Author(s): Swapna Nadakuditi* and Shobhit Agrawal
Healthcare access is a universal right of a human yet there are disparities when it comes to the access and availability of healthcare services in urban vs rural areas. Even if there is adequate supply of services in the rural areas, the lack of physician availability limits healthcare access. A comparative study on access to care and services availability among rural and urban adults and children shows that between 2013-2015 the utilization of emergency room (ER) in urban adults is around 34% whereas it is 43.5% in rural adults reflecting on the fact that the rural adults lacked the basic preventative care access and there is an uptick in emergency visits [1]. These limitations that the rural population is facing in accessing health care are resulting in healthcare disparities. This is where Telemedicine is proving to be effective in reducing healthcare access related barriers. Telemedicine is a method of using electronic and telecommunications technology to provide care to members from a distance without the need for the member to be physically present in the provider’s location.
Non-availability of healthcare professionals in rural areas can result in lack of basic healthcare access and services. According to a research article in the urban areas there are 53.3 physicians per 100,000 people whereas the ratio of 39.8 physicians per 100,000 people in rural areas. The Designated Health Professional Shortage Areas Statistics shows that around 65.6% rural areas are designated as Primary care health professional short areas rural areas (HPSAs) as of September 2022 [1]. Pandemics like COVID and Ebola in the recent past entirely crippled the healthcare system not just in rural but also in urban areas by stretching thin the physician’s and the medical equipment availability forcing the countries to adopt to alternate options to administer patient care. In another study conducted to compare physician, dentists, and nurses’ availability in rural areas to those urban areas , the results showed that the rural areas have less per capita of primary care providers than urban areas. Figure 1 below shows the provider-to population ratio of different care providers [2]. There are also large variations in the availability of physicians among types of rural areas. Hence non availability of these health care professionals would result in likelihood of lower health outcomes and life expectancy.
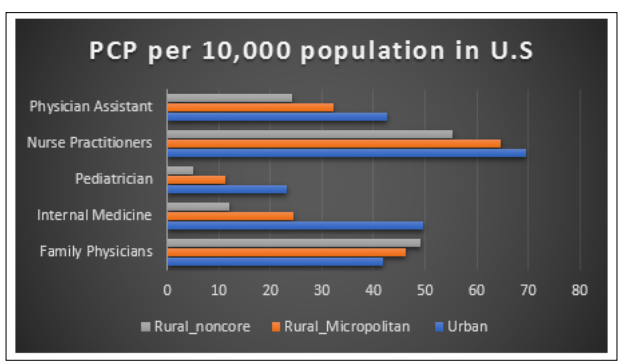
Figure 1: Number of Providers Per 10,000 Residents in United States
While the adoption of telehealth and telemedicine had been slow due to the federal policies and regulations and lack of reimbursement plan for virtual care delivery. The Centers for Medicare and Medicaid services expanded virtual care and telehealth access to Medicare advantage members in 2018 which took 2 years to go in effect in 2020 ensuring the services are reimbursed to encourage further adoption. Medicare reimburses Telehealth services based on certain parameters as defined by CMS. “Store-and-forward delivered services are prohibited, except for CMS demonstration programs in Alaska and Hawaii.” Medicare mostly covers live telemedicine. Medicaid policies for telemedicine vary from state to state; each state determines how the telemedicine services would be reimbursed. The commercial payers are most aggressively reimbursing for telehealth visits despite the regulations that affect them. There are laws that mandate commercial payers provide comparable coverage and reimbursement for telemedicine services as in-person services [3].
The article aims to discuss the barriers in the healthcare in rural areas and how telemedicine is proving to be an effective solution to improve the access to specialized care and the future of telemedicine in healthcare delivery across the globe.
Telemedicine helped break the barriers in patient care in rural areas by using remote technologies such as video conferencing, mobile applications where patients can get provider consultations, diagnostic evaluations, and medication refills from the comfort of their home or local clinics. The result is the availability of patient care in the most remote locations around the globe. Telemedicine can eliminate the need for transportation from rural areas, reduce hospital readmissions, and improve healthcare equity irrespective of the socio-economic background.
Telemedicine also made access to specialists much simpler to rural population, unlike the traditional health delivery models where the concentration of the specialists is high in Urban areas thus reducing the visits, scheduling and the wait time needed to get specialist care. The Tele Emergency Program offers rural access to 24/7 live-video consultations with emergency medical clinicians for New Hampshire, Vermont, and Maine. Kentucky Telehealth Network, with over four-hundred-member sites offers services medical, surgical, and mental/behavioral health [4]. Telemedicine can be used for remote consultations thus enhancing primary care and aid in the retaining of healthcare providers for rural areas.
