Author(s): Varsha Ajit Sangle*, Dipali Gundre and Pragya Bhatnagar
Regional odontodysplasia (RO) is an unusual developmental anomaly in which ectodermal and mesodermal tooth components are affected. It is a localized, nonhereditary developmental abnormality of teeth with extensive adverse effects on the formation of enamel, dentin and pulp. This article reviews a case of a 16-year-old male who reported with unerupted maxillary anterior teeth. This case was rare in that it involved maxillary dentition with unerupted maxillary anterior teeth on the right side, but on the left side central incisor was unerupted. Radiographically, the affected teeth had a ‘ghostly’ appearance, showing a marked reduction in radiodensity. Both enamel and dentin appeared to be very thin, the pulp chamber was exceedingly large, and the roots were short with wide open apices. All these characteristics were consistent with the diagnosis of regional odontodysplasia. The affected teeth were surgically removed and prosthetic rehabilitation was provided to the patient.
Regional Odontodysplasia (RO) is an unusual developmental anomaly in which ectodermal and mesodermal tooth components are affected. It is a localized, nonhereditary developmental abnormality of teeth with extensive adverse effects on the formation of enamel, dentin and pulp [1].
The condition was probably first described by Hitchin (1934) [2]. Many authors however, credit it to McCall and Wald (1947) who published this condition under the name “arrested tooth development” [3]. In 1954, the term ‘shell teeth” was introduced by Rushton, which was used to describe the radiographic findings.[4] The term “odontodysplasia” was coined by Zegarelli et al., in 1963. Since it is commonly found to be affecting a group of several adjacent teeth in a particular segment of the jaw, Pindborg added the prefix “regional” in 1970; and thus, RO became an accepted terminology [4]. The other terms which can interchangeably be used with this condition are “ghost teeth”, “odontogenesis imperfecta”, “localized arrested tooth development”, “unilateral dental malformation”, “amelogenesis imperfecta”, “non-herediteria segmentalis”, and “familial amelodentinal dysplasia” [4-7].
Clinically, RO can affect the deciduous and permanent dentition in the either maxilla, the mandible or both together [1]. Maxilla is involved twice as compared to mandible. It is usually unilateral and rarely crosses the midline. The maxillary central and lateral incisors and canines being more affected than the posterior teeth. RO exhibits no specific racial predilection. Females are more often affected than males (1.4:1) [4].
This case report is of RO involving the maxilla of right side crossing the midline with certain unique findings.
A 16-year-old boy came to the Department of Oral Pathology and Microbiology, with a chief complaint of missing or unerupted maxillary anterior teeth. A previous history of trauma to his maxillary anterior region about six years back was recorded, due to which there was avulsion of few deciduous teeth. Also, few teeth, which were fractured, were subsequently removed. The patient’s medical history was non-contributory. Both parents reported no previous history of tooth or genetic anomalies on either side of the family.
Orthopantomogram showed malformed and retarded development of the right central incisor, lateral incisor, canine and left central incisor as compared to the chronological age of the child. The malformed teeth had thin radio-opaque contours with no distinction between the enamel and dentin, and wide pulp chambers, giving a ‘ghost-like’ appearance. The crowns of the affected unerupted teeth were surrounded by radiolucent areas, probably representing enlarged dental follicles. An insignificant amount of root formation was visible radiographically [Figure 1]. C T scan picture showed unrupted teeth which were malformed with enlarged pulp and enlarged surrounding follicular space [Figure 2 A and 2 B].
