Principles of Instrumentation in Periodontics
Author(s): Anil Melath, Jilu Jessy Abraham*, Hemalatha, Sruthy KS and Sonal Suresh
Abstract
Instrumentation in periodontics plays a crucial role in the effective management of periodontal diseases. This article explores the fundamental principles guiding instrumentation techniques used in periodontal therapy. The primary objectives include achieving optimal biofilm removal, root surface detoxification, and creating a conducive environment for tissue healing. Various instruments, such as scalers, curettes, and ultrasonic devices, are discussed in terms of their indications, advantages, and limitations. Additionally, the importance of ergonomic considerations and operator proficiency in enhancing treatment outcomes is emphasized. Understanding these principles is essential for dental practitioners to deliver comprehensive periodontal care that promotes long-term oral health and patient satisfaction.
Principles of Periodontal Instrumentation
- Accessibility: Position of Patient & Operator Visibility, Illumination & Retraction.
- Condition & Sharpness of Istruments.
- Maintaining A Clean
- Instrument stabilaization.
- Instrument Activation.
Accessibility
- Accessibility means to access accessibility facilitates thoroughness of instrumentation.
- Position of patient & operator should provide maximal accessebality.
- Inadequate accessibility impedes through instrumentation, prematurely tires the operator diminishes effectiveness of clinician.
- Clinician should be seated comfortably on an operating stool, so that clinicians’ feet are on the floor the thighs parallel to the floor.
- Be in a straight and head erect position.
- Patient should be in supine position & placed so that the mouth closed to the resting elbow of the clinician for instrumentation of maxillary arch patient chin should be rise slightly.
- For mandible arch, ask the patient to lower the chin until the mandible is parallel to floor.
Visibility, Illumination and Retraction
- Visibility: Visibility means to see.
- Illumination: Illumination means Direct vision is with direct illumination from dental light. Indirect vision is by using a mouth mirror.
- Retraction: Retraction means to Retraction provides visibility, accessibility and illumination. Mirror is also used for retraction of cheeks and tongue. Index finger is also used for retraction. When retracting, care should be taken to avoid irritation to the angle of mouth. Careful retraction is especially important for patients with the history of recurrent herpes labialis, because these patients may easily develop herpetic lesions after instrumentation.
Conditioning and Sharpness of Instrument
- Clinician should make sure that instruments are clean, sterile and in good condition.
- Working end of the pointed or bladed instrument must be sharp to be effective. Sharp instruments enhance tactile sensitivity and allow the clinician to work more
- Dull instruments may lead to incomplete calculus removal and unnecessary trauma because of excess force usually applies to compensate for their ineffectiveness.
Maintaining a Clean Field
Despite good visibility, illumination and retraction instrumentation can be hampered if the operative field is obscured by saliva blood and debris.
The pooling of saliva interferes with visibility during instrumentation & impedes control because a firm finger rest cannot be established on wet slippery tooth surface adequate suction is essential & can be achieved with saliva ejector.
Compressed air & gauze squares can be used to facilitate visual inspection of tooth surfaces just below the gingival margin during instrumentation.
Instrument Stabilisation Instrument Grasps
- Modified Pen Grasp
- Standard Pen Grasp
- Palm And Thumb Grasp
- Finger Rest
- Conventional
- Cross Arch
- Opposite Arch
- Finger On Finger
Pen Grasp: The thumb, index finger and middle finger are used to hold instrument as pen is held.
Modified Pen Grasp: The most effective & stable grasp. The pad of middle finger rest on the shank of the instrument.
Palm and Thumb Grasp: Useful for stabilizing instruments during sharpening & for manipulating air & water syringe. Not recommended for periodontal instrumentation
Finger Rest: Serves to stabilize the hand &the instrument by providing a firm fulcrum as a movement. A good finger rest prevent injury. Maximal control is achieved by using middle finger. Middle finger is kept between the instrument shank and fourth finger.
