Author(s): <p>E Abel Maldonado Ortiz*, Guadalupe Evelyn Pioquinto Gutierrez, Cristobal Meneces, Luis Bernardo Chavez Colunga and Elizabeth<br /> Rubio Gonzalez</p>
Extraskeletal Osteosarcoma (EOS) is a rare malignant neoplasm producing osteoid in places others than bone or periosteum [1]. The proposed etiology of EOS is metaplasia of connective tissue or embryonal remnant [2]. Previously reported cases of primary thoracic osteosarcoma did not provide a comprehensive profile of clinical manifestations and were characterized by left-sided pleural effusions, recurrent bloody effusions, cough, pleuritic chest pain and progressive dyspnea [3].
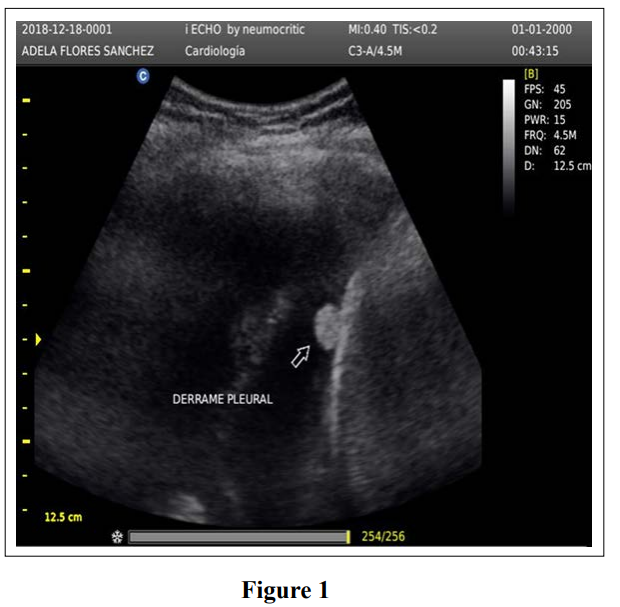
While chest radiography in combination with thoracic CT are more sensitive diagnostic tool in evaluation of pleural effusions, pleural calcifications and pleural tumors, thoracic ultrasound (LUS) has recently gained wider acceptance in the initial evaluation of pleural disease.
We herein report a case of primary extraskeletal osteosarcoma of the pleura, review the cases of pleural EOS reported in the scientific literature, and discuss the emerging role of point of care LUS in the bedside evaluation of malignant pleural disease.
A 64-year-old women presented to our cardiopulmonary and critical care clinic, complaining of 1-month of right-sided flank pain and shortness of breath. She did not have a history of smoking, environmental or occupational exposure to toxins, or comorbidities.
Her physical examination was unremarkable except for diminished breath sounds over the entire right lung and dullness to percussion in the affected side.
Lung ultrasound evaluation (Chison ECO 3, Guanzon, Chine) showed a right pleural effusion, pleural thickening, calcified nodularity, and diffuse pleural plaques.


Chest CT scan (Figure 2) showed a massive right pleural effusion, pleural nodules, an irregularly shaped large calcification on the parietal pleura, and a paratracheal calcified nodule.

Thoracocentesis and bronchoscopy were performed with cytology and cultures of the pleural effusion and bronchioalveolar lavage revealing no evidence of malignant or infection.
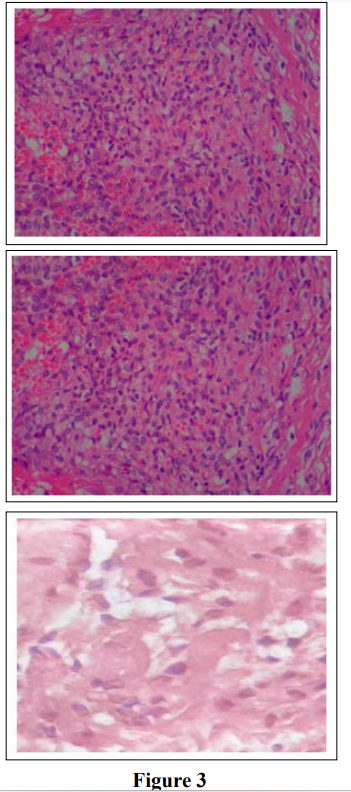
A medical pleuroscopy (Olympus BF type 2.9 Japan) was performed by the interventional pulmonary team under general anesthesia, selective left main stem intubation and non-invasive hemodynamic monitoring with bioimpedance (Cardioscreen 1000, Medis GMbH W. -v- Siemens-Str. 898693 Ilmenau Germany). Multiple pleural nodules were seen in the thickened parietal pleura (>1 cm). A large amount of pleural fluid (4 liters) was evacuated and several biopsies of the pleura were obtained. A white, hard osteoid superficial tissue were sent for histopathological analysis.
The biopsy fragments consisted of smooth muscle and osteoid producing cells, and a preliminary diagnosis of primary extraskeletal osteosarcoma was made. Immuno-histochemistry showed positive staining to vimentin, citokeratine 5/6 and negative for S-100. These pathological findings are consistent with pleural extraskeletal osteosarcoma.

