Author(s): Salman Pervaiz Butt*, Bill Cook, Yasir Saleem, Gaurav Pandey, Arun Kumar and Umer Darr
Patients undergoing coronary artery bypass graft (CABG) surgery with elevated hematocrit levels can face unique challenges related to increased blood viscosity, compromised tissue perfusion, and impaired oxygen delivery. This case report presents a 45-year-old male patient with very high hematocrit levels who underwent CABG surgery. Preoperative optimization, intraoperative monitoring, and postoperative management were implemented to mitigate the risks associated with high hematocrit. The patient’s hematocrit, blood gases, and cerebral saturation were continuously monitored during the procedure, demonstrating adequate perfusion. The patient had an uneventful postoperative course and was extubated the same day. A literature review revealed limited evidence regarding the management of high hematocrit patients undergoing cardiac surgery, emphasizing the need for further research. Tailored management strategies, including preoperative hematocrit optimization and individualized antithrombotic therapy, are crucial for optimizing outcomes in this patient population.
Patients undergoing coronary artery bypass grafting (CABG) face specific challenges when their hematocrit levels are elevated, indicating a higher proportion of red blood cells in their blood. This condition can result in increased blood viscosity, which in turn can negatively affect tissue perfusion and impede oxygen delivery. Elevated hematocrit levels in CABG patients also heighten the risk of coagulation issues, potentially leading to graft clotting during or after the procedure. The connection between hematocrit and coagulation is intricate and involves various factors. Firstly, the thickened blood resulting from high hematocrit levels can obstruct blood flow in smaller vessels, thereby increasing the likelihood of clot formation. Furthermore, elevated hematocrit can interfere with platelet function, disrupting the delicate equilibrium between clot formation and dissolution. Moreover, when combined with other factors like increased platelet count or coagulation abnormalities, heightened hematocrit levels can contribute to a hypercoagulable state.
A 45-year-old male patient presented with coronary artery disease (CAD) requiring CABG using cardiopulmonary bypass. Preoperative laboratory investigations revealed a significantly elevated hematocrit level of 61%, which exceeded the upper limit of the normal range. The patient was asymptomatic with history of being heavy smoker and diabetic.
A thorough preoperative evaluation was conducted to assess the patient’s overall health status and determine the optimal management approach. The preoperative assessment indicated no notable abnormalities except for an elevated hematocrit level. After thorough deliberation by a multidisciplinary team, it was determined cardiac surgery should proceed with the implementation of appropriate measures to mitigate the risks associated with high hematocrit. Prior to surgery, the patient underwent pre-donation post anesthesia with 600 ml of blood collected via a central line and stored in specialized blood bags containing citrate, following the guidelines provided by the blood bank. To prevent hypotension, crystalloid fluids were administered to replenish the patient’s volume deficit.
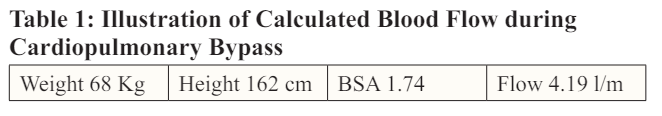
In addition, it was determined that retrograde autologous priming (RAP) and ante grade autologous priming (AAP), our usual practice for patients undergoing cardiopulmonary bypass, should be omitted. The patient was successfully placed on bypass, with diligent efforts made to enhance oxygen delivery, ensure proper fluid balance, and closely monitor critical parameters such as hematocrit levels, cerebral saturations, venous saturation, and urine output.
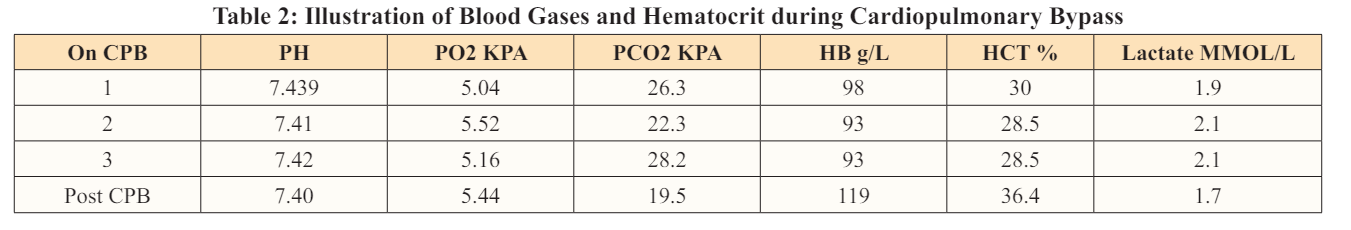
During the bypass procedure, routine blood gases were conducted, as depicted in Table 2. Continuous cerebral saturation, inline blood gases, and electrolytes were also monitored throughout the procedure. To maintain appropriate anticoagulation levels, activated clotting time (ACT) levels were consistently monitored.