In terms of managing emergency care using Telemedicine the local providers can partner with emergency care specialists to manage chronic and acute conditions remotely. For chronic disease management for conditions such as diabetes, the patients can monitor and manage the disease at home through remote patient monitoring kits reducing the risk of hospital readmissions and improving patient outcomes.
Telemedicine will be a great tool to bridge the gap in the mental health professional’s availability and in the delivery of mental health care without the need for in person visits as the mental health diagnosis and therapy is involves a conversational type of approach. According to the centers for disease control and Prevention (CDC), between 1999 and 2017 there was 33% increase of suicide rates and in the rural counties the rates were twice as high as urban areas thus giving a stark reminder of need for additional mental health professionals availability in the rural areas [5]. According to the study conducted in privately insured patients from 2005 to 2017 mental health was the primary reason for telemedicine visits with more rural states like Nevada had over forty-five visits per one hundred members for serious mental illness [6]. Telemedicine is heavily used to administer mental and behavioral health to children residing in rural communities.
Telemedicine proved to be cost effective not only for the patients in rural areas by reducing the travel to physician locations but also helped the remote communities and hospitals in reducing the cost incurred for setting up the physical infrastructure or paying exorbitant salaries to specialists by outsourcing the specialty services resulting in potential savings. A study Evaluating the Economic Impact of Telemedicine in a Rural Community concluded that among the communities evaluated for the economic impact showed around $145,000 saving annually with telemedicine adoption proving that telemedicine not only improves health care access but also boosts local economy [7].
The pandemic helped expand the telemedicine use through which most of the non- urgent patient care is being delivered virtually. The increase in adaption and the technological advancements coupled with the regulatory changes in expanding telemedicine to provide access to safe consultation with nurse practitioners, psychologists paved the way for increased access to remote patient monitoring allowing providers to check on the patients from anywhere eliminating the need for physical presence.
There is a rapid expansion of services offered via telemedicine from simple consultations to chronic disease management and specialty care such as dermatology and neurology services have been provided to patients in rural areas who otherwise would not have access to these services. Technological advancements such as wearable devices are proving to be effective to continuously monitor and share the data with healthcare providers in diseases such as diabetes from remote locations thus improving preventative care. The integration of AI and predictive analytics into the telehealth platforms are providing more accurate and early diagnosis and helping health care providers create early disease inventions.
There are efforts being made to establish global standards for telemedicine services and would increase access to the remotest part of the globe once implemented. The changes to the regulatory environment in adding additional specialties in telehealth approved services and improved reimbursements is further encouraging the telemedicine expansion. There is an increased acceptance from underserved and rural areas due to the convenience and the quality of care delivered. In United States post pandemic there is rapid increase in the use of telemedicine services as shown below in figure 2 It is forecasted that around 64M people will be using telemedicine by 2023 [8].
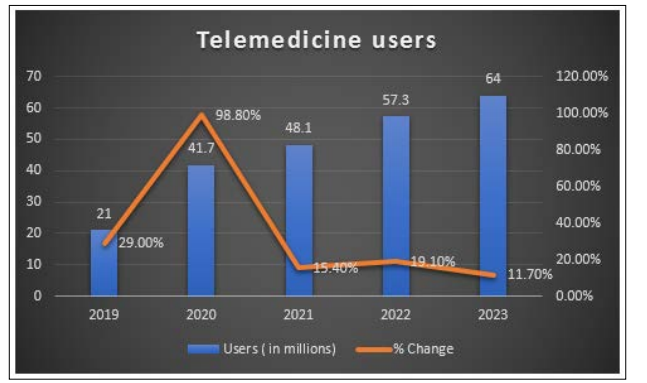
Figure 2: Telemedicine Users in United States
Integrating the telemedicine services into the traditional healthcare delivery models optimizes resource allocation without compromising patient care. Finally, improved communication across the healthcare providers due to access of patient information electronically is helping to improve Access to care and health equity.
Telemedicine in rural health settings can improve healthcare delivery by bringing access to specialized care closer to home thus promising solutions to many challenges that exist in rural healthcare delivery. The future of telemedicine depends on the faster adaptation of modern technologies and changes to policies. With the advancements in technology and the growth in healthcare innovation telemedicine can be the future way to administer healthcare delivery and this future is not just ensuring care continuity but increasing the quality of care and global reach of healthcare services.
