient to lower BP [15]. SCI lesions lower than T6 are less likely to cause AD, because intact splanchnic innervation allows for compensatory dilatation of the splanchnic vascular bed [25].
AD, when unrecognized or not treated promptly, can cause intracranial haemorrhage, encephalopathy and seizures or cardiac arrhythmia, which can result in death. This warrants a high index of suspicion in the presence of following symptoms and signs:
• Headache
• Sudden hypertension
• Bradycardia
• Flushing/blotching of skin above spinal injury level
• Profuse sweating above spinal injury level
• Skin pallor and piloerection below spinal injury level
• Chills without fever
• Nasal congestion
• Blurred vision (dilatation of pupils)
• Shortness of breath, sense of apprehension or anxiety
AD is most commonly precipitated by urinary tract issues, followed by bowel problems. Table 2 summarizes the various common precipitants of AD that may be preventable [25].
Table 2: Common precipitants of Autonomic Dysreflexia (AD).
| Common precipitants of AD |
|---|
| • Skin-pressure area, burn, ingrown toenail, tight clothing or stockings |
| • Bladder- urinary tract infection, epididymo-orchitis, bladder distension, blocked indwelling catheter, renal tract calculus, urological procedures |
| • Bowel-constipation, rectal irritation, haemorrhoids |
| • Haemoptysis, loss of appetite & weight loss |
| • Gastrointestinal-biliary colic, appendicitis, other causes of acute abdomen |
| • Obstetric and gynaecological-onset of labour, menstrual cramping |
| • Musculoskeletal-fracture |
Recommendations for the management of suspected Autonomic Dysreflexia:
• Blood pressure control & monitoring-the use of sublingual nitrate, short acting calcium channel blockers or hydralazine can be considered
• Look for and correct any noxious inciting stimuli (eg. ingrown toenails)
• Remove tight-fitting garments
• Check for distended bladder, obstructed indwelling catheters and evaluate for urinary tract infection (UTI)
• Rectal examination looking for faecal impaction, fissures, haemorrhoids and treat appropriately-consider using numbing agents such as lignocaine in performing the rectal examination to minimize the risk of worsening AD
• Medications: Rapid-onset/short-duration agents such as Glyceryl trinitrate (GTN) and Hydralazine
Post-traumatic syringomyelia is the development of pathological cystic cavitation extending rostrally or caudally from the site of original cord injury, which occurs in about 17-20% of persons with SCI and is a common cause of worsening myelopathy. It is often heralded by pain, ascending dissociated sensory loss, increased spasticity, weakness and loss of function [15].
Recommendations for the management of syringomyelia:
• Magnetic resonance imaging (MRI) to confirm the diagnosis
• Pain management with analgesics
• Timely referral to a neurosurgeon
Spinal cord injury (SCI) disrupts bladder control: a condition often referred to as neurogenic bladder, which in turn causes other complications like urinary tract infections, vesicoureteral reflux, renal failure, and renal calculi.
Upper motor neuron dysfunction (cord injury at levels above S1- S2) involves loss of cortical inhibition of sacral reflex arcs due to disturbance of descending spinal tracts, leading to detrusor hyperactivity which occurs often in combination with detrusorsphincter dyssynergia. Whereas complete cord lesions will lead to involuntary, reflexive emptying of a hypotonic bladder, incomplete lesions cause detrusor disinhibition (hyperreflexia) resulting in urge incontinence. In detrusor-sphincter dyssynergia (DSD), the bladder reflexively contracts against the closed bladder neck, which leads to elevated bladder pressures causing vesicoureteral reflux with possible complications of hydronephrosis, recurrent pyelonephritis, and progressive deterioration in renal function [26].
Lower motor neuron bladder dysfunction is seen in conus medullaris and cauda equina injuries which results in detrusor areflexia (hypotonic bladder). Other clinical findings that accompany detrusor areflexia include saddle anesthesia, reduced anal sphincter tone, loss of voluntary sphincter control, and absence of the bulbocavernosus reflex [26].