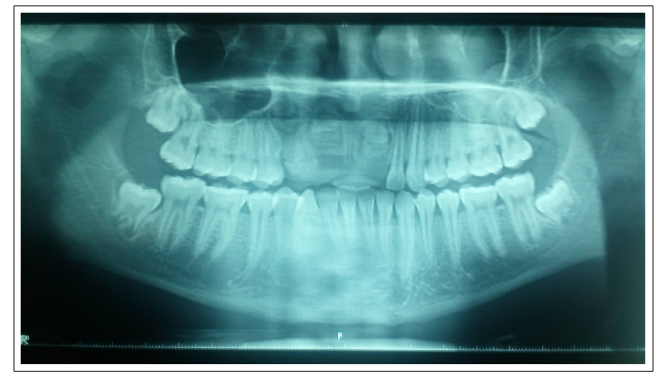
Figure 1: Orthopantomogram showed malformed and retarded development of the right central incisor, lateral incisor, canine and left central incisor
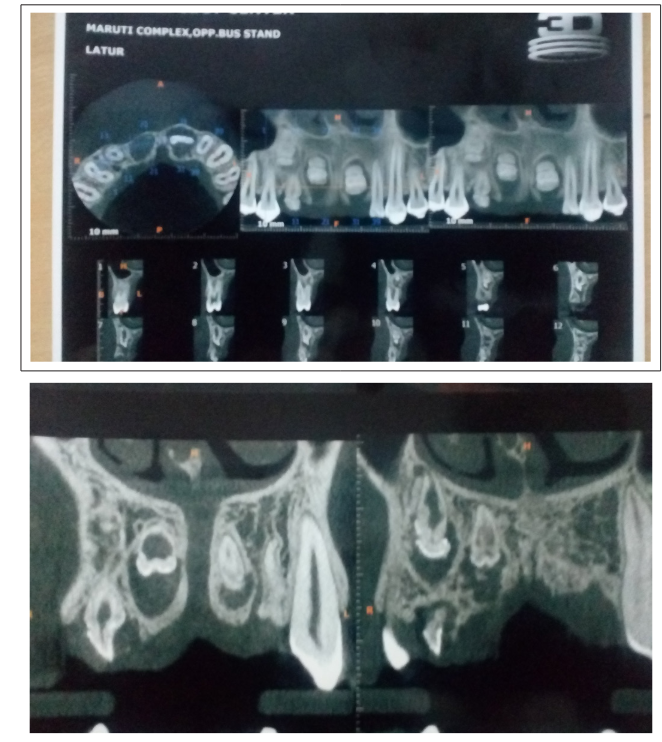
Figure 2: C T scan picture showed malformed unrupted teeth and enlarged pulp
On the basis of these clinical and the radiographical findings, a provisional diagnosis of regional odontodysplasia was made. Considering the situation, as the eruption of the affected teeth was not favorable, it was suggested to surgically remove the affected teeth. The patient’s family was properly educated about the situation. Consent was obtained for surgical removal and prosthetic rehabilitation.
Under local anesthesia, the affected teeth were surgically removed [Figure 3]. The teeth were of altered morphology, yellowish in color, soft or rubbery in consistency, and had very short roots, with wide open apices [Figure 4].

Figure 3: Picture showing surgical removal of affected teeth

Figure 4: Gross specimen of affected teeth is yellowish in color, soft or rubbery in consistency
Surgically removed teeth were histologically examined under the microscope in the ground and decalcified section. Histologically, all structures of the tooth germ were affected. [Figure 5A and 5B] In the ground section, the enamel was of variable thickness, producing an irregular surface. Longitudinal ground sections [Figure 6A and 6B] revealed the presence of enamel tissue over dentin and a central enlarged pulp cavity. The dentino-enamel junction was flat and in some areas irregular. The dentin layer was abnormally thin with the mantle dentin showing a normal dentinal tubular pattern, while the deeper dentin contained a mixture of predominant interglobular dentin and poorly organized tubular dentin.
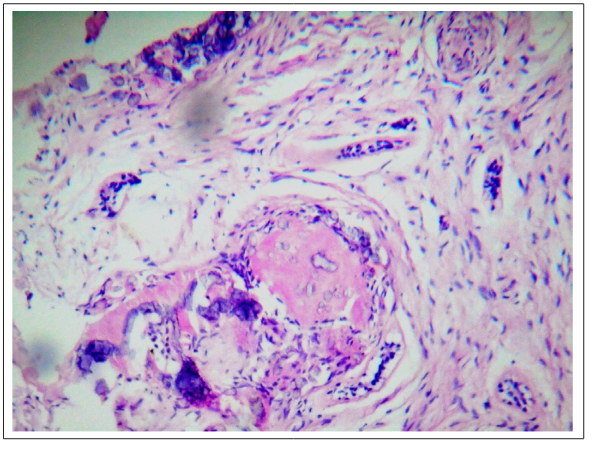
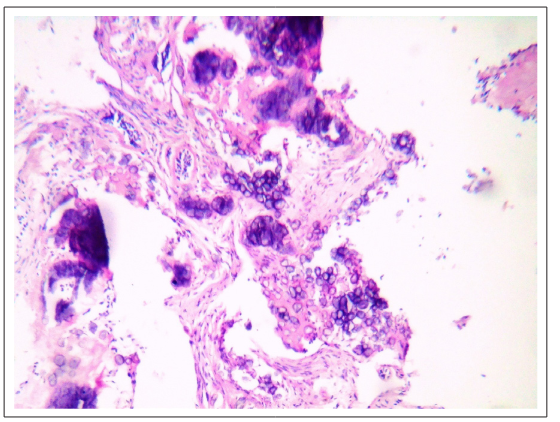
Figure 5A and 5B: H &E section showing all structures of the tooth germ were affected
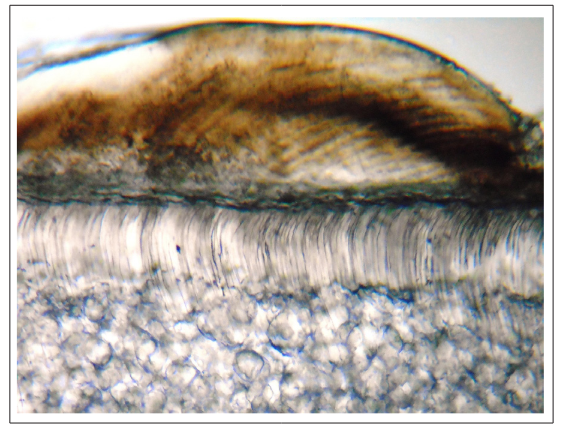
Figure 6A and 6B: Ground section showing interglobular dentin and poorly organized tubular dentin
Hematoxylin and eosin staining of the decalcified sections revealed the presence of teeth-like structures, with abnormally formed dentin and wide pulp spaces [Figure 7]. Few areas of enamel space were seen. In most of the areas the dentin was atubular and a mixture of predominant interglobular dentin. Based on the histological features, this provisional diagnosis of regional odontodysplasia was confirmed.