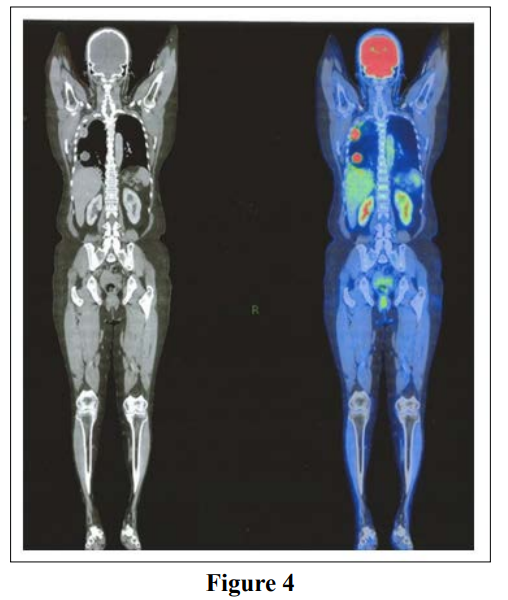
A PET CT scan found no evidence of an extra thoracic primary tumor (Figure 4). The tumor was therefore diagnosed as a primary osteosarcoma of the pleura and the patient was referred to an oncologist for treatment.
Wilson et al described the first case of mediastinal extraskeletal osteosarcoma confirmed by necropsy in 1941. (4). The most completed epidemiological record to date of these rare tumors was published in 2017 by Quian et al, including data from 60 extraskeletal osteosarcomas clinical findings were nor consistent in the series and non specific but shortness of breath, local pain, hemoptysis, weight loss, fatigue and lower limb weakness were reported. Some patients were asymptomatic (5).
Primary extraskeletal osteosarcoma arising from the pleura is extremely rare. Cohon reported the first case of primary pleural osteosarcoma in 1968. (6). Thus far,only 16 additional such tumors have been reported, including our case (7-18) Pleural calcifications can be benign and may be due to trauma (19), pleural infections, pneumothorax, calcifying fibrous pseudo-tumors of the pleura, and pleural plaques related to asbestos exposure (table 1). On the other hand, malignant causes includes pleural metastasis from osteosarcoma, chondrosarcoma, adenocarcinoma and periosteal osteosarcoma, as well as calcifications or ossifications due to pleural mesothelioma (20-21)

In some cases, the distinguishing between pleural osteosarcoma and mesothelioma may be difficult requiring special histological stains, immune-histochemistry, and ultrastructural and/or cytogenic analysis. [22,23]. In accordance with established diagnostic criteria for extraskeletal osteosarcoma, the tumor must arise in the soft tissue and not be attached to bone or periosteum, have a uniform sarcomatous pattern (to exclude the possibility of mixed malignant mesenchymal tumor), and produce osteoid and/or a cartilage matrix [24].
Confirmation of the diagnosis is important because chemotherapy for mesotheliomas has been improving in recent years, and multimodality therapy may offer some benefit in selected patients.
In comparison with others reports with documented aluminum or asbestos exposure, our patients had not known previous exposure. The etiology could be secondary to metaplasia of connective tissue or embryonal remnant.
Our case report highlights the emerging importance of point of care LUS which can be readily performed at the bedside showing pleural thickening and calcifications. The ultrasound findings were later confirmed by CT scan and the diagnostic made by medical thoracoscopy.
Pleural effusion is the most frequent findings in pleural osteosarcoma on chest radiography and/or chest CT scan is presented in 29% of reported cases [6]. Malignancy remains the most common cause of massive unilateral pleural effusion in the UK and USA, with an estimated 250.000 new cases per year. Unfortunately, cytologic analysis of pleural fluids diagnostic only in 60% of malignant pleural effusion. Tumor or ossification are considered the gold standar for the diagnosis of malignant pleural tumors including diffuse malignant pleural mesothelioma (MPM), localized fibrous tumor and pleura osteosarcoma of which MPM is by far the most common (approximately 90%). CT scan allowed better characterization of the pleural disease, differentiation of pleura thickening and pleural fluid [23]. Treatment options for primary pleural osteosarcoma are limited to surgical resection of the lesion (plaques/mass) and chemotherapy. Unfortunately, these carcinomas have poor prognosis at 5 years.
To out knowledge, point of care lung ultrasound was not the initial diagnostic test in previous reports of primary pleural osteosarcoma. In our case LUS was extremely helpful detecting a massive pleural effusion, pleural thickening secondary to diffuse plaques in the parietal pleura and echogenic nodules in minutes.
Ultrasound can be performed at bedside, is a relatively inexpensive, and harmless procedure which is increasingly performed by chest physicians.
Furthermore, the sensitivity and specificity of LUS to detect malignancy in the setting of a pleural effusion has been reported in 26/33 patients with malignant disease (sensitivity of 79% (95% CI 61 to 91%), specificity of 100% (95% CI 82% to 100%), positive predictive value (PPV) of 100% and negative predictive value (NPV of 73%) (25). Additionally, parietal pleural thickening > 1cm suggestive of malignancy is associated with sensitivity of 42% (95% CI 74% to 99%), PVP 93% and NVP 49% for differentiating malignant from benign disease. The presence of nodular thickening has a sensitivity 0f 42% (95% CI 26% to 61%), and specificity of 100% (95% CI 82 to 100%) PPV 100% and NVP 50% [25].
An additional advantage of LUS is the use of contrast enhancement or CEUS ( Ultrasound-guided needle biopsy) offers excellent diagnostic yields with a low incidence of complications [26].
In our experience, video assisted thoracoscopy was conducted by the clinical interventional pulmonologist, in comparison with surgical team in other studies. Such a clinical interventional team is a potential advantage, specially in areas where medical resources are limited.
In conclusion, primary extraskeletal osteosarcoma is a very rare carcinoma, not associated with any specific clinical symptoms or specific risk factors as demonstrated in our case. Point of care LUS proved useful in our case as the initial diagnostic study guiding further management.
Conflict of Interest: The authors have not conflict of interest.
Janice Zimmerman, MD. MACP MCCM.
Critical Care Division, Department of Medicine, Houston Methodist Hospital, Houston, TX.
Luis M. Seijo, MD.
Director de Neumología, Universidad de Navarra. Navarra, España.