Sustained high bladder filling pressures from poorly controlled detrusor hyperactivity and/or reduced bladder compliance may cause upper tract deterioration, hydronephrosis and renal failure.
Table 3 shows a brief approach to management of neurogenic bladder dysfunction in SCI patients [26].
Table 3: Approach to the management of neurogenic bladder dysfunction in SCI.
| Type of Bladder Dysfunction | Pathophysiology | Treatment Goals | Interventions | Method of Bladder Emptying |
|---|---|---|---|---|
| Upper Motor Neuron (UMN) Bladder | Detrusor-sphincter dyssynergia | Adequate drainage Low-pressure storage Low-pressure voiding | Anticholinergic suppression of detrusor contractions (e.g, oxybutynin, tolterodine, tricyclic antidepressants) | Intermittent catheterization Indwelling catheter (transurethral or suprapubic) |
| Detrusor hyperreflexia | Bladder evacuation with low postvoid residuals Prevention of urge incontinence | Functional electrical stimulation Suppression of bladder hyperexcitability with anticholinergics Suppression of bladder hyperexcitability with intravesical capsaicin or botulinum toxin | Activation of implanted device Timed, regular volitional voiding | |
| Lower Motor Neuron (LMN) Bladder | Detrusor areflexia (atonic bladder) | Prevention of overdistention by scheduled bladder emptying | Intermittent catheterization Indwelling catheter (transurethral of suprapubic) |
UTIs are common in SCI, with an incidence of 2.5 episodes per patient per year, but is complicated by a high mortality rate from urosepsis of up to 15%. Low-frequency, high-volume catheterization, indwelling catheters and assisted (as opposed to self) intermittent catheterization are all risk factors for UTI [27].
Colonization and asymptomatic bacteriuria occur frequently in patients with permanent catheters, particularly with low pathogenic organisms such as Pseudomonas aeruginosa or mixed-growth bacteria. Nevertheless, asymptomatic bacteriuria in patients with SCI should not be treated, even in patients employing intermittent catheterization. For symptomatic UTI in patients with SCI, the treatment should be based on urinalysis, culture, and sensitivity in a fresh urine specimen taken at a new catheter change. Available guidelines recommend 7-10 days of therapy, with no evidence of the superiority of any particular class of antimicrobials. Despite this, it is good practice to obtain urine cultures before and after the completion of the antimicrobial treatment for the identification of microorganisms and for the evaluation of antimicrobial susceptibility testing [28].
Prophylactic antibiotics should be avoided because they only serve to promote colonization with resistant organisms. Recurrent UTIs call for a review of patient hygiene and catheterization techniques and consideration of further investigation to exclude structural causes such as bladder calculi, diverticulum or catheter cystitis [29].
Recommendations for the management of urinary complications:
• Clean intermittent self-catheterization (CISC)
• Drainage by permanent indwelling urethral or suprapubic catheter
• Reflex voiding with an external collecting device
• Routine monitoring of renal function by trending urea, electrolytes, creatinine, and estimated glomerular filtration rate (eGFR) at least annually, with renal tract imaging (ie. ultrasound or intravenous pyelogram) performed every 2 years [29]
• Prompt treatment of urinary tract infections: there is no role for antimicrobials in asymptomatic pyuria and for long term prophylaxis for UTI.
• Timely referral to the appropriate specialist eg. Urologist for the management of refractory cases and those needing specialized conduits
Bowel dysfunction in SCI occurs as a result of impaired colonic transit time, altered compliance, immobility, and medication side effects (eg. anticholinergics, antidepressants, narcotic analgesics). Problems such as constipation, faecal incontinence or bowel accidents, abdominal distension and pain can significantly impact social and emotional well-being, activity participation, and quality of life.
The 2 broad types of bowel impairment post-SCI are: [30,31] A. Upper motor neuron (UMN) or hyperreflexic bowel (lesions above T12) Defecatory manoeuvres cannot be performed in these patients due to a lack of functioning abdominal musculature. There is an increased colonic wall and anal tone. Voluntary control of the external anal sphincter (EAS) is interrupted, and the sphincter remains tight, thereby retaining stool and causing constipation. Clinically there are intact anocutaneous reflexes and hypertonic EAS.