The patient demonstrated a urine output of 600 ml without any indications of hemolysis. In addition to the prime plasmalyte-A 1200+100 (20%) albumin, the patient received 800 ml of crystalloid solution during the bypass procedure.
The table provides clear evidence of the patient’s adequate perfusion, as indicated by satisfactory levels of gases, hematocrit (HCT), and serum lactate. The continuous monitoring of cerebral saturation further confirms that the patient’s brain received sufficient oxygenation throughout the procedure. After discontinuing the bypass, 600 ml of the patient’s own blood was successfully transfused back. Additionally, the utilization of a cell saver during the operation enabled the recovery and subsequent transfusion of 622 ml of cell-salvaged red blood cells to the patient.
Procedure was completed uneventful and patient was transferred to the ICU where he got extubated same day without any complications.
The management of patients with very high hematocrit undergoing CABG requires careful consideration to minimize the potential risks. Numerous studies have consistently demonstrated a correlation between high hematocrit (HCT) levels and an elevated incidence of morbidity and mortality in patients undergoing cardiac surgery. Patients with elevated HCT levels are at a heightened risk of experiencing adverse events, including myocardial infarction, stroke, renal dysfunction, and prolonged mechanical ventilation. This association is likely attributable to the augmented blood viscosity resulting from high HCT, which can lead to compromised tissue perfusion [1].
Adult patients with polycythemia undergoing cardiac surgery pose unique challenges due to their increased risk of bleeding and thrombosis. The available literature on the management of these patients is very limited, but several studies shed light on potential interventions to minimize complications.
A systematic review by IK Janmohamed et al. aimed to address the management of patients with Polycythaemia Vera (PV) undergoing cardiac surgery, considering their increased risk of bleeding and thrombosis. Through a literature search and qualitative analysis, 10 case reports encompassing 11 patients were included. The findings revealed that preoperative intermittent phlebotomy was conducted in 63.6% of patients, and postoperative therapy commonly involved the use of one antiplatelet agent and one anticoagulant. Several perioperative measures were identified as important for minimizing complications, including generous fluid management, phlebotomy, preservation of core body temperature, early extubation, monitoring of myocardial ischemia, infarction, and vascular events, as well as intense chest physiotherapy and patient mobilization. The review concludes that these considerations should be systematically discussed within a multidisciplinary team, striking a balance between the acute surgical needs and the risks of hemorrhage and thrombosis associated with PV in the context of cardiac surgery [2].
Mancuso et al. conducted a study to evaluate cardiovascular risk factors on the thrombotic risk and survival outcomes in patients with polycythemia Vera (PV). The current thrombotic risk evaluation scores for myeloproliferative neoplasms, including PV, do not consider cardiovascular risk factors. The researchers collected and analyzed data from 165 consecutive PV patients, assessing the frequency of thrombotic events in subgroups categorized by the presence or absence of cardiovascular risk factors. Statistical analyses were performed using X2, Kruskal-Wallis, Kaplan-Meier, and log-rank tests. The findings revealed a strong association between the frequency of thrombotic events and cardiovascular risk, with the risk increasing as the number of risk factors increased. Additionally, survival significantly declined as the number of cardiovascular risk factors increased, regardless of traditional PV risk stratification. The study concludes that prospective studies are necessary to determine the true influence of cardiovascular risk factors on thrombotic risk and survival in PV patients, leading to the development of specific therapeutic recommendations [3].
Ruggeri et al. investigated post-surgery outcomes in patients with PV undergoing cardiac surgery. Their study revealed a higher risk of thrombotic complications in PV patients compared to essential thrombocythemia patients. The findings emphasized the importance of close monitoring and individualized management strategies for PV patients undergoing cardiac surgery [4].
The relationship between polycythemia and heart complications was explored in a review by Venegoni et al. Thrombosis of coronary arteries, heart chambers, and great vessels is a known complication of polycythemia. While exchange phlebotomy was previously the mainstay of treatment for coronary thrombosis in these patients, advances in thrombolytic agents, emergency catheterization techniques, and coronary artery bypass surgery have provided alternative options [5].
