Author(s): <p>Keith Chittenden</p>
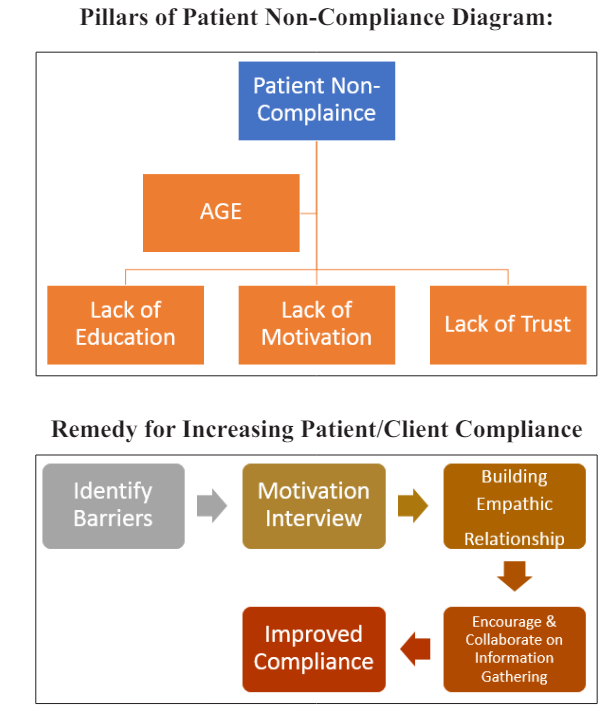
This is a research-based perspective article into patient non-compliance within the domains of medicine, physical rehabilitation, and exercise/strength and conditioning. The article identifies major pillars behind patient non-compliance: age, education, motivation, and trust as being the most influential variables that affects the amount of compliance a patient has with medical/exercise and therapeutic treatments. The article summarizes research that has identified theses variables and gives pragmatic options to help reduce the occurrence of ongoing patient non-compliance. Communication, patient compliance, motivational interviewing, virtual information gathering and barrier identity are all techniques discussed to overcome patient non-compliance. There are pragmatic tips for medical providers, therapists and trainers to assist in the management of non-compliance in their patients and clients in all aspects of practice in an evidence-based approach.
In medicine, healthcare, and sports conditioning; the goal of all practioners is the successful application of their goals to improve the health, well-being and performance of their patients and clients. Every practioner devotes many years of studying, on job training or residency into improving their skills to be the best practioner they can be. In medicine, doctors spend most of their professional lives studying pharmacological, surgical, wound care, and biomechanical approaches to solving patients’ pathological disorders with the hope of finding the best and shortest route to resolving the patient’s issue. In healthcare and sports conditioning, the therapist/trainer has devoted much of their studies on exercises and rehabilitation modalities to mitigate pain and restore maximal function after injury or enhance performance in sports. In all these scenarios, the most important person which is the center of attention is the patient. The patient is the person that receives the treatment, rehab or conditioning to improve their injury/pathology/ health/performance. In the old model of medicine; the patient is the recipient of the treatment and does not have a voice in the process of determining what the best medical course of action is for them. In the new patient-medical model of medicine and healthcare the patient is viewed as a team member or a partner in the long-term goal of continuous care receiving the maximum potential of a successful recovery or better performance. However, in many cases the patient does not follow the rules or contraindications of the desired outcomes for success. Research has demonstrated the risks for non-compliance can result in an increase in both morbidity and mortality for patients [1,2]
If a patient is ill, the doctor will prescribe the patient medication to be taken at certain intervals during the days over a specific course of time or if surgery is performed on an extremity and the doctor instructs the patient not to walk on the foot for certain duration of time. In a rehabilitation setting, a patient is given specific exercises to be done outside of therapy sessions so that progress can be achieved faster during the therapy sessions. In a non-compliance example, many patients choose not to follow the instructions of the practioner and therefore may prolong the treatment cycle. The question that most practioners have is; why doesn’t the patient follow the instructions or protocols to reach a positive outcome/recovery? This a complex question and requires analysis to what barriers the patient may be facing preventing them from following through with taking medication, following post-operative protocols or doing exercises on their own.