B. Lower motor neuron (LMN) or areflexic bowel (lesion affecting parasympathetic cell bodies at the conus, cauda equina or pelvic nerves) These patients lack spinal cord-mediated reflex peristalsis and slow stool propulsion leading to severe constipation. There is an increased risk of incontinence because of the denervated external anal sphincter and lack of control over the levator ani muscle. The patient often has loss of sacral reflexes including defecation and anocutaneous reflex and poor EAS tone.
The prevalence of bowel symptoms increases with time after injury, suggesting that these problems are acquired and potentially preventable. Bowel regimens should be individualized, taking into consideration the level and extent of neurological impairment, functional status, skin integrity, diet and nutritional factors, the individual’s problem-solving skills, social situation and lifestyle goals. Bowel function and a regular bowel program should be reviewed regularly as part of an annual cycle of care using a structured questionnaire. Patient-led modifications to management are likely to be necessary over time.
Recommendations for the management of bowel-related complications:
• Develop individualized regular bowel routine (daily or every other day for UMN bowel, or twice per day or daily for LMN bowel).
• High dietary fibre intake, stool softeners, colonic stimulants, contact irritants, bulk formers.
• Bowel emptying timed 30 minutes after a meal to utilize gastrocolic reflex
• Rectal emptying achieved using an enema, suppositories, anal digital stimulation and/or manual evacuation (the latter being particularly helpful in LMN-type bowel dysfunction
• Timely referral to the appropriate specialist eg. Colorectal Surgeon when conservative management is ineffective: surgical interventions like sacral nerve stimulation, colostomy, and Malone antegrade continence enema could be considered.
Non-surgical treatment methods include high dietary fibre intake, abdominal massage, digital rectal stimulation, manual evacuation, oral laxatives, transanal irrigation, rectal suppository and other pharmacological agents (stool softeners, colonic stimulants, contact irritants, bulk formers) and functional electrical and magnetic stimulation of skeletal muscles [30]. When conservative management is ineffective, surgical interventions may be considered. Surgical treatments include sacral nerve stimulation with implantation of electrical stimulation systems, colostomy, and Malone antegrade continence enema, which should only be considered when all else has failed.
Neurogenic heterotopic ossification (HO) is characterized by the formation of new extraosseous (ectopic) bone in soft tissue surrounding peripheral joints in patients with neurologic disorders. This complication may occur in up to half of SCI patients, beginning at a mean of 12 weeks after injury [31].
Only 10 to 20 percent of patients with HO have clinical symptoms, with decreased range of motion and inflammatory pain being most often reported in the affected joints. The large joints below the level of injury are typically affected: most commonly the hip. An elevated serum alkaline phosphatase level can help differentiate early heterotopic ossification from other conditions but this is not a specific finding [32]. The triple phase bone scan is the most reliable test for diagnosis.
Recommendations for the management of Heterotopic Ossification:
• Passive range-of-motion exercise to maintain joint mobility
• Early administration of nonsteroidal anti-inflammatory drugs (NSAIDs; Indomethacin 75 mg daily for three weeks or Rofecoxib 25 mg daily for four weeks) after SCI appears to reduce the incidence of HO according to a 2010 systematic review that included two randomized trials [32-34]
• Bisphosphonates may also be useful [32]
• Timely referral to the Orthopedic Surgeon or Physical Medicine & Rehabilitation specialist as surgery and/or medications is a possible treatment option to allow functional range of movement
Within days of the onset of SCI-induced immobility, there is an immediate and excessive loss of bone mass which leads to a significant decline in Bone Mineral Density (BMD) at and below the level of injury: a phenomenon known as Sublesional Osteoporosis which occurs after motor complete SCI [35]. The most feared complication is that of lower extremity fragility fractures: fractures that occur following transfers or activities that involve minimal or no trauma, which most commonly affect the distal femur or proximal tibia, and often present with no warning and may go undetected. Caregivers need to be aware as fractures often present atypically, with subtle clues such as mild redness, swelling, or slight deformity, without significant pain. Risk factors for fragility fracture after SCI include female gender, older age at injury, increased time post-injury, the use of medications such as anticonvulsants, benzodiazepines, and opioid analgesics, and most of all, history of prior fragility fracture. BMD thresholds are < 0.78g/cm2 at the femoral head, with most fractures occurring below 0.49 g/cm2 [36].
