Author(s): Jenifer B Ellecom, Ian Shaw and Gary G Adams*
Background: Obesity has been on the rise in developed and developing countries such as Nigeria. Data from the WHO demonstrated the prevalence of obesity increased by 15% between 2002 and 2016 in Nigeria. Here, we examine the rate of obesity in Nigerian adults and the associated cause and impact on the population.
Methods: An electronic search was conducted from November 2020 to October 2022 across PubMed, PMC, Science Direct and NU search. A formal search strategy was used to combine the keywords. The retrieved studies were filtered through inclusion and exclusion criteria. Fifteen studies were included in this systematic review. The data of the included studies were extracted using the Critical Appraisal Skills Programme (CASP) checklist and results analysed with Revman meta-analysis.
Results: Three key themes were identified across the 15 studies: socio-economic status, sedentary lifestyle and diet-associated obesity. Obesity was found in an average of 22% (n=1042) and 34% (n=2361) females and males, respectively. As such, the rate of obesity was overall significantly higher in Nigerian females than males.
Conclusion: The prevalence of obesity in Nigeria was high with Nigerian adult females more affected. The high rate of obesity was associated with non-communicable diseases (NCDs) such as gestational diabetes, diabetes mellitus, stroke, cardiovascular disease and cancer. Support from health care professionals, nursing practitioners and governmental interventions are required to reduce the burden on and the deterioration in Nigerian adults’ health and wellbeing.
According to the World Health Organisation (WHO) (2016), since 1975, global obesity defined as a non-communicable disease has tripled, with an estimated 650 million adults worldwide. During that period, the rate has increased from 21.5% to 38.9% with over 3 million people dying globally every year with no signs of a decline (WHO, 2016).
Obesity arises as a result of accumulated excess body fat in individuals caused by high consumption of unhealthy energy dense foods, sugar and saturated fats (junk foods) and beverage drinks (beer, coca cola) (WHO, 2016). An unhealthy dietary pattern combined with reduced physical activity (sedentary lifestyle) enhanced the risk of an individual gaining weight and becoming obese [1]. Consequently, according to a previous study by Sola et al. (2011), unhealthy lifestyles led to obesity associated with adverse effects on health such as hypertension, cardiovascular disease (CVD), dyslipidaemia, stroke, cancer and diabetes mellitus [2]. For this reason, WHO (2015) described obesity as a complex disease (WHO, 2015) with other factors, such as genetics and social-economic status, also having an influence on the prevalence of obesity in individuals [2, 3].
To assess the prevalence of obesity, various measurement tools, such as the waist- hips ratio (WHR) could be used. The WHR measured the waist-hip circumference determines the amount of fat stores in the waist, hips and buttocks of an obese individual [4]. However, Lear et al. (2010) stated there are ethical issues associated with WHR. For example, WHR cut-off points varies among ethnic groups. There are specific cut-off points for populations in South-America, Europe, Asia and Africa as body compositions differ. Thus, according to the body mass index (BMI) is the most reliable measurement tool [5].
The BMI measures individuals’ body fat based on the weight in kilograms (kg) and height in meters (m2 ). As such, the BMI is subdivided in criteria [5]. A normal BMI is between 18.5 - 24.9 kg/m2 . A BMI of 30.0 - 34.9 kg/m2 is classified as class I obesity (low- risk), whereas class II (moderate- risk) is a BMI of 35.0 - 39.9 kg/m2 . A BMI greater than 40.0 kg/m2 is seen as high-risk and classified as class III obesity (Pletcher, 2016). WHO (2017) predicted over 1 billion adults worldwide would have a high BMI by 2025 [6].
Globally, obesity is seen in children and adults and the rise in
obesity has resulted in a major public health concern in numerous
high-income countries including North America and Europe.
Countries in the Middle East (e.g., Pakistan) and Latin America
(e.g., Brazil) also reported a similar effect with obesity with
increased female prevalence. In 2016, more than 20% of females
were obese in 14 Latin American countries and in the Middle
East over 30% of females. The high percentage of obesity has
resulted in a regional shift in many countries, a shift also seen in
Sub-Saharan African countries, where more than 1.9 billion adults
were either overweight or obese in 2017 [6,7]. Countries in the
Sub-Saharan Africa were slowly transitioning from a traditional
diet, that contained high amounts of fibre and carbohydrate and
low amounts of sugar and fat, to a diet high in saturated fat, energy,
sugar and sodium as compared to Western countries. Despite this
slow nutritional transition, the rate of obesity appears to have
significantly increased in Nigeria [5].
Nigeria, a country located on the western coast of Africa is a
federal republic and comprises 36 states, with the official language
being English as a result of colonisation, which started in 1901
and ended in 1960 [8].
