Author(s): Ana Carolina Andrade1, Bruno Camporeze, Joel Fernando Sanabria Duarte, Matheus Kahakura Franco Pedro, Bruno Augusto Telles, Daniel Almeida Benzecry and Henry Koiti Sato
Histoplasma capsulatum infection is endemic in many regions around the world, including Latin America [1]. However, cerebral presentation occurs in less than 25% of patients with disseminated histoplasmosis and even rarer as a stand-alone presentation. Three forms are described: meningeal, miliary granulomatous and parenchymal with formation of “histoplasmoma” [2]. Due to the rarity of the case and unusual clinical presentation and topography we describe the case below
A 51-year-old man, accountant, living in an urban area, was admitted to the emergency department with 30 days of bilateral decrease in visual acuity and blurred vision. Previously type 2 diabetic with good control using metformin. Denies respiratory symptoms, skin lesions, medication use to autoimmune disease, cancer, transplant organ, HIV infection, recent travels, contact with caves, bat or bird droppings. On neurological examination, he was alert and oriented, with inferior nasal quadrantopsia in his right eye. No changes in strength, reflexes and sensitivity. The first brain MRI showed:
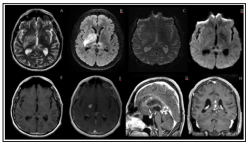
Figure 1: A- axial t2; B- axial FLAIR; C- axial DWI; D- axial SWI; E- axial T1; F-axial T1 pos-contraste; G- sagital T1 poscontraste; H- coronal t1 pos-contraste. Intra-axial lesion located in the nucleocapsular region with low signal on T2-weighted images and nodular enhancement on post-contraste images. There is also perilesional vasogenic edema with no restricted diffusion or hemorrhage / calcification on susceptibility image. There is also some other areas affecting the cerebral and cerebellar hemispheres.
First cerebrospinal fluid (CSF) analysis: 0.91/mm3 cells, 419 mg/dl protein and 30 mg/dl glucose and presence of exclusive oligoclonal bands. The second CSF analysis, with a 12-day interval between them: 270/ mm3 cells (79% mononuclear), 226 mg/dl protein and 24 mg/dl glucose. Presence of exclusive oligoclonal bands in CSF. Extensive investigation was carried out: sarcoidosis (CD4/CD8 ratio and angiotensive-converting enzyme), IgG4- related disease and anti-aquaporin 4 was negative. Normal protein electrophoresis and CSF immunotyping. Negative culture for fungi in CSF. Negative anti-histoplasma capsulatum antibodies in serum. Serologies for autoimmune and infectious diseases, including HIV and syphilis, were negative (2 measurements). The diabetics control has 7.2% glycated hemoglobina. Chest, abdomen and pelvis tomography without significant alterations. Initially opted for pulse therapy with corticosteroids for five days without significant clinical and imaging improvement. Then, he was submitted to a brain biopsy with the presence of a chronic granulomatous inflammatory process and the presence of small yeast-like fungal structures with some narrow-based budding under Grocott’s special stain. With negative BAAR research. Treatment with amphotericin B was performed for 28 days and the patient was released using itraconazole. New brain MRI, after initial treatment, shows important improvement in image appearance.
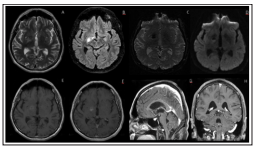
Figure 2: During the follow up, we depicted an important improvement of all lesions affecting the supra and infratentorial region, with some foci oh hemorrage on SWI related to the stereotaxic biopsy.
The actual incidence of central nervous system involvement is difficult to know. It is estimated that cerebral histoplasmosis and meningeal histoplasmosis occur in up to 7.6% of all cases and in 24% of patients with disseminated disease [3]. Isolated central nervous system histoplasmosis is even rarer, but prevalently being encountered in young, immunocompetent host [3]. It is known that imnossuppression with compromised cellular immunity is an important risk factor, as in HIV-positive patients with a history of transplantation [3]. In our case, despite extensive investigation of risk factors, the patient had only type 2 diabetes with acceptable control and no identifiable infectious source. The most common presentation of cerebral histoplasmosis is the form of chronic meningitis, isolated masses are rare and, due to their low specificity in the image, differential diagnoses with central nervous system lymphoma, tuberculoma and toxoplasmosis are mandatory [4]. The analysis of the CSF, in most patients, shows signs of chronic infection with lymphocytic pleocytosis, although neutrophilic is also common, low glucose and increased protein (some reports with more than 2 g/dl), however, presentations with isolated masses may have normal CSF [3,1]. Diagnosis is challenging, especially in immunocompetent patients, without epidemiology for the fungus and with isolated presentation of the central nervous system [2]. The gold standard for diagnosis is growth of the fungus in culture of CSF, from meningeal or brain biopsy tis sue, or from other sources such as blood or bone marrow (in those with disseminated disease) [3]. CSF yielded a positive culture in 65% of patients [3]. In patients with parenchymal disease, biopsy of the mass may be necessary. Although culture is more sensitive, Grocott-Gomori methenamine-silver staining of histologic sections may show characteristic small, round yeasts with narrow-based budding [1] (figure 2). The recommended treatment is Liposomal amphotericin B (5.0 mg/kg daily over 4-6 weeks) followed by itraconazole (200 mg 2 or 3 times daily) for at least 1 year and until resolution of CSF abnormalities [5].
