Author(s): M Azzakhmam*, A Rahali, Mr Elochii, A Kessab, H Chahdi and M Oukabli
Introduction: The autoimmune pancreatitis (AIP) is a chronic inflammatory disease secondary to autoimmune disorders. Its s considered as a manifestation of IgG4 related disease.
Case Report: We report an exceptional case of AIP of a patient who presented with nonspecific symptoms leading to an MRI-diagnosis of a pancreatic tale tumor with strong presumption of cystadenocarcinoma rather than adenocarcinoma. Histopathological study revealed a tense lymphoplasmacytic infiltrate associated with storiform fibrosis and collagenization. Furthermore; many pseudocysts were associated lesions immunohistochemical tests revealed a diffuse staining of plasma cells by IgG and IgG4 antibodies. The diagnosis of an AIP with multiple pseudocysts mimicking a pancreatic tale tumor was made.
Conclusion: These, all criterions considered together made our case, a rare entity that may be a challenging diagnosis leading sometimes, as the current case, to a massive surgery.
Auto-immune pancreatitis (AIP) is a benign lesion first reported in 1961 [1, 2]. YOSHIDA and al proposed the concept of this entity in japan in 1995 [3]. Typically, the diagnosis can be easily assessed by imaging features when showing a diffuse pancreatic enlargement and ductal structures without dilatation. On ancillary tests, the serum IgG and IgG4 levels are often high in cases of AIP [4]. Another criterion defined by Yoshida is the absence of pancreatic cysts [3, 1]. Rare cases of AIP with pancreatic cysts have been reported, but they described also pancreatic swelling, ductal strictures and elevated IgG4 serum levels. Herein, we report an exceptional case of pseudotumoral AIP with multiple pancreatic pseudo cysts and without increase of IgG4-serum levels, misdiagnosed clinically and radiologically as a pancreatic tale tumor.
A 45 years old woman was referred to our hospital for further explorations after discovering, on abdominal ultrasonography, an inter spleen-pancreatic lesion, probably at the dispense of the pancreatic tale; it was a round well circumscribed lesion with solid and cystic components measuring 70x60mm [figure1]. The echography was undertaken because of chief complaints of abdominal pain with paroxystic vomiting, with no fever or weight loss, nor systemic symptoms. The physical examination revealed a slight deep tenderness in epigastrium with no palpable mass in soft abdomen. Lab investigations found an amylase and lipase serum levels within the normal range, the CA19-9 marker was slightly elevated.

Figure1: Abdominal ultrasonography showing a mass of the pancreatic tale in the vicinity with the spleen helium.
Thus, a complementary abdominal CT-scan been assessed to explore the abdomen; it showed a pancreatic tale mass measuring 62mm of long axis, solid and multi-cystic with contrast-enhanced cystic-walls, distant from the mesenteric vessels but in the vicinity of the spleen hilium [Figure2]. The MRI described also the same features with no lymph nodes detected and no peritoneal effusion.
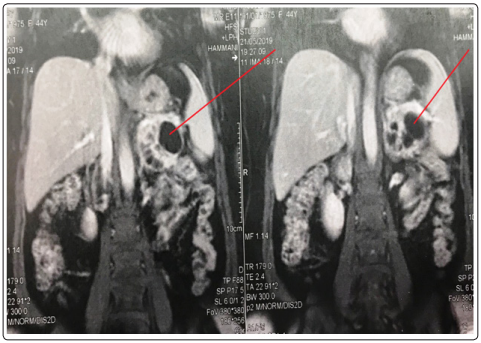
Figure 2: Abdominal CT-scan showing multi-cystic pancreatic tale mass with contrast-enhanced cystic-walls, distant from the mesenteric vessels but in the vicinity of the spleen hilium and the sigmoid colon.
Thus, the radiologists mentioned strongly the diagnosis of a cystadeno-carcinoma rather than an adenocarcinoma, and the patient underwent an extensive surgery consisting of distal pancratectomy. The specimen been achieved to our pathology lab. Grossly, the pancreatic portion was totally occupied by a well circumscribed mixed lesion with solid and cystic components. It measures 7x6x5cm and was well demarcated from the remaining pancreatic tissue, with a pancreatic margin of 0,3cm. It was also in tight contact with the spleen hilium without evident infiltration. Dissection found no lymphnodes. [Figure3]

Figure 3: gross aspects of the pancreatic lesion showing a well circumscribed mixt solid-cystic mass
Histopathological study of the tumor revealed a rich collagenous tissue with abundant infiltration of plasma cells [figure 4a]. A particular pattern of storiforme fibrosis [figure4b] and obstructive phlebitis been described. The plasma cells markers CD38/CD138 were overexpressed, with strong reactivity for IgG and IgG4.The IgG4/IgG was nearing almost 80% [4c-4d].