Since Nigerian independence, it has endured decades of political instability and economic inequality, which has had a negative impact on the country’s education, nutrition, health care system and the entire country. For example, most of the Nigerian population live in deprived areas [9]. A previous report by the National Bureau of Statistics in 2020, stated more than 40% (84.8 million people) of the total population (212 million people) in Nigeria live in poverty (National Bureau of Statistics, 2020). However, people living in larger Nigerian cities such as Lagos and Abuja where there is rapid economic development, are more likely to find a job (e.g., office job, roadside trading). As such, they are financially capable to consume varieties of foods and have more accessible facilities (e.g., healthcare) to improve their living condition. Thus, the inequality in the economic status impacts greatly the health of many Nigerians, where obesity has been on the rise. Data from WHO between 2002 and 2016 illustrated the prevalence of obesity in Nigeria with an increase of approximately 15%. The highest rate of obesity was reported in the South- East and North-East Nigeria. Nearly 40% (n= 364) of the people who lived in the South-East were obese with approximately 30% (n= 209) in the North-East. In 2020, an estimated 12 million individuals presented with obesity in Nigeria. The high rate of obesity led to an increase in non-communicable diseases (NCDs) such as diabetes mellitus (WHO, 2020). Estimated 5.8% (n= 6 million) of Nigerians adults were diagnosed with diabetes mellitus in 2018 with a consequential impact on the mortality rate [10]. According to the WHO (2021), NCDs accounted for nearly 30% of all deaths in Nigeria of which 3% related to diabetes and 12% CVD [11].
Ezeigwe et al. (2020) explained demographic changes, growing
income, and sedentary lifestyles, cultural perceptions, lack of
education, fertility and the intake of highly processed diets were
the drivers for nutritional, socio-economic and western inequity
attributing to obesity in Nigeria [12]. Moreover, Bosely (2014)
analysed the obesity prevalence data and stated it was higher in
females than males, a possible reason that Nigerian males were
likely to be taller than the female counterparts [13].
The high prevalence of Nigerian obesity also impacts on the
quality of life (QoL), self- esteem, productivity and the health
of Nigerian individuals [13]. This negatively impacts health
care costs in treating obesity with medical care, mediation and
physician consultation costs for obese individuals with NCDs
nearly three times higher (E172) than the cost for non-obese
Nigerian individuals (E69) [14, 15].
Garba et al. (2016) also stated there were more obese individuals
admitted to the hospitals than non-obese individuals. This increase
in obese patients increased the pressure and burden on health care
professionals. For example, not all hospitals had suitable facilities
[15]. With the potential high medical bills or expensive medication
requirements, medical treatment was not always immediately
sought among most Nigerians and as such late disease diagnosis
impacted mortality rates associated with obesity [16].
Here, we examine the associated cause and impact of obesity in
Nigerian adults.
Pubmed, PMC, ScienceDirect, NUsearch and British Medical Journal were searched from 2011 to 2019 using a broad search strategy to identify all potentially relevant publications. The text words contained in the titles and abstracts of relevant articles and the index terms used to describe the articles were used to develop a full search strategy. The search strategy, including all identified keywords and index terms, was adapted for each database source included. Initial keywords used in this review were“obesity”, “Nigerian”,“adults”,“cause” and“impact” together with the Boolean operator“AND” or“OR”. Finally, additional studies were searched for in the reference lists of all identified reports and articles. 150 studies identified and removed as duplicates. The titles and abstracts of remaining 126 articles read and 60 studies excluded using the pre-determined inclusion and exclusion criteria. Sixty-six articles further screened and full-text assessed for eligibility. A total of 15 papers met the inclusion criteria and 51 articles were added to the excluded studies. The overview of the search result was presented using a PRISMA flow diagram. A Critical Appraisal Skills Programme (CASP) checklist was used to assess, evaluate and critique the included papers.
Studies were included if they met the following criteria: 1) subjects were Nigerian population diagnosed with obesity and ≥ 18 years old; 2) studies of obesity interventions that measured the BMI (body mass index), waist- hip ratio, dietary measurements and questionnaires; 3) studies that reported the rate of obesity between Nigerian males and females; 4) the onset of obesity class I, II and III were reported as outcomes; 5) studies: descriptive and cross-sectional studies. Studies were excluded if they were in a language other than English, published before 2000, case studies and systematic or narrative reviews.
A process of screening and supplementary search parameters were used to ensure relevance to the topic and duplicate articles were removed. Following abstract review, studies were excluded if they were not primary research, unrelated to obesity, excluded non- Nigerian ≥ 18 years old and young Nigerian ≤ 18 years old as participants, non-English language or did not have full text available for the review. The full text of selected studies was assessed in detail against the inclusion criteria by two independent reviewers. Reasons for exclusion of full-text studies that did not meet the inclusion criteria were recorded and reported. The results of the search were reported in full in the final report and presented in a Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram.
The selected studies were critically appraised for methodological quality using the Critical Appraisal Skills Programme (CASP) checklist and checked with the second reviewer.
Data from the selected studies were extracted using standardised data tables to bring all data together for easy reference. These included author/year/country, sample size, age range, intervention, clinical and study outcomes.