Recommendations for the management of fracture risk post-SCI:
• Calcium and vitamin D supplementation
• Baseline and regular monitoring of BMD
• Early administration of pharmacological therapy (bisphosphonates).
• Neuromuscular electric stimulation (NMES), Active-assisted Standing, and Body Weight Supported Treadmill Training
• Timely referral to the appropriate specialist in bone health eg. Endocrinologist in cases where fractures occur despite primary prevention
Prevalent in as high as 71.8% of all SCI patients, pressure injuries are defined as localized injury to the skin over bony prominences (most commonly the sacrum and ischial tuberosities) due to pressure combined with shear and friction [37]. Pressure injuries are serious, lifelong secondary complications of SCI that can lead to further disability: reduced mobility, dependence, surgical intervention, and fatal infections; increased rehospitalization risks, and mounting healthcare costs [38].
Recommendations for the management of pressure injuries [43]
• Daily skin examination to allow for early detection of ulcers
• Shifting body weight in bed and wheelchair on a regular basis
• Cleaning skin promptly after soiling
• Individually prescribed wheelchair seating system
• Maintaining adequate protein intake of 1-1.2g/kg/protein/day
• Timely referral to a specialist eg. Plastics and Reconstructive Surgery for assistance in special wound dressings or Hyperbaric Oxygen Therapy, as treatment is time-consuming and expensive, with variable efficacies, encompassing electrical stimulation, laser, ultrasonography, topical negative pressure, normothermic dressing, recombinant erythropoietin, anabolic steroids, maggot therapy, topical oxygen, and surgery [39].
Most SCI patients undergo emotional turmoil and stages of grief (denial, anger, bargaining, depression, acceptance) during the acute to the chronic phase of injury [39]. While it is of utmost importance to support them during the acute phase, it is also important not to raise false hope of recovery, but rather to make patients see that they can still have a good quality of life with SCI.
After life-changing injuries, any patient with SCI might experience relationship issues. Literature reports a high incidence of divorce and marital problems in SCI patients. Young SCI patients might face problems finding partners and/or maintaining relationships with their partners [40].
To integrate SCI patients into the community it is vital to establish their independence with appropriate assistive devices in order to make them lead an independent life. Return to work would instil confidence, preserve financial independence, and establish physical and psychological well-being for many patients with SCI [41].
Recommendations for the management of psychosocial complications post-SCI
• Establishing a good rapport with patients and organising counselling sessions to explore areas of need and address them.
• Referral to SCI support groups may be useful as the sharing of experiences in communal group sessions may be therapeutic.
• Referral to the Psychiatrist and/or Psychologist for appropriate cases for pharmacological as well as non-pharmacological management
• Motorized wheelchairs and personal mobility devices may be prescribed to help patients reintegrate into society.
• Charitable organizations and groups offering employment opportunities to patients with a disability may be introduced to patients in a timely manner.
• Inspiring stories of SCI patients participating in the Paralympics events prove that sports instil confidence and create a competitive zeal in any individual, and physically challenged patients are no exception. Any effort in including SCI patients in recreational activities and disabled sports would be invaluable.
SCI can be a highly traumatizing experience for both patients and the clinicians managing them. Awareness of the various medical complications and psychosocial issues post-SCI is crucial for the physicians managing these patients at the primary care level and concerted multidisciplinary management along with appropriate referrals to specialists will help reduce the financial costs and psychosocial burden of this major cause of long-term disability. To this end, healthcare systems around the world are transitioning to provide an integrated care pathway for SCI patients, with primary care physicians being at the hub of a multi-spoke model featuring inpatient specialist rehabilitation and community-based specialist rehabilitation[40].