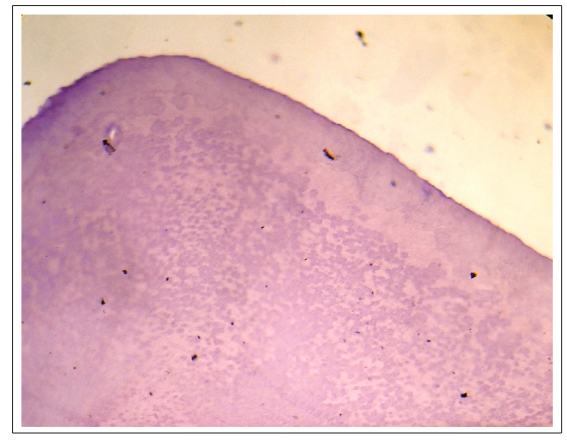
Figure 7: Decalcified sections revealed atubular dentin and a mixture of predominant interglobular dentin.
The patient will be kept under review until he reaches adulthood, when a final rehabilitation for the lost teeth might be accomplished after the facial bones have attained complete growth.
Regional Odontodysplasia is a relatively rare, nonhereditary, localized developmental anomaly of the dental hard tissues of a group of contiguous teeth [8]. Many cases are probably misdiagnosed as malformed teeth or odontomas [9]. It occurs in both deciduous and permanent dentitions, and it has a marked preference for the maxilla [8]. Other conditions, such as, dentinal dysplasia, shell teeth, hypophosphotasia, dentinogenesis imperfecta, or amelogenesis imperfecta can mimic some features of regional odontodysplasia. However, these disorders tend to affect the entire dentition, which is contradictory to RO [10].
Although many theories have been proposed for the development of regional odontodysplasia but its etiology was unknown. It has been suggested that the disturbance may derive from a disorderly proliferation of the dental epithelium at an early stage of tooth development. One theory says that an imbalance of necessary proteins might lead to the structural disorganization seen in this anomaly, such as the metalloproteinase (MMPs), which are enzymes that play a key role in dental development. Many causative factors have been suggested, for example, viral infections, vascular defects involving ischemia, local infections, trauma, Rh incompatibility, irradiation, metabolic and nutritional disturbances, vitamin deficiencies, metabolic and nutritional disturbances, vitamin deficiencies, somatic mutations affecting the dental lamina, localized trauma during pregnancy, forceps delivery, hyperpyrexia, hereditary and somatic mutation, and also neural crest migration disorders associated with hemangiomas. Some patients may also present with systemic anomalies, such as facial asymmetry and other abnormalities [8-10]. After an extensive literature review, Tervonen et al. suggested RO could be caused by vascular disturbances creating a local ischemia affecting odontogenesis. This theory is supported by the occurrence of associated hemangiomas or vascular nevi in areas adjacent to affected teeth in many of the reported cases [8].