Data analysis was conducted using the RevMan meta-analysis Review Manager 5.4.1. Tabulated data of the mean difference and standard deviation between obesity in females and males were extracted from the included studies at three criteria (socioeconomic status, sedentary lifestyle and diet). Meta-analyses were performed separately according to each criterion to estimate the rate of obesity by using random effect models depending on the level of heterogeneity. Outcomes were reported as mean difference with 95% confidence intervals (CIs). Heterogeneity was measured using the I2 index. A p-value less than 0.05 was considered statistically significant.
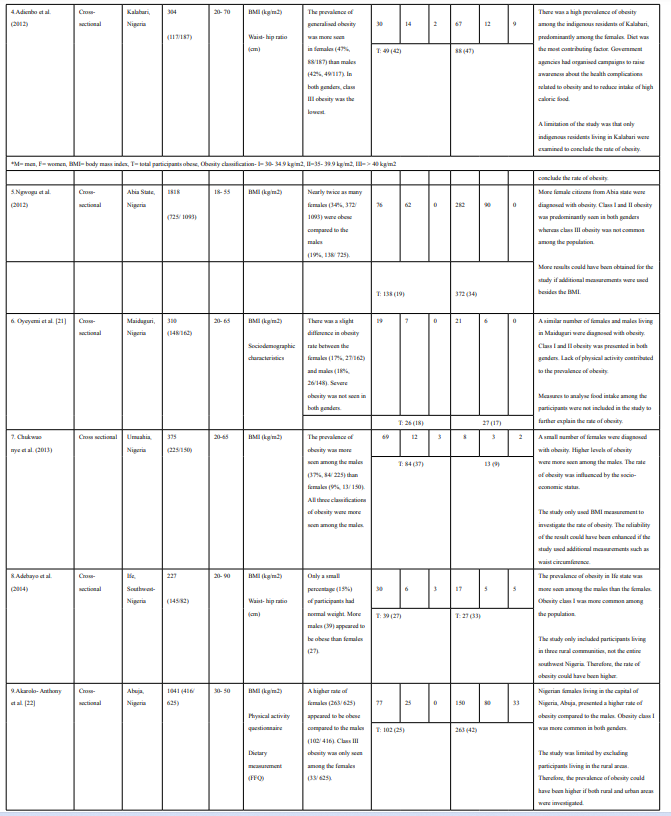
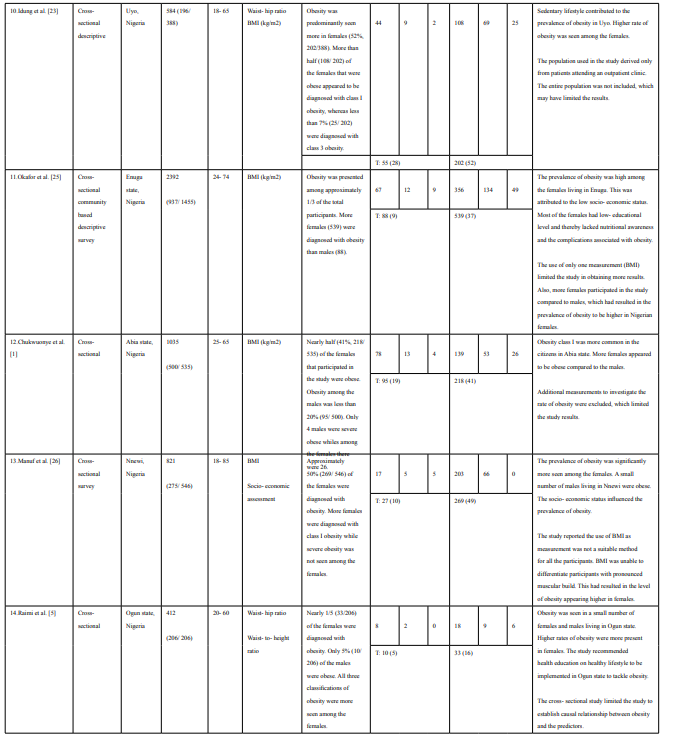
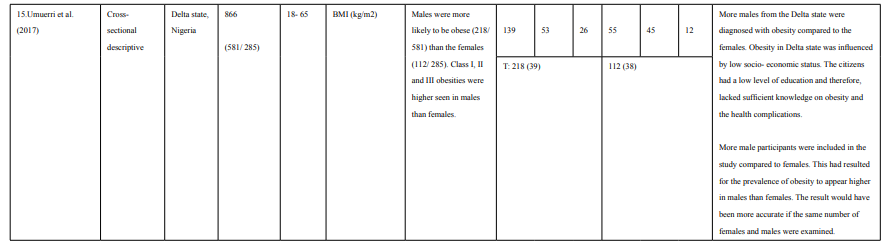
Five studies comprising 5495 participants used the BMI to measure how low socio- economic status in Nigeria influenced the prevalