Author(s): Pornsri Niransuk, Yada Tingthanatikul and Chonthicha Satirapod*
OHVIRA syndrome is a rare condition usually present during early puberty, after menarche. The main symptoms are caused by the obstruction of hemivagina and accumulation of blood, which cause the symptoms such as dysmenorrhea, chronic pelvic pain or pelvic mass. Transvaginal septectomy is the best way to treat of patient’s obstructive hemivagina. However, in young patients, the small vagina canal is a significant limitation, and it is challenging to explore the surgical field. Due to the uncommon condition at young ages and variation in coexisting anomalies, approach techniques and instruments are still under development. In this case series, we present 2 cases of OHVIRA syndrome who received surgical treatment at Ramathibodi Hospital, Mahidol University. Both cases used the same innovative vaginal retractor, designed and modified for the young patient with OHVIRA syndrome. After the procedure, patients showed no complications or recurrence up to 2 years of follow-up.
Female genital tract anomalies are one of the rare conditions that can result in various abnormal symptoms, including pelvic pain or mass, dysmenorrhea, and recurrent pregnancy loss, possibility leading to surgery. One of the rare conditions of Mullerian duct anomaly is Obstructive hemivagina ipsilateral renal ovary, also known as OHVIRA syndrome or Herlyn-Werner-Wunderlich syndrome (HWWS). The OHVIRA syndromes comprises three significant abnormalities: uterine didelphys, obstructive hemivagina and ipsilateral renal anomaly. Accordingly, this abnormality accounts for 5% of the total Mullerian dysgenesis which prevalence varies from 0.4-6.7% [1]. OHVIRA syndrome was first reported in 1922, by Purslow C., et al [2]. The patients will present the symptoms when they start menstruation or a short period after that, a so-called post-pubertal disease. There are various anomalies even though the presenting symptoms are in the same pattern. Interestingly, uncommon cases can present with the symptoms shortly after birth (within the first 6 months after delivery) due to withdrawal of maternal estrogen hormone and causing vaginal bleeding [3, 4]. The rare variants of the classical syndrome were average of 27.6% such as uterus septum, ectopic ureter [5].
Treatment for this condition aims to release the obstruction of the hemivagina and prevent its recurrence. The correlating anomalies that could complicate the situation, such as hemotosalpinx and endometrioma, must be explored for purpose and treatment plans. Surgery is the standard option of treatment which is traditional transvaginal septum resection. The septectomy technique depends on physician-patient preference and available instruments. Nowadays, the vaginoscopic resection of the septum was also introduced as an option for correcting the hemivaginal septum. In Ramathibodi hospital, we use combined techniques to approach the operating treatment for OHVIRA syndrome. Then we are going to present the two-case series of OHVIRA syndrome that were treated at Ramathibodi Hospital. Our team developed an innovative instrument to improve the surgical field for a better outcome and prevent recurrent septum or adhesion in the vagina.
Our data was a retrospective study based on a patient’s medical records with OHVIRA syndrome between 2020 to 2022 at Ramathibodi Hospital, Mahidol University. Two cases of OHVIRA syndrome were diagnosed with MRI. We reviewed from the time of diagnosis to the most recent follow-up examination. Here we showed the clinical presentation (signs and symptoms), physical examination, radiologic imaging, operative reports, pathological report, follow-up session, and complications. The study was approved by the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University (Approval No. MURA2022/210).