Types
Intraoral Finger Rests
- Conventional
- Cross Arch
- Opposite Arch
- Finger On Finger
Extra Oral Fulcrums
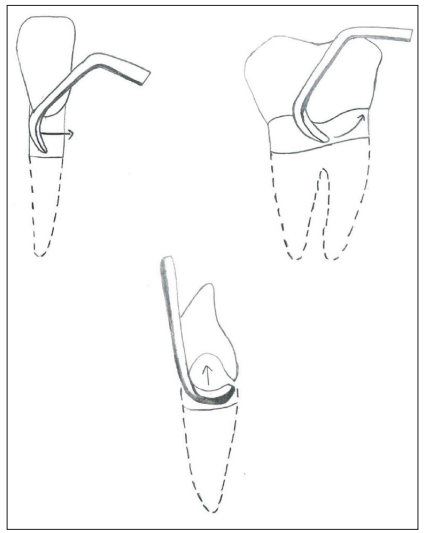
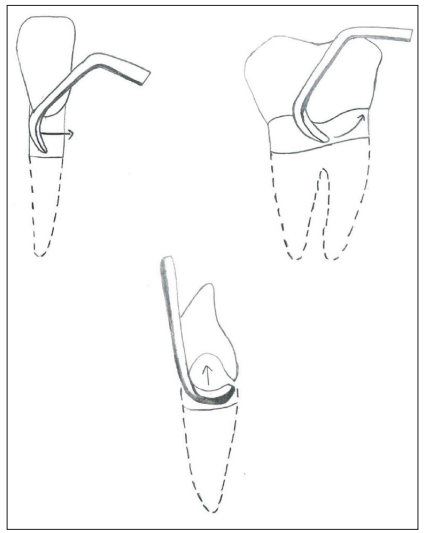
Instrument Activation Adaptation
- Adaptation refers to the manner in which the working end of periodontal instrument is placed against the surface of periodontal instrument is placed against the surface of tooth.
- Objective is to make the working end of instrument conform to the contour of the tooth surface
Angulation
It refers to the angle between face of a bladed instrument and the tooth surface also called tooth-blade relationship during insertion angle is 0o. During scaling and root planing angle is 45o - 90o.
Lateral Pressure
It refers to the pressure created when force is applied against the surface of tooth with the cutting edge of a bladed instrument. May be firm, moderate or light. Uncontrolled application of heavy forces should be avoided.
Strokes
Strokes 3 Types
- Exploratory Stroke
- Scaling Stroke
- Root Planning Stroke
Any of these strokes may be activated by a pull or push motion in vertical, oblique or horizontal direction.
- Exploratory Stroke: Light feeling stroke used with probes & explores to evaluate the dimension of pocket & to detect calculus& irregularities on tooth surface.
- Scaling Stroke: Short powerful pull stroke used with bladed instruments for the removal of both subgingival & supragingival calculus. Scaling motion should be initiated in the force arm & transmitted to the wrist to the hand with a slight flexion of fingers push scaling motion is rarely used.
- Root Planning Stroke: Moderate to light pull stroke used for final smoothening and planing of the root Hoes, files, curettes and ultrasonic instruments can be used [1-3].
Conclusion
For effective periodontal therapy and optimum patient outcomes, it is necessary to master the principles of periodontal instrumentation. Dental practitioners’ ability to thoroughly debride periodontal tissues and manage diseases will improve by understanding and applying the basic concepts such as instrument selection, adaptation, and angulation. Compliance with these principles not only enhances clinical effectiveness but also leads to improvement in patients’ general health and wellbeing. Through these approaches, it is possible for dentists to remain competent and achieve better outcomes in managing different dental conditions.
References
- Jill SG, Rebecca Sroda, Darlene S (2016) Fundamentals of Periodontal Instrumentation and Advanced Root Instrumentation, 8th Edition. Available at: https://books.co.in/books/about/Fundamentals_of_Periodontal_Instrumentat.html?id=5zZRawEACAAJ&redir_esc=y
- Dwarakanath CD (2019) Newman and Carranza’S Clinical Periodontology, Michael G Newman, Third South Asia Edition. Available at: https://www.amazon.in/Newman-Carranzas-Clinical-Periodontology-Third/dp/8131255034.
- Newman, Takei, Klokkevold (2009) Carranza ‘S Clinical Periodontology, Newman, Takei, Tenth Edition. Available at: https://www.amazon.in/Carranzas-Clinical-Periodontology-10th-Newman/dp/B0CSWS1ML2.
View PDF