Author(s): Atanu Mohajan*, Dipanwita Dhar*, Lailus Sabikunnahar Mishu, Vinod Warrier, Sathyanarayana Gowda and Shahid Nasim
Lemierre’s syndrome (LS) is a rare but severe complication of bacterial pharyngitis or tonsillitis, often caused by Fusobacterium necrophorum, leading to septic thrombophlebitis of the internal jugular vein and distant septic emboli. Though typically affecting young adults, we present a case of an 84-year-old man with multiple comorbidities, including dementia and coronary artery disease, who developed LS. Despite treatment with intravenous antibiotics, his condition deteriorated, resulting in gram-positive septicemia and death. This case highlights the potential for LS to affect older populations with significant comorbidities, underscoring the importance of clinical vigilance and prompt management.
Lemierre’s syndrome (LS) is a rare condition characterized by oropharyngeal infection complicated by septic thrombophlebitis of the internal jugular vein. It is primarily associated with Fusobacterium necrophorum but can be caused by other microorganisms, including Staphylococcus and Streptococcus species. LS was nearly eradicated with the introduction of antibiotics but has seen a resurgence, likely due to reduced antibiotic use for pharyngitis. This case report highlights an atypical presentation of LS in an elderly patient with multiple comorbidities, reinforcing the need for heightened awareness among clinicians.
An 84-year-old man with a medical history of dementia, hypertension, type 2 diabetes mellitus (T2DM), coronary artery disease (CAD), and previous coronary artery bypass grafting (CABG), presented to the emergency department with a three-day history of worsening shortness of breath, jaw swelling, cough, and confusion. His family noted decreased oral intake and lethargy.
On examination, the patient was tachycardic (heart rate 114 beats/ min), tachypnoeic (respiratory rate 27 breaths/min), and had an oxygen saturation of 94% on room air. His blood pressure was 107/60 mmHg, and his temperature was 36.3°C. Chest auscultation was unremarkable, but abdominal tenderness was noted.
CT Head, CT Neck and CT Pulmonary angiogram
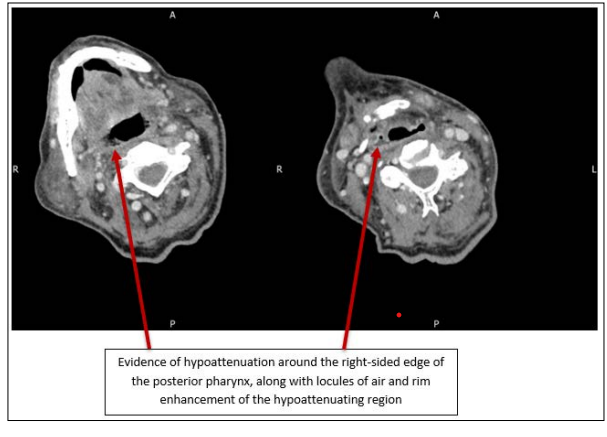
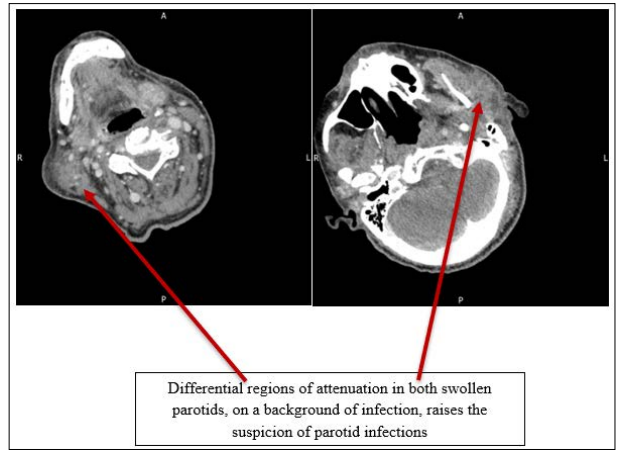
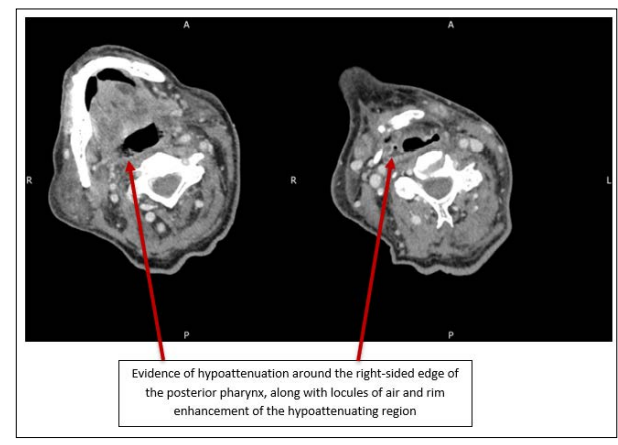
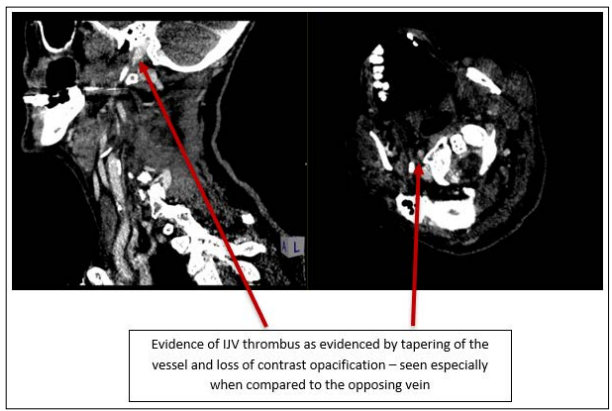

The patient was diagnosed with sepsis secondary to a pharyngeal abscess, complicated by Lemierre’s syndrome with septic thrombophlebitis of the internal jugular vein and septic pulmonary emboli.
