Author(s): <p>Carla Echart, Florencia Dorfman, Sofía Saccone and Magdalena Otazú*</p>
Antithyroid drugs constitute one of the main pillars in the treatment of hyperthyroidism. They are associated with a variety of adverse effects, most of which are mild or minor. However, there are other rare but potentially fatal adverse effects, such as pancytopenia, of which only a few cases have been reported worldwide. This paper presents a clinical case of febrile neutropenia, associated with anemia and thrombocytopenia, secondary to treatment with methimazole.
Hyperthyroidism is characterized by an increase in the synthesis and secretion of thyroid hormones by the thyroid gland. The prevalence of this disease is approximately 1.2% [1]. The most common cause of hyperthyroidism is Graves-Basedow disease, of autoimmune etiology.
Thionamides are drugs that have been used for the treatment of hyperthyroidism for several decades. Despite their safety, they are associated with multiple adverse effects, with agranulocytosis being the most feared due to its high mortality risk. This condition occurs in 0.2-0.5% of patients, and it is mainly observed in the first 3 months after starting the drug [2]. Pancytopenia is even rarer, with an incidence of 0.01% [3]. Certain susceptibility loci have been identified to be associated with increased risk. The most common clinical signs are fever and odynophagia, though patients may also be asymptomatic [2]. Patients should be instructed to seek medical assistance promptly if these symptoms occur. Treatment requires immediate discontinuation of the antithyroid drug and the initiation of broad-spectrum antibiotics. Subsequently, definitive treatment of hyperthyroidism is required. The aim of this paper is to report a clinical case of pancytopenia caused by methimazole (MMI) and to review the literature on the adverse effects of Antithyroid Drugs (ATD).
Female patient, 51 years old, with no notable family or personal history, diagnosed with Graves' Disease in March 2023, in the context of symptoms of thyroid hyperfunction (palpitations, distal tremor, weight loss of 12 kg in 3 months) and diffuse goiter. At debut, the patient presented TSH < 0.005 uU/ml (0.27-4.2), free T4 5.6 ng/dl (0.93-1.70) and free T3 38.4 pg/ml (2-4.4). Thyroid ultrasound revealed an enlarged gland with a volume of 19 cm³, a heterogeneous echostructure with intense vascularization on colour doppler throughout the gland, and the thyroid scintigraphy shows predominantly diffuse uptake (Figure 1). She was started on MMI 30 mg/day and atenolol 50 mg/day. A complete blood count or functional liver enzymogram prior to the start of treatment is unavailable. The patient consulted in the emergency room approximately 2 months after starting MMI due to fever and odynophagia. On physical examination, tachycardia of 108 cpm, without elements of dysthyroid orbitopathy, oropharynx with multiple whitish exudates and at the thyroid gland level, diffuse grade 2 goitre was noted, no nodules or lymphadenopathy were palpable. Laboratory testing at admission revealed severe neutropenia of 10 cells/mm³, normal hemoglobin and platelets, normal kidney and liver function, sexually transmitted disease serology negative, antigen test for SARS-COV 2 negative, blood culture negative, urine culture negative, chest x-ray and electrocardiogram normal. MMI was immediately suspended and therapy was started with intravenous antibiotics, oral fluconazole, and granulocyte colony-stimulating factor (G-CSF), one subcutaneous ampoule per day. In the evolution, the patient adds anemia (hemoglobin 8.4 g/dl) and decreased platelet count (platelet 57 x10³/ul); myelogram was performed, which reported bone marrow dysplasia (Figure 2). Subsequently, clinical improvement occurred, with an increase in neutrophils to normal values, G-CSF was suspended, and radioiodine was administered at a dose of 25 mCi with a view to definitive treatment of hyperthyroidism.
