Author(s): <p>António Gentil Martins</p>
Purpose and Design: Having to remove an invasive Retinoblastoma one aims to avoid an unstable orbital cover after removing the periosteum and when an usual skin graft procedure might not assure the stable support of an ocular prostheses.
Methods: Based on de-doubling the lids (skin, tarsus and conjunctiva) as well as moderately freeing the peri-orbital tissues, followed by suturing together the conjunctiva of both lids.
Results: purpose and design obtained.
Conclusion: A reliable and stable orbital skin cover to support any prostheses Extraperiosteal orbital contents removal is considered essential to avoid a new recurrence when orbital exenteration is required. A new technique for orbital exenteration is described aiming to avoid one unstable free graft on the bare orbital bone that does not usually support the required postoperative aesthetic orbital prostheses.
Retinoblastoma is the most frequent ocular tumor in children and the first neoplasm to be recognized as hereditary and genetically determined in the vast majority of cases. Although nowadays early diagnosis is commun, there are still some patients that will require orbital exenteration, that is total removal of the eye, the muscles, the fat and, according to us, also, and always, the periosteum of the orbit. We present a new technique for orbital exenteration to be used in advanced cases or after recurrence of the tumor following enucleation [1-4].
The technique is demonstrated through a patient having been treated at the Pediatric Department of the Portuguese Cancer Institute Francisco Gentil (Institute’s founder).

Figure 1: Retinoblastoma
The technique is based on de-doubling the lids (skin, tarsus and conjunctiva) as well as moderately freeing the peri-orbital tissues, followed by suturing together the conjunctiva of both lids, sectioned as deep as possible in the fornices (but takingparticular care that that area is not involved by the tumor.Before trying to unfold the lids one performs a small transverse incision at the external commissure, from where the dissection of the lids will start [5-8].
The fold thus formed is invaginated into the orbital cavity in which the periosteum had been removed, and kept there by a moderately compressive dressing, at least over a week

Figure 2: External Horizontal Incision, With Removal of the Eye, Together with the Optic Nerve
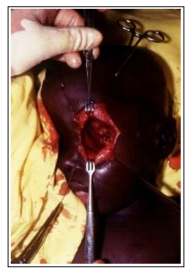
Figure 3: Orbital Cavity with the Lids Already Unfold
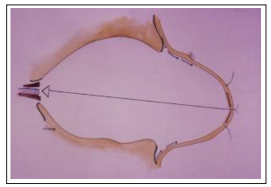
Figure 4: Schematic Drawing of the Lids Already Unfold and Sutured Together
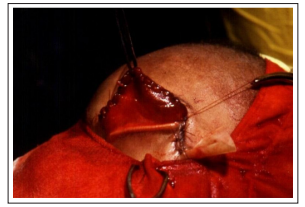
Figure 5: Lids Joined Together before being Introduced into the Orbital Cavity

Figure 6: Orbital Cavity filled with a Compressive Dressing, Pushing back the Lids
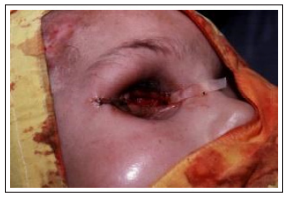
Figure 7: Immediately after after Exenteration, Showing the External Incision
The therapy of advanced Retinoblastoma involves chemotherapy,
Radiation and Surgery. Treatment of very localized lesions has
evolved markedly and also chemotherapy has improved results,
particularly with the use of Carboplatin, VP16 (Etoposide) and
VP 26 (Teniposide). As far as surgery it is certainly essential to
obtain a good segment of the optical nerve when doing a simple
enucleation.The main problem arises with more advanced lesions.
With the presented technique we can obtain two well irrigated flaps
that will be able to cover the bare surface of the orbital bones left by
the needed radical deperiostizing radical exenteration, indispensable
to avoid the recurrences which rather frequently follows surgery
that does not include periosteal removal.This way one avoids the
more complex and lengthy use of skin tubes or neighboring skin
flaps (more disfiguring), or the simple use of free grafts in bare
bone, (without the periosteum), usually obtained from the thigh, but
that generally result in a very unstable scar, unable to support the
required silicone aesthetic prostheses, which in an artist specialist
hands, result in an acceptable social appearance.

Figure 8: Orbital Cavity a few months after Surgery, with a Reliable and Stable Support for a Future Aesthetic Prostheses
Operation should take one or two hours and we believe it is wise to leave an eventual plastic surgical flap’s reconstruction for a later stage. As the orbit lies alongside with the air sinuses it is advisable to avoid blowing the nose in the immediate surgical period and it also may be better to try and sleep with the head slightly elevated, in order to try to more quickly eliminate any post-operative swelling.
Eventual (although extremely unlikely) recurrence, always possible in those patients with very severe and extensive lesions, can be easily detected, as it would also happen with the free grafts. The use of other more elaborate reconstructive procedures, eventually involving skin tubes and flaps should always be reserved for a later stage, after the possibility of recurrence is extremely unlikely. Till then, a good aesthetic prostheses is certainly the best option.
In some cases the prostheses can be the best aesthetic solution, with the drawback of the eventuality of recurrence if the periosteum is not removed.
In any case this same approach can be used after simple enucleation, although then we would prefer the early use of a prosthesis and a better aesthetic result [9-12].
In general, literature is sparse concerning surgical techniques for advanced lesions.This new surgical technique is efficient, relatively quick to perform and with a good final result, lining the orbit with well irrigated tissues, capable, in the short term, to stand the pressure of a prostheses, and does not make more difficult the detection of an eventual recurrence. It will not be required to be stressed that in performing this operation, the basic principles of surgical oncology, namely the one of incisions in totally normal tissues must be respected [13-16].
Disclaimer: The paper is a single author piece and presents no conflict of interests.