In a study by Cundy, the perioperative management of polycythemia patients was discussed. The author emphasized the need for preoperative reduction of packed cell volume in polycythemia patients and the administration of perioperative antithrombotic therapy. The study also highlighted the potential benefits of maintaining a mild state of anemia for optimal circulatory efficiency in polycythemia patients [6].
In a case, report Ilsang Han et al. describes a 67-year-old male with severe aortic stenosis and secondary polycythemia who underwent acute normovolemic hemodilution prior to aortic valve replacement surgery. The patient had a high preoperative hematocrit level due to hypoxia-induced polycythemia. Acute normovolemic hemodilution was performed after anesthetic induction to reduce the risk of thromboembolism associated with high hematocrit levels. The surgery was successful, and the patient had a post-operative period without any side effects. The findings suggest that acute normovolemic hemodilution may be beneficial in reducing hematocrit levels in patients with secondary polycythemia undergoing cardiac surgery. However, careful control of hematocrit levels is necessary to avoid potential side effects [7].
Findings from the presented case report by Grgur Dulic et al. highlight the challenges associated with performing coronary artery bypass grafting (CABG) in patients with polycythemia vera (PV). Thrombotic risk is elevated in PV patients with coronary artery disease (CAD). Despite following management algorithms and guidelines, the patient in this case experienced complex postoperative recovery, with thrombosis occurring in the native coronary vessels, including the left anterior descending artery and right coronary artery. The case emphasizes the need for further investigation into the preferred surgical approach (on-pump CABG or off-pump CABG) and optimal management strategies for patients with PV undergoing cardiac surgery [8].
A recent study evaluated the association between intra-operative autologous blood donation and the decrease in peri-operative transfusion in cardiovascular surgery based on a Japanese administrative database. The data of patients who underwent cardiovascular surgery from 2016 to 2019 were analyzed. The study found that intra-operative autologous blood donation was associated with a reduced transfusion rate and amount of blood used in both cardiac and aortic surgeries. The red blood cell transfusion rates and amounts were significantly lower in the intra-operative autologous blood donation group compared to the control group. These findings suggest that intra-operative autologous blood donation could be an effective blood transfusion strategy in cardiovascular surgery for Japanese patients, leading to potential benefits in reducing transfusion requirements [9].
Contrarily, low preoperative hematocrit levels are also associated with an increased risk of stroke following isolated coronary artery bypass grafting (CABG), as highlighted by a study conducted by Musallam KM et al. The research revealed that a 1% decrease in hematocrit concentration was correlated with a 1.07 increased odds of stroke. The risk of stroke exceeded 2% when preoperative hematocrit levels fell below 37% in men and below 38% in women. Importantly, this association held true regardless of intraoperative transfusion use. Consequently, the study underscores the importance of screening and effectively managing patients with low preoperative hematocrit levels to potentially mitigate the risk of postoperative stroke in those undergoing isolated CABG [10]
In summary, all these studies provide valuable insights into the management of adult patients with polycythemia undergoing cardiac surgery; the limited available evidence underscores the need for further research in this area. Additionally, collaboration between cardiac surgeons, anesthesiologists, hematologists, and cardiologists is crucial in managing such complex cases. A global trial would be beneficial to evaluate outcomes in this specific patient population.
The management of patients with high hematocrit undergoing coronary artery bypass graft (CABG) surgery requires meticulous attention to minimize potential risks. This case report underscores the significance of comprehensive pre, intra, and postoperative management to ensure positive outcomes in such patients. Close monitoring of hematocrit levels, blood gases, and cerebral saturation played a crucial role in maintaining adequate tissue perfusion and oxygenation throughout the surgical procedure. The patient experienced a smooth postoperative recovery and was successfully extubated on the same day. However, the available literature on the management of high hematocrit patients and its effects in cardiac surgery is limited, highlighting the need for further research in this area. Tailored management strategies, including optimizing perioperative hematocrit levels, are essential to achieve favorable outcomes in this specific patient population. Additional studies are necessary to determine the true impact of cardiovascular risk factors on thrombotic risk and survival in patients with high hematocrit undergoing cardiac surgery, which can guide the development of specific recommendations in the future.
This case report is based on a single patient’s experience and represents a limited sample size. Additionally, the specific management strategies employed in this case may not be universally applicable, and individual patient characteristics should be considered in decision-making
