Author(s): Laure Stella Ghoma Linguissi*, Geneviève Andoseh and Albert Mabiala
Lung cancer and pulmonary tuberculosis (TB) are two major public health problems associated with similar clinical and radiological presentations thus leading to misdiagnosis and inappropriate initiation of treatment. We investigated the case of a patient presenting symptoms for Tuberculosis and who was finally diagnosed as having probable lung cancer. Lung cancer may be the cause of some of the symptoms in TB suspected patients and this calls for vigilance on clinicians to know what appropriate tests are needed for patients presenting symptoms suspicious of TB in order to differentially diagnose TB and /or lung cancer.
Lung cancer and pulmonary tuberculosis (TB) are two major public health problems associated with significant morbidity and mortality worldwide and in low and middle income countries [1-3]. The symptoms of both diseases sometimes overlap with common features such as cough, hemoptysis, weight loss, fever, chest pain, dyspnea, loss of appetite and similar radiological images (enlarged lymph nodes, pleural effusion, opacification of air-spaces of lungs, pulmonary consolidations with irregular margins, thickwalled cavities and parenchyma infiltrate with elevated metabolic activity) are common features for both diseases [4–6]. These similarities in presentation leads to delay in the correct diagnosis and administration of appropriate therapy. Several factors are responsible for this situation in developing countries, including lack of awareness, inappropriate infrastructure, high cost of diagnosis and socio-economic factors [4,5]. Previous studies have outlined the differences between the two diseases as well as features that would make a clinician suspect the right diagnosis early [4].
TB is an important risk factor for cancer, through prolonged inflammation and pulmonary fibrosis which can induce genetic mutation and alternations, formation of scars, tissue lesions [7,8]. Tuberculosis (TB) resembles a malignant tumor and in the thorax, it may manifest as pulmonary infiltrates and / or a mediastinal lymphadenopathy. On the other hand, reactivation of latent TB in patients with cancer can occur because of immunosuppression due to malnutrition, aggressive chemotherapy, and immunomodulatory therapy
We present a case of an elderly aged male who presented symptoms for pulmonary TB but on further investigation was diagnosed to have lung cancer.
A 57-year-old man, presented to the infectious diseases department of the Makélékélé hospital with complaints of cough and expectoration for the past 1 month. There was no history of associated hemoptysis. Patient complained of chest pain and dyspnea. Patient did not complain of breathlessness, fever, weight loss or anorexia. Patient weighed 61kg and height was 152cm. Patient has primary level of education and works as a decessionary. The patient had a pulmonary symptom of rates crepitants but had no digestive, neurological and dermatological symptoms. Patient received BCG at birth and has never received a blood transfusion. Patient records no past treatment nor medical history, is a consumer of alcohol but not a smoker.
Patient was suspected to be a case of chronic respiratory disease like interstitial lung disease or pulmonary tuberculosis and least likely lung cancer.
Electrocardiogram was with in normal limits. Laboratory values showed Hb 10.3 g/dl, Hematocrit 34 %, WBC of 7.01 X10 9/ L with 69 % neutrophils, Platelet count 110 X 10 9 /L, Prothrombin time 17.2 second, total serum bilirubin 0.73 mg/dL with direct fraction 0.4 mg/dL, Serum Aspartate transminase 10.8 IU/L, Serum Alkanine transaminase 10.9 IU/L, Serum Alkaline phosphatase 256.2 IU/L, Random blood sugar 84.9 gm/dl, S. urea 46.3 mg/dl, and serum creatinine 0.93 mg/dl).
Sputum for acid fast bacilli by Ziehl Neelsen (ZN) method was negative. HIV, HBV and HCV testing for patient were all negative. Chest X ray posterioanterior (PA) view (Figure 1) revealed the presence of multiple intra parenchymal nodules of variable size looking like a released balloon in both lung fields. Mediastinal lymph nodes were absent and there was no pleural effusion. There was a normal chest-thorax index with a provisional diagnosis of lung cancer needing further confirmation. Patient was not put on Antituberculosis drugs until the confirmation could be gotten.
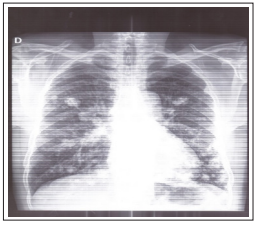
Figure 1: Chest X-ray showing the presence of multiple intraparenchymatous nodules
After thorough investigations, pulmonary tuberculosis was excluded from this patient and an incidental finding of probable lung cancer needing further confirmation was diagnosed. Patient was not put on antituberculosis drugs and he was managed with non specific antibiotics.
The association of TB and cancer in the lungs complicates diagnosis [9]. A high index of clinical suspicion and a focused diagnostic approach is essential to establish the diagnosis early [10]. However, careful history and examination can help clinician to suspect lung cancer.
In the case presented, the patient was an elderly male (57 years old). Previous studies have shown that lung cancers were more frequently found in recent survivors of tuberculosis infection. The simultaneous or sequential occurrence of TB and Lung Cancer in the same patient has been reported in various case series and case-control studies [8].