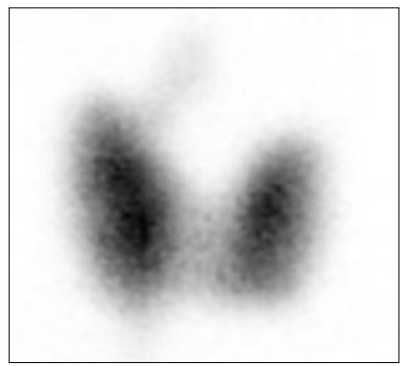
Figure 1: Thyroid Scan with Diffuse Uptake of the Gland

Figure 2: Myelogram: Methimazole-Induced Bone Marrow Dysplasia
ATD such as methimazole, carbimazole and propylthiouracil (PTU) have been widely used for the treatment of hyperthyroidism for several decades. Their main effect is to inhibit synthesis of thyroid hormone by interfering with thyroid peroxidase-mediated iodination of tyrosine residues on thyroglobulin, an important step in the synthesis of thyroxine and triiodothyronine [4]. In general, these drugs are administered for long periods with good tolerance. Mild adverse effects occur in up to 20% of patients and include skin reactions, arthralgias, and gastrointestinal symptoms [4-5]. Agranulocytosis, defined as a neutrophil count less than 500 cells/ mm³, is a rare but serious complication associated with ATD, since it endangers the patient's life [1]. Pancytopenia is another adverse effect described, though it is less common. In a study conducted by Watanabe et al involving 50,385 patients treated with ATD, only five cases of pancytopenia were identified; which corresponds to an incidence of 0.01% [3]. In four cases in this study, pancytopenia was preceded by agranulocytosis, as in this report. Such effects generally occur within the first 3 months of treatment, but this complication can arise even a year or more after starting therapy [6]. Notably agranulocytosis can develop after a previous course of treatment without complications.
In the study carried out by Nakamura with 754 cases with agranulocytosis, over 70% of the patients developed these adverse effects within 60 days, and nearly 85% within 90 days (6). In addition, they demonstrated that neutropenia can appear suddenly, among 211 patients with blood counts prior to neutropenia, more than half showed normal granulocyte counts in the 2 weeks prior to onset, one patient even had a normal count just one day before the onset of neutropenia [6].
Several reports suggest that MMI-induced side effects are dose- related, while those of propylthiouracil are less dose-related [4,7]. It has been suggested that high doses of MMI are associated with the development of agranulocytosis [8]. In a study conducted by Cooper et al. It was observed that patients receiving MMI 40 mg/ day have 8.6 times greater risk of agranulocytosis compared to lower doses [9]. In a retrospective study, a higher frequency of agranulocytosis was found in cases receiving MMI 30 mg/day, compared to those receiving 15 mg/day [10].
The pathogenic mechanism by which ATD induce agranulocytosis is not well established but appears to be immune-mediated. Cytoplasmic antibodies have been identified that target antigens on the surface of neutrophils. On the other hand, oxidative metabolites of drugs induce T cell-mediated reactions against the proliferation and differentiation of pluripotent hematopoietic stem cells in the bone marrow [4,11]. Several pharmacogenomics studies have identified that patients carrying the HLA-B*27:05, HLA-B*38:02 and HLA-DRB1*08:03 alleles could present a higher prevalence of agranulocytosis due to ATD [11]. Early diagnosis is essential to prevent the progression of infection and associated mortality. Female sex and age over 40 years have been found to be favorable factors [6]. Among the clinical manifestations, oropharyngeal infections are the most frequent, presenting with fever and odynophagia as in this case [2,4]. Treatment in these cases primarily consists suspension of the ATD and beginning with the administration of broad-spectrum antibiotics, after taking corresponding culture samples for study. Some studies indicate that granulocyte colony stimulation factors reduce recovery time, duration of antibiotic therapy and hospitalization [2,12]. However, these results should be considered with caution since other studies suggest that the treatment is ineffective in cases of severe neutropenia [13]. ATD-induced neutropenia is rare, so systematic control blood counts are not recommended [2]. Regarding hyperthyroidism, the use of another ATD is contraindicated, given that there is cross-reactivity between MMI and PTU, so definitive therapy with surgery or radioiodine is considered.
MMZ is a drug frequently used in the treatment of hyperthyroidism, and its use is associated with different adverse effects, some of which pose a high risk for the patient. Neutropenia or pancytopenia induced by ATD carries a high morbidity and mortality, making it crucial to have updated knowledge on the subject. This should be taken into account in patients receiving this treatment, since it is mandatory to perform a blood count before starting ATD. Patients should be educated about these side effects and instructed to promptly discontinue the medication and seek medical attention in the event of fever and odynophagia. Early recognition of these adverse effects will allow timely action, where suspension of ATD is the first therapeutic measure.