According to the literature this condition seems to be more prevalent in females. It has a marked preference for the maxillary arch involvement over mandibular arch (2:1), which does not cross the midline [1]. However, sometimes bilateral involvement can also be seen. More commonly anterior region is affected whereas the affected teeth most often occur as a continuous series, although occasionally the anomaly will “skip” a tooth or group of teeth. Most patients came with a chief complaint of delayed eruption or gingival swelling [2,10]. The clinical presentation in this case was failure in eruption of teeth, which could be related to odontodysplasia. The affected teeth had an abnormal morphology with an irregular surface contour, with pitting and grooves, and a rough surface with defective mineralization [8]. The teeth appear to be hypoplastic, hypocalcified, and showed yellowish or brownish discoloration.
Radiographic features of RO have consistently demonstrated thin and defective layers of enamel and dentin, resulting in a faint and fuzzy outline. This reduced radiopacity with loss of distinction between hypo mineralized enamel and dentin have given rise to the term “ghost teeth.” The teeth presented with a shorter appearance and a wide-open apex with a large pulp chamber [8,10].
Histologically, all structures of the tooth germ are affected [2]. In the ground section; the enamel is of variable thickness, producing an irregular surface. The enamel prisms are irregular and show hypoplastic and hypocalcified areas, whereas, the enamel closer to the dentinoenamel junction appears more normal [8,9]. Invagination extending from the enamel surface into the dentin have been reported. The dentinoenamel junction is irregular and scalloped [4]. The dentin is thin, and the tubules are reduced in number and tortuous in shape [10]. The most significant feature is the presence of large areas of amorphous dentin containing irregularly shaped foci of a poorly formed dentinal matrix,within which, capillaries are sometimes present [1]. Interglobular dentin and globular masses interrupting the dentinal tubules are frequently seen. Cellular dentin and amorphous areas within the coronal dentin are usually evident [10]. Prominent interglobular dentin is also seen in radicular dentin [8,9].
The greater difficulty arises in treatment planning, as no consensus as to the best option has yet been reached. The main question is whether to remove the affected teeth or not, but we believe that this decision should be taken after the assessment of each individual case of regional odontodysplasia. Some authors prefer extraction and replacement with removable, and later, fixed prostheses, while others have suggested keeping the unerupted teeth, and waiting for their calcification [7,10]. From the evaluation it was decided that the eruption of the affected teeth was questionable, so it would be better to surgically remove the affected teeth and provide prosthetic rehabilitation for the patient.
The present case of RO is rare since it was seen in male patient involving maxillary anterior region crossing midline asymmetrically. The treatment of regional odontodysplasia requires a multidisciplinary approach and an organized team effort. In the present case an intermediary prosthesis was delivered. However, further treatment in the form of orthognathic surgery, bone grafting, and implant therapy needs to be anticipated in the future.
1.Cho S (2006) Conservative management of regional odontodysplasia: case report. J Can Dent Assoc 72: 735-738.
2.Crawford PJM, Aldred MJ (1989) Regional odontodysplasia: a bibliography. J Oral Pathol Med 18: 251-263
3.Rushton MA (1965) Odontodysplasia: “Ghost teeth”. Br Dent J 119: 109-113.
4.Claudhry AP, Wittich HC, Stickel FR, Holland MR (1961) Odontogenesis imperfecta. Report of a case. Oral Surg Oral Med Oral Pathol 14: 1099-1103.
5.Cahuana A, Gonzalez Y, Palma C (2005) Clinical management of regional odontodysplasia. Pediatr Dent 27: 34-39.
6.Volpato L, Botelho G, Casela L, Borges A, Silva K (2008) Regional Odontodysplasia: Report of a case in the mandible crossing the midline. J Contemp Dent Pract 3: 142-148.
7.Marques ACL, Castro WH, Vieira-do-Carmo MA (1999) Regional odontodysplasia: an unusual case with a conservative approach.Brit Dent J 186: 522-524.
8.Tervonen SA, Stratmann U, Mokrys K, Reichart PA (2004) Regional odontodysplasia: a review of the literature and report of four cases. Clin Oral Invest 8: 45-51.
9.Chinn C, Kohli K (2003) Regional odontodysplasia. A case report. NYSDJ 3: 27-29.
10.Spini TH, Sargenti-Neto S, Cardoso SV, Souza KC, de Souza SO, et al. (2007) Progressive dental development in regional odontodysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104: 40-45.
View PDF