Acute coronary syndrome (ACS) or pericarditis was considered due to elevated troponin levels but was later excluded based on the patient’s clinical course and a follow-up troponin decrease.
Initial treatment included intravenous co-amoxiclav and fluids. Following the identification of gram-positive organisms, antibiotic therapy was adjusted to intravenous flucloxacillin and vancomycin. Treatment-dose enoxaparin was started due to the internal jugular vein thrombosis. An echocardiogram showed no acute cardiac abnormalities.
Despite an initial response to antibiotics, the patient’s condition deteriorated, and he became unresponsive. Given his advanced age, multiple comorbidities, and poor prognosis, end-of-life care was discussed and agreed upon with the family. Antibiotic therapy was continued for two weeks before being discontinued. The patient experienced fluctuating consciousness and eventually died a few days later from septicemia caused by Staphylococcus aureus.
Lemierre’s syndrome is classically described as a disease of young adults, but this case demonstrates its occurrence in an elderly patient with significant comorbidities. The pathogenesis typically involves Fusobacterium necrophorum leading to septic thrombophlebitis of the internal jugular vein, though Staphylococcus aureus was the causative organism in this case.
The delayed recognition and diagnosis of LS in this patient may be attributed to its rare occurrence in older populations and non- specific presenting symptoms such as confusion and lethargy. Early diagnosis and appropriate antibiotic therapy are critical to preventing complications such as septic emboli, which were present in this case.
This case highlights the importance of maintaining a high index of suspicion for LS in patients presenting with symptoms of pharyngitis and systemic infection, regardless of age or comorbidities. Imaging studies, particularly CT, are essential for diagnosis, revealing thrombi and septic emboli that are hallmarks of the disease.
While LS is rare, its incidence appears to be increasing, possibly due to more conservative antibiotic prescribing for pharyngitis.
This case also emphasizes the challenge of managing complex infections in elderly patients with multiple comorbidities. Comprehensive management requires a multidisciplinary approach, including infectious disease specialists, radiologists, and intensivists [1-8].
This case demonstrates the severe complications of LS in elderly patients with multiple comorbidities, highlighting the need for a multidisciplinary approach to management.
Informed consent was obtained from the patient’s family for the publication of this case report