The risk is higher for men than for women and much higher for the elderly. Several studies have been published showing the association between the male gender and higher risk of lung cancer as well as TB. Young age is usually associated with pulmonary TB while the middle aged or elderly is usually associated with lung cancer. But age and lung cancer are not rare in the youth, patient’s age is no more a good reference in differential diagnosis [4]. Patient had the following commonest symptoms of lung cancer identified by Bhatt et al; chronic cough, dyspnea and chest pain (usually present and severe) [4].
Patient did not complain of breathlessness (vague and dull for lung cancer but marked and specific for pulmonary TB), fever (nonspecific for lung cancer), weight loss or anorexia, hemoptysis (a late feature in lung cancer but early for pulmonary TB) Patient weighed 61kg and height was 152cm. Patient has primary level of education and works as a decessionary. The patient had a pulmonary symptom of rates crepitants but had no digestive, neurological and dermatological symptoms. Patient received BCG at birth and has never received a blood transfusion. Patient records no past treatment nor medical history, is a consumer of alcohol but not a smoker.
Our patient was not a smoker although it is known that cigarette smoking is the important risk factor and causes almost 20% of global cancer deaths and 70% of global LC deaths [7]. Although active smoking is a major risk factor for lung cancer, passive smoking defined as the inhalation of smoke from another’s smoking and which is difficult to measure is also a risk factor [4,11]. This shows that there may be other risk factors such as air pollution, genetics and more still to be investigated that are associated with the lung cancer.
Patient tested negative for AFB smear and HIV. His samples were not cultured. In the absence of sputum culture results, we cannot exclude the possibility that the patient had pulmonary TB. Pulmonary malignancy was observed on the Chest X ray of our patient. It is commonly not visible on chest radiography early in the disease under one centimeter in diameter, and as the disease progresses, it may present as a non-specific focal consolidation with irregular borders and commonly with calcifications and usually with a solid component versus a ground glass appearance [6]. Although there are some classic findings highly suggestive of tuberculosis, it can also be quite variable sometimes revealing non-specific findings such as parenchymal consolidations in primary disease, fibrosis and scarring with parenchymal and nodal calcifications in inactive disease and more poorly defined, patchy consolidations in reactivated disease, as Parker et al. Parker et al [6]. also observed in their study, all of which could also be consistent with a lung cancer diagnosis.
Previous studies have shown that tuberculosis may increase the risk of lung cancer through substantial and prolonged pulmonary inflammation, leading to host tissue damage, fibrosis, scar formation, and genetic alterations [12].
A CT scan which is frequently the second step either to follow up on an abnormal chest X-ray finding, or to evaluate troublesome symptoms in those with a normal chest x-ray was not carried out. Lung mass is not visible on conventional X-rays unless they are larger than 5-6 mm in diameter. In the CT images, however, modern CT machines can detect lesions up to 1-2 mm in diameter, hence CT is more sensitive than chest radiography and it can accurately tell tumor site, size and invasion to adjoining structures such as mediastinum, chest wall etc. There are many features on CT scan, which suggest the diagnosis of lung cancer.
Sometimes, tuberculoma on CT scan can be misdiagnosed as lung cancer or metastasis due to its appearance resembling mass. Therefore, cytohistopathological evidence is of utmost importance to reach definite diagnosis of lung cancer. There are some limits to the case presented here. Firstly, we did confirm the diagnosis of lung cancer and pulmonary TB.
Secondly, we did not investigate other risk factors that could support the association with lung cancer such as: Exposure to certain metals (chromium, cadmium, arsenic), some organic chemicals, radiation, air pollution; Some viruses like HPV and CMV; Cytogenetic studies on oncogenes, like c-myc, L-myc, N-myc, c-raf and tumor suppressor genes, like p53 and Rb and non-small cell lung cancer genes like K-ras, N-ras, H-ras, c-myc, c-raf and tumor suppressor genes like p16 and Rb genes. These could be the focus in a new study.
Tuberculosis and cancer can be found in the lungs, as described by Vesna Cukic, 2017 [3]. In our case, we have a non-diagnosis of initially suspected pulmonary TB but suggestive diagnosis of lung cancer. Therefore, it is more likely that a patient presenting with what appears to be tuberculosis could rather have a lung cancer or both and shows the greater urgency to make an expedited diagnosis of the malignancy. This is of major concern as early diagnosis of lung cancer can increase the chance of tumor resectability, and timely chemo-radiotherapy may provide better quality of life. In patients with negative smear microscopy and suggestive radiological findings of both fields affected, it is beneficial for clinicians to further investigate for both TB (bacteria culture and PCR) and lung cancer (CT scan and cytology), in order to authenticate the final diagnosis. This incidental diagnosis of lung cancer shows the importance of making tools available diagnosis for lung cancer in patients presenting with symptoms for TB in order to arrest the cancer at an earlier stage.
The patient provided written informed consent for publication of this case report and any accompanying images.
The authors report no conflicts of interest in this work.
There were no funding sources
GLLS. was responsible for writing the manuscript. AG and MA. mainly participated in manuscript revision.