Case 1: A Thai girl, nine years and nine months old was consulted by the emergency department due to urinary retention with a pelvic mass. Her underlying condition is attention deficit hyperactivity disorder (ADHD), obesity, central precocious puberty, and constipation. Then she follows up with the pediatrician. She was menarche at eight years and six months old and had regular menstruation. Two months earlier, she had pelvic pain after menstruation that radiated to the buttocks but no dysmenorrhea. Her pelvic pain was progressive. Moreover, she developed urinary frequency and urinary retention problems. She had no history of sexual activity. At the emergency room, a physical examination revealed a pelvic mass of 18 wk sized with cystic consistency. Transabdominal ultrasound showed a cystic mass of 8.14x14.1 cm, hypoechoic content, a normal left kidney, and an unidentified right kidney. Magnetic resonance imaging (MRI) findings showed right hydrometrocolpos and right renal agenesis, compatible with OHVIRA syndrome, as shown in Figure 1A and 1B. Then she was admitted to the gynecologic ward and set up for operative treatment, vaginoscope, and transvaginal septectomy. Firstly, a vaginoscopy was performed. This step showed hematocolpos at the right side of the vagina, and the left cervix was identified. Next step, the vagina was explored by using our innovative vaginal retractor. Then, a surgical marker was used to mark the outline for resection to avoid injury to the urethra and another cervix. After that, the vaginal septum was incised carefully, more accessible due to good exposure by the new instrument, following the previously drawn outline. Then, brownish content of about 700 milliliters (ml) was released. Finally, the surgical edge was sutured with synthetic absorbable sutures using a continuous locking technique with an assisted vaginoscope. Follow-up in the next year, clinically and transabdominal ultrasound, showed no dysmenorrhea, recurrent hematocolpos, or pelvic masses.
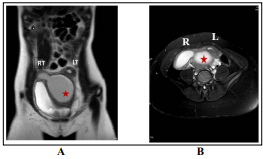
Figure 1: Case 1 Magnetic resonance imaging images. A-Coronal view, B-Axial view, RT showed right horn of uterus, LT showed left horn of uterus, Red star showed hematocolpos
Case 2: A Thai girl, eleven and two months old, began menstruating at nine years old. She presented with right lower quadrant pain with a fever. The diagnosis was urinary tract infection, an antibiotic was given, and her clinical improved. Transabdominal ultrasound showed an absent right kidney and bilateral hydronephrosis. Therefore, she was referred to Ramathibodi Hospital for suspected ureteropelvic junction (UPJ) obstruction. We repeated ultrasound and MRI, which showed an absent right kidney, a normal left kidney, and uterine didelphis with a right hematometrocolpos suspected of having OHVIRA syndrome. There was a right hematosalpinx size of 2.5 cm in diameter, as shown in Figure 2A and 2B. Therefore, she was admitted and planned for definite treatment, vaginoscopy, and vaginal septectomy. Intraoperatively, a bulging cystic mass measuring 5 cm was located on the right side of the vagina wall. In addition, a surgical marker was used to mark the outline, and the vaginal septum was incised following the outline. The brownish content was drained, about 300 ml. Septectomy was done with resected tissue measuring 5 x 2 x 0.5 centimeter (cm), as shown in Figure 4. Using a continuous locking technique, the surgical wound was sutured with synthetic absorbable sutures. Intraoperative ultrasound showed a decrease in the size of the right hematosalpinx. The other essential data is shown in Table 1.
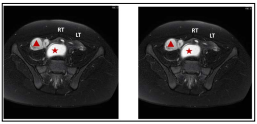
Figure 2: Case 2 Magnetic resonance imaging images. A. Coronal view, B Axial view , RT showed right horn of uterus, LT showed left horn of uterus, Red star showed hematocolpos, Red triangle showed right hematosalpinx
Table 1: Summary information of case series
| Clinical manifestations | Case 1 | Case 2 |
|---|---|---|
| Age | 9 years and 9 months old | 11 years and 2 months old |
| Symptoms started | 9 months after menarche | 6 months after menarche |
| Presenting symptoms | Chronic pelvic pain, urinary retention, dysuria, pelvic mass 18 weeks size with cystic consistency | Right lower quadrant pain, urinary tract infection |
| Anomaly | -Uterine didelphys and double vagina, ipsilateral right renal agenesis -Hematocolpos 10 cms at right side of vagina with brownish content 700 ml. | -Uterine didelphys and double vagina, ipsilateral right renal agenesis -Hematometrocolpos 5 cm at right side of vagina (with brownish content 300 ml.) and hematosalpinx |
| Operative time | 1 hour 15 minutes 1 | 1 hour 55 minutes |
| Pathology results | Benign squamous epithelium with acute and chronic inflammation | Chronic and acute inflammation |
| Follow up/ Recurrent | 1 year, no recurrent | -At 3 month after surgery showed no hydrosalpinx -At 2 year, no recurrent |
Both cases were operated on and started with vaginoscopy to explore and identify the vaginal, cervix, vaginal septum and hematocolpos size. Then the surgical site was marked with a surgical marker identifying an actual location to excise. This step will help the surgeon resect the vaginal septum sufficiently to prevent a recurrence but not too much so that the urethra and cervix are injured. However, the main obstacles to operation are the small vagina and greater depth of the vaginal canal, which make the physician unable to explore and resect all the septum. For this reason, our team developed the vaginal retractor, made from high-grade stainless steel in an L-shape with different sizes. This retractor can be used on both arms; one side is the vaginal retractor, and the other is the handle. The smallest size is 1cm width x 7 cm depth. As we know, OHVIRA syndrome is most presented shortly after menarche. The patients are mainly in the early puberty period without a history of sexual activity. The procedure could be more complex, requiring a smaller instrument and deeper exploration of the vaginal septum and cervix. So, we designed the shape of the device as an L-shape, and the longer holding part will differ by size for diffferent patients, as shown in Figure 3. The septum that we resected is shown in Figure 4. Furthermore, the surgeon used the innovative vaginal retractor in the operation room to create excellent surgical field visibility.
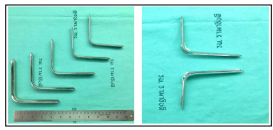
Figure 3: Innovative vaginal retractor for young age patient

Figure 4: The vaginal septum from Case-2, tissue sized 5 x 2 x 0.5 cm
After the procedure, both patients were admitted to the hospital to observe their conditions. Their vital signs are all stable; there is no fever. Pain score was minimal, 1 to 2 (pain score 0 to 10; 0 means no pain), without the use of any analgesia or antibiotic. They were admitted to observe for one day after the operation and discharged on the next day. They both have only minimal bloody discharge from the vagina. Moreover, a few months after the procedure, they have no abdominal pain, dysmenorrhea, or urinary symptom. We also did an ultrasound every time they visited the outpatient unit, and they showed no new pelvic mass. Especially for the second case, the ultrasound showed complete resolution of the right hematosalpinx in the third month after the operation. At the recent follow-up, both patients showed no recurrent abnormal symptoms and pelvic masses. We still follow up for long-term consequences and recurrence of the vaginal septum.
OHVIRA syndrome is one of the female genital tract anomalies caused by the abnormal development of paramesonephric and mesonephric ducts in the embryonic period [6]. In the classical case, abnormal development of the mesonephric duct leads to agenesis of the kidney. Failure of this process will result in the ipsilateral mullerian duct developing more lateralized, leading to fusion loss with the contralateral paramesonephric duct, causing uterine didelphys [7]. Also, malformation of the hemivagina and urogenital sinus causes obstruction, resulting in hemivaginal obstruction. Related to the abovementioned, classical OHVIRA syndrome will present with the uterine didelphys, renal agenesis and hemivaginal obstruction approximately 72.4% from previous literature [5]. However, there could be rare variations in anatomy that may require more procedures, such as septate bicollis uterus, unilateral cervical atresia, dysplastic or atrophic kidney, or ectopic ureter (insertion into the vagina) [3, 5]. Not only variation in anatomy, but some cases are also present at uncommon timing, prepubertal or newborn period, were recorded about 45 cases in 11 years followed up [3].
The classification of female genital tract anomalies was described as AFS 1988/2009 (The American Fertility Society), ESHRE/ ESGE 2014 (The European Society of Human Reproduction and Embryology/ European Society for Gynaecological Endoscopy) or ASRM 2021 (The American Society for Reproductive Medicine) [8-10]. All the descriptions depended on the abnormal findings of the female genital tract. The literature’s specific classification for OHVIRA syndrome showed two classifications, for example, 1. Rock and Jones classification 2 [11]. New Chinese classification by Zhu L. et al [12]. These two classifications are different, the former is classified by location of an anatomical defect of the septum (which explained the outcome of hematocolpos), but the latter is classified by complete or incomplete obstruction of the hemivagina. However, all of these classifications are not correlated with their associated anomalies. In the uncommon case of OHVIRA, there can also be unusual periods, such as in the newborn, prepubertal period, or presenting with multiple variants [3, 4, 13]. A review of 734 cases showed dysplastic or multicystic kidney (7.8%), endometriosis (13.6%), a single uterus (0.4%) or in other case reports, an ectopic ureter or a duplicated ureter [14-16] . From this information, this condition is quite rare and can be caused by misdiagnoses [17]. Awareness and careful evaluation are very important to prevent unnecessary operations and complications of surgery. In untreated cases, the accumulative content can result in hematosalpinx, endometriosis, pelvic adhesion, pyosalpinx, or pyocolpos [18, 19].