Patient centered care has been the most acceptable method in medicine and healthcare in the US and most European countries over the last 5-10 years. According to the patient-centered care model, treatment plans are prescribed with the patient’s goals, comprehension and well- being as the first goal11. The patient is active and usually involved in the decision on how the pathology (i.e., a common cold, the flu, or diabetic wound) is going to be treated. In some cases, oral medication, surgery or wound care dressings are chosen to be the best option, depending on the pathology and its current course. In many cases, the patient receives the wound care dressings or the prescription to the medication immediately at the doctors’ offices or clinic. It is then expected that the patient uses the dressings immediately or go to their local pharmacy to get the medication and start taking it immediately. Similarly in a rehabilitation and strength and conditioning fields, the clients are given exercises and, in most cases, are taught the exercises with physical demonstration. The client/patient will perform the exercises in the clinic or training facility and then be instructed to continue on with them outside of therapy or training.
However, this does not happen and the client/patient does not do the exercises. Why the disconnect and the lack of compliance on the part of the client/patient? According to research done in the areas of patient compliance; patient’s age, lack of education, daily behavior motivation trends and trust seems to be the major pillars behind patient non-compliance [1, 3-5].
According to Settineri, Patient compliance has many variables including age, education level, current disease comprehension, social status, patient beliefs, and cultural competence [4]. These factors have shown to be good predictors of whether or not a patient will be complaint to following medical/therapy’s orders/ protocols. Patients/clients that are used to adhering to daily behaviors such as following a diet, taking vitamins, or engaging in regular exercising have an easier time adjusting to following medical protocols such as taking medications, following wound care dressings or adhering to non-ambulatory orders versus patients that do not [1,3,4,]. Patients that are used to open and frequent communication with healthcare and medical providers also has shown to aid in compliance. Especially when the medication dose amount and schedule can be adjusted to meet the demands of the patient’s schedule. Another technique used to aid in compliance of the patient is an active role of educating the patient about their condition or pathology the patient currently has (i.e., diabetes, hypertension, fracture of ankle/foot, tendinitis etc..,) [1-4]. This is a time-consuming technique on the role of the medical and healthcare provider, however can be worthwhile if the result will help with an increase of compliance on the part of the patient. Clear communication directly to the patient is essential. The provider needs to make sure the patient is very clear on what is being communicated between patient and physician/therapist/trainer. A medical provider needs to clearly explain the pathology/condition, symptoms of the pathology, ramifications and severity of the condition if there is non-compliant, in a matter that the patient can understand. The medical/therapeutic prover should stay away from medical jargon and “buzz-words” and explain the patient’s pathology/condition and expected symptoms at an educational level that the patient can understand; this will help avoid patient confusion and a disconnect in their comprehension about their current health condition. Cultural competence is important factor the provider must take into consideration when explaining medical advice to a patient, especially if the patient is not indigenous to the country. Different cultures from global communities may interpret advice differently than a patient from the country the medical provider is practicing in. It is important the medical/therapeutic provider understand the cultural background of the patient. This will make the communication go smoother. The communication goal for the culturally competent medical provider is teaching the patient what the pathology is, what symptoms they will experience, what ramifications could happen if left untreated and how well symptoms and pain can be lessened if treated by compliance to the treatment plan [3,4,6]. A physician, therapist or trainer could use a reference such as a past patient or client that underwent the same treatment plan or exercise program and have achieved success.
According to Hall, A strategy to change patient compliance to be receptive to medical and healthcare advice is the modification of behavior motivation [2]. In some cases, when a medical practioner or a therapist is experiencing patient non-compliance, the natural course of action is to respond to the patient by repeating health advice with greater authority or to adopt a more coercive style in order to educate the patient about the imminent health risks if they don’t change [1,2,4,7]. Unfortunately, this style of motivation can have a negative effect on the patient and force them to be even more non-compliant. According to Hall, motivational interviewing can have some positive effects on the patients’ potential positive behaviors [2]. There are four principal stages in the motivational interviewing. The first is centered around empathy [2,8]. In the empathetic stage, the patient is asked to reflect on how they feel being in the care of a medical/healthcare/training professional and how they perceive the treatment or conditioning should go. The next stage in motivational interviewing is discrepancy [2,7]. In this stage the patient is asked to identify how they plan on making changes to their behavior and lifestyle so that they will be able to adapt to the constraints of following the medical/therapeutic/ exercise regimes. This will help in the planning stage when it is time to start adapting their daily lives around the medical/ therapeutical protocols [2,7]. The next stage is one of the most important stages of this interview process; identifying barriers. This stage is centered around the patient to identify the barriers that seem to be interfering with their motivation to follow medical/ therapeutic/strength conditioning advice [1,2,7,9]. This stage and the foundation built by the previous stages will help the practioner and patient break through the point where the patient will not follow the necessary medical advice/exercise prescription needed to be successful [1,2,4,8]. The last stage in motivational interviewing is the external support needed throughout self-efficacy of behavior change. This is where external people in the lives of the patient will be very important. A positive social network that surrounds the patient seems to be the long-term component the patient will need to help him/her stay on track with following proper medical and therapeutic prescriptions [1,2,4,7]. A patient’s spouse or family is one of the strongest and most reliable social supports systems a patient can have. Followed with close friends and co-workers, a patient can rely on their support system to keep them on track by simply having the support system “checking-in” with the patient on a daily or weekly basis to see if the patient has taken their medications, completed their therapeutic exercise regime or not ambulate on their post-surgical extremity (i.e., status-post foot surgery). The patient’s social support system will help enhance and strengthen the patient’s self-efficacy to being more compliant with medical/therapeutic advice [1-4]. These tools through a successful motivational interview (usually by a licensed/certified professional) may help the patient be more compliant.
According to Stewart et al., Multiple variables have an effect on compliance rates [10]. After an extensive statistical analysis, two major factors play an integral role in patient compliance; age and experience with medical providers [2,7,10]. As the patient’s age increases, compliance to medical advice seems to decline. As with many senior level patients (i.e., age 65+), compliance goes down. This phenomenon is not well explained, however using global adherence rates; a higher age will result in lower compliance in aging patients [1,2,5,8,10]. A large age gap between the patient (i.e., 65+ years old) and the medical provider (i.e., 25-40+ years old) can also increase a rift of trust of the patient to the medical provider [1,3,5,7]. This may lead to lack of trust of patients with their medical and healthcare practioners.
According to Zhang et al., Trust is an important integral characteristic that patients have which will determine the level of compliance and non-compliance [5]. In present day society, information via the internet is readily available to the public. Most health/medical related information is regularly updated. Many patients are doing their one research when they have a personal injury, pathology, or have a need for increased physical exercise training for physical improvement. Many patients will research and accumulate as much current information about their condition and will have it readily accessible when they go to see their medical/ healthcare provider. This is a strategy some patients will use to test the knowledge of their medical/healthcare provider to see if they up to speed with the treatment options, therapeutic modalities or best exercise programs that are out in the public domain [1,3,5]. If there is a disagreement between the medical provider and the patient about the appropriateness of the information the patient has gathered, this can cause altered levels of patient satisfaction or even mistrust towards the medical/healthcare provider. The medical/healthcare provider may either disagree with the literature the patient has found or have a different opinion on how treatment should proceed based on the patient’s tolerance or what intervention is more appropriate for the individual patient vs. the accepted intervention found on WebMD. This may cause a bigger rift in the trust relationship between patient and medical/healthcare provider [1,5]. This would also cause a negative effect on the patient’s willingness to comply with medical advice. Research has shown that a patient with a higher level of education and cognitive ability tends to have an easier time forming a personal relationship and can bond easier with a physician, a healthcare professional or performance trainer [2,3,6,8,11]. Zhang, showed that patients that possess higher cognitive reasoning skills that seek out health/medical related information on their own about their current medical/health status has shown a higher desire to be more collaborative with the medical/healthcare provider [5]. The patient demonstrates a higher desire to be more receptive to forming a partnership with a provider vs merely being a passive recipient for treatment. Therefore, active participation on the part of the patient towards their care yielded higher trust and compliance rates than those who did not take an interest in their current medical/ health condition. This is good news to most medical/healthcare providers, however in the fields of medicine, healthcare, and physical training; “one cannot choose your patients/clients”. The internal characteristic of trust is a very integral part of motivation [1-4]. If a patient is not motivated by positive influences both internal and external to them, then trust will be a difficult barrier to overcome.