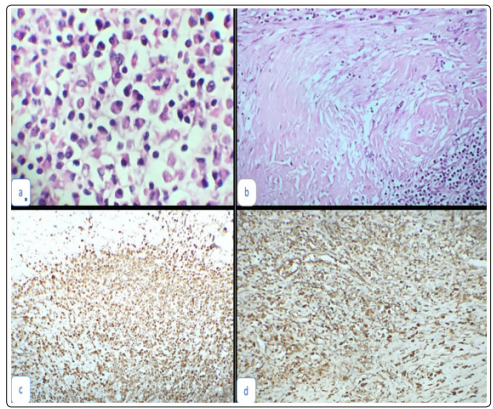
Figure 4: histological aspects of the resected lesion: a. Manufacturing power [HEx20]: rich collagenous tissue with abundant infiltration of plasma cells. b. Manufacturing power [HEx20]: particular aspect of storiform fibrosis. c. Manufacturing power [HEx20]: immunohistochemical study showing diffuse staining of plasma cells with IgG. d. Manufacturing power [HEx20]: immunohistochemical study showing diffuse staining of plasma cells with IgG4, with an IgG4/ IgG ratio near to 80%.
The cystic wall contained a few pancreatic duct epithelium associated with fibrosis and inflammation. Finally, there were no granulocytic epithelial lesions of the wall.According to all these findings, the diagnosis of lymphosclerosing pancreatitis associated with multiple pancreatic pseudo-cysts has been retained.A measurement of the IgG and IgG4 serum-levels have been achieved to complete the criterion diagnosis; they were within the normal range: respectively 12, 3 g/l (7, 00-16, 00) and 0,580g/l (0,039-0,864).
AIP first described by Sarles et al in 1961 as a primary inflammatory sclerosis of the pancreas [1, 2]. AIP is a rare disease; the estimated incidence is approximately 0,82 per 100 000 in Japan. This value is also low in western nations. The increased diagnostic modalities (radiological and serological) can explain the rise of incidence and help to differentiate AIP from malignant pathologies [1- 4]. However, AIP accounts for approximately 27% of Whipple resections done for suspicious pancreatic adenocarcinoma [5].
In a Korean study including 67 patients of AIP, 12 patients were operated due to false diagnosis of pancreatic carcinoma [6].
In the study conducted by Hammani et al, a 27 years old man presented with obstructive jaundice and radiographic image of pancreatic cancer [7]; Whipple operation was performed and histopathological examination revealed AIP. Patient respond to steroids with resolution of symptoms [7]. The most common clinical presentation of AIP is painless obstructive jaundice, which can also be confused with pancreatic cancer [5]. The most common histopathological features of AIP are irregular narrowing of the pancreatic duct, swelling of the pancreas, lymphoplasmocytic infiltration and storiforme fibrosis, and a favorable response to steroids.
Elevation of serological IgG level is a mandatory criterion by definition [1]. Furthermore, Yoshida et al, have also reported that one of the characteristic features of AIP is the absence of pancreatic cysts [3].
The non-swelling of the pancreas associated with pseudocysts is very rare, although there are two reports of 27 cases of AIP with pancreatic pseudo cysts. In the study conducted by KAMISAWA et al in 2011, IgG4 serum levels are not elevated in about 20% of AIP patients [8]. Other studies conclude that the sensitivity of serum IgG4 elevation for diagnosing AIP varies from 68% to 81% [9]. Cystic formation been reported to be 7% in some studies [10]. All these findings considered together, the present case must be rare; the serum levels of IgG4 were within the normal range, and there was only a focal tumoral-like-swelling, and the cyst formation. This case has been diagnosed only after surgery for a radiological diagnosis of pancreatic tumor.it was very difficult to achieve diagnosis before surgery and without histological study of the specimen. Finally; Awareness of the entity and use of ancillary techniques in making the pre-operative diagnosis could have saved the patient from an extensive surgical procedure.
All authors declare no conflict of interests including any actual or potential financial, personal or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, their work.
Approval to publish this paper with all related data re was obtained from the patient.