Diagnosis of OHVIRA syndrome need a combination of tools to help for diagnose. A physical and pelvic examination is essential for patients presenting with abnormal symptoms. On the other hand, pelvic examination as a routine is hardly ever done because this syndrome occurs early after menarche or even in newborns. So, imaging is essential to help physicians diagnose and guide subsequent proper management, which includes ultrasonography and MRI. In some situations, valuable tools are limited. Other tools may help, such as hysterosalpingography (HSG) and Computerized Tomography Scan (CT) scan. However, the alternative imaging is less likely to be used because of the limited anatomy information, which is crucial for the surgical plan and management. The essential investigations include ultrasound and MRI, which help diagnose accurately. The accuracy of ultrasonography in diagnosis was about 90-92%. Presently, MRI is the gold standard for diagnosis [20-22].
For the standard treatment of OHVIRA syndrome with symptomatic, the vaginal septectomy releases accumulating blood from an obstructed hemivagina, hematocolpos, or hematometrocolpos [6]. The main purposes of treatment are to: 1. Corrected proper anatomy for menstrual release 2. Prevent the recurrence of the vaginal septum and operative complications and 3. Preserve fertility function. Nevertheless, there is still no specific method or definite guideline for management. The most important factors are a uterine anomaly and variation of coexisting anomalies.
Occasionally, distortion of uterine anomaly makes it difficult to do transvaginal resection and may require a unilateral hysterectomy [23]. From the previous literature, there was the recommendation (the American College of Obstetricians and Gynecologists committee opinion in 2019) for acute obstructive uterovaginal anomalies, for example, imperforated hymen, distal vaginal atresia, and OHVIRA syndrome [24]. Currently, there is a suggestion for using vaginoscopy to assess anatomical structure and excision of the septum. Another formerly information by N.A. Smith et al, specified for OHVIRA syndrome, had described surgical management. They proposed that the definitive treatment is vaginoplasty or vaginal septum resection. Nevertheless, for the narrow vagina in adolescent girls, a single procedure may not be enough to complete the surgery. They suggest one and two-stage surgery (the first surgery aims to release hematocolpos, and the second surgery is for resecting the excess septum) [16] . However, two-stage surgery is preserved for young patients or when it is extremely hard to expose the vaginal septum. These patients will reoperate after vaginal remodeling (maturation of vaginal epithelium and increase vaginal sized) [25]. In addition, minimally invasive surgery was introduced as the optional surgery for OHVIRA syndrome, with the benefit of hymenal preservation, being less invasive, and causing less pain for the patient. The recurrence of the septum is still under investigation. According to the previously provided information, we concluded that the surgical option for managing OHVIRA syndrome is shown in Table 2. There is less information about the recurrence rate using the different methods.
Table 2: Surgical options of OHVIRA syndrome
| Operative options | Procedures | Procedures | Advantage | Disadvantage | Recurrent or complication |
|---|---|---|---|---|---|
| Transvaginal approach | Traditional procedure Vaginoplasty (septum resection) | Standard procedure | - Definite treatment - Properly excised and prevent recurrent | - Limit exposure in young age - Hymen injured | 11 -20% [18, 26] [27] |
| Vaginoscopy and septum resection | Optional/Advance procedure | - Good visualization - Preserve hymen integrity | - Need experience laparoscopic surgeon - Need specific instrument -Thermal injuries are under debated | Less information [28] [29] [30] | |
| Transvaginal combined with transabdominal approach | Laparotomy or laparoscopy | - If cannot approach only by vaginal route or need more information | - Identified uterine anomaly and additional surgical intervention maybe required | - Maybe unnecessarily interventtion (salpingectomy, hysterectomy) | No data available |
In our case reports, both cases presented with abdominal pain within a short period (6-9 months) after menarche. The main presentations related to urinary tract symptoms, urinary retention and infection were not the classical presentation in OHVIRA syndrome. The main investigations were ultrasonography and MRI. Multidisciplinary teams, including pediatricians and urologists, were prepared and discussed the procedure and possible complications with the patient and family. The operation was scheduled for the next few days after the diagnosis. Intraoperatively, both cases initiated the process with vaginoscopy followed by septum resection, as described above. As the young age of patients, narrowing of the vagina and the septum are difficult to approach. The septum is deep inside from introitus, along with the vaginal canal which extends to the posterior fornix of the vagina. As we mention, the visibility of the lesion and operative field were limited. We used the new instrument to improved this limitation and help the surgeon operate adequately. The main goal is to resect the excess septum as much as possible to prevent recurrent septum and avoid injury to adjacent organs. With the new instrument, the surgeon can resect the septum adequately, and there were no recurrences or complications up to 2 years of follow-up. Compared with a hysteroscopy, the other benefits of this instrument were that it was reusable, had a low price and could be used by general gynecologists. Physicians can use this tool to correct the septum without vaginoscopy and with less injury to a patient. In the second of these case reports, another essential condition is hydrosalpinx. In our second case, we did not do the laparoscopy to explore the hematosalpinx. We expected the lesion to be resolved after a drainage operation, as described in the literature [16]. We followed up on the clinical and ultrasound at 1st month and 3rd month after the procedure. The patient showed no pelvic pain, no genital pain, and regular menstruation. The ultrasound showed a decrease in size in the first month and a resolved hematosalpinx in the third month after surgery. So, laparoscopy or laparotomy for salpingectomy is not recommended as routine procedures because there can be recovery after release of hematocolpos.
The other options of management, which are still under debate, are to introduce the incision for release of the hematocolpos by hysteroscopic scissor, electrocautery (L-hook electrode) or laser. This technique has the advantage of preserving hymen integrity, which is important in some populations and is called the “notouch” technique. However, the data about recurrence and thermal injury complications must be explored. Recently published data showed that the Holmium laser, an electrothermal bipolar vessel sealing device, may not be sufficient for removing a thick vaginal septum. There are still differences in the details of preoperative management and the technique of traditional septum excision, such as the role of preoperative hormonal treatments or whether to suture the wound after excision [14]. The previous data showed more conservative options for patients in the prepubertal age group. The retrospective study from Han JH et al in 43 cases of prepubertal patients showed that only 13% of patients required an operation [3]. In patients aged less than six months, they followed up on the patient’s condition. Vaginal aspiration was performed in the huge vaginal mass, compressing the urinary tract. The non-surgery group followed up and found that one-half still may require an operation. So, in the special age group, counseling with the family is important for a management plan; more treatment options must be discussed. In some literature, the surgical incision was done to release accumulating fluid and follow-up. The future intervention was postponed until puberty [13].
After an operation, follow-up, complication, and recurrence are very important. Complications and recurrent could be adhesion in the vagina, vaginal stenosis, or recurrent septum. The recurrence rate for traditional vaginal septum resection varies between 5-20%, with a follow-up period of up to 20 years [18, 26, 27]. The recurrence rate of vaginoscopic incision and resection of the vaginal septum is still unknown due to only a short period of followed-up. The literature showed follow-up up to 1 year with no recurrent septum. Some literature showed recurrence within three months after surgery [28-31]. Therefore, vaginoscopic resection still needs more research. The other important long-term outcome is an obstetric outcome. A previous study showed that, after surgery, successful pregnancies were about 77% [5].
OHVIRA syndrome standard management is the surgical treatment of excised vaginal septum. The main operation techniques are still transvaginal, with a traditional approach or vaginoscopy with resection. However, subtle anatomical differences can modify the therapeutic approach. Long-term recurrent and follow-up needs to be investigated, and fewer data due to rare conditions. Here, we show an innovative instrument developed for improved outcomes of operations that is reusable and durable and can be the alternative instrument for improved surgical procedures in OHVIRA syndrome.
We want to thank Anusorn Adirekkittikun for making the innovative vaginal retractor in this work possible. This research did not receive a specific grant from any funding agencies. The authors have no conflict of interest.