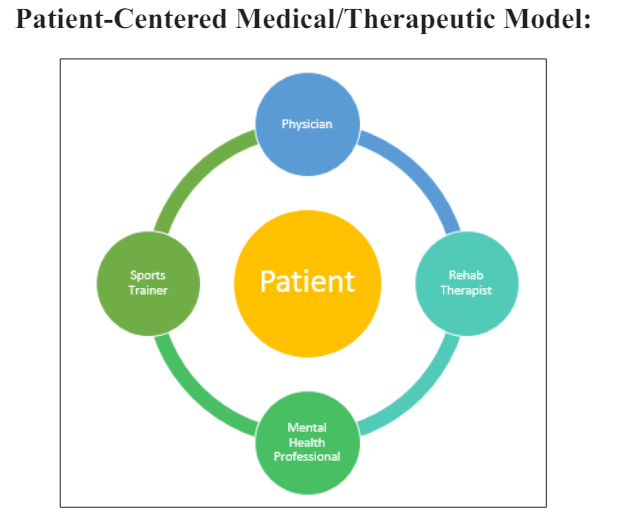
The research on patient compliance has been limited, however there are some fundamental agreements into what contributes to patient is non-compliant towards medical/healthcare/performance conditioning advice. The fundamental pillars surrounding patient compliance are centered around age, education, motivation, and trust. These universal variables may contribute to answering the question of why a patient may not be complaint to medical and healthcare providers [3,5,6,10]. With this knowledge, it is important for providers to plan their care according to their patients. In medicine, it may be difficult to form a long and solid rapport with a patient due to time constraints the physician may have with each patient they treat. With the pressures of the medical industry, a 5-10-minute visit with a physician has become the new norm in medicine. As a result, forming a solid understanding and a strong empathic bond between a patient and a physician can be challenging. Research has shown that motivation and patience towards learning about the medical condition on the part of the patient will help ease the uncertainty and fear the patient may be experiencing when seeking medical/healthcare treatment. This could help with increasing adherence towards maintaining a schedule of taking a prescription drug or following a therapeutic exercise regime at home. It may be necessary to spend an extra 5 minutes getting to know something about the patient (i.e., common interests, work history, part military service, favorite sports teams etc...,) to help solidify a strong bond between the patient and medical provider. In the field of therapy (PT, OT, SP) and strength/performance conditioning, there is more time to establish a rapport with the patient. Forming a relationship by discussing non-therapeutic subjects may put the patient at ease, so more barriers can be removed and lessen the animosity towards receiving and following medical/therapeutic treatment regimes. Research shows that when the patient/client is actively involved with treatment planning and are encouraged to seek out information on their own, compliance tends to be increased. Having the patient/client feel they are a teammate rather than a mere recipient getting treatment can help keep the patient on track. When a patient has a strong social support system, patient/client compliance can be bolstered significantly [11,12].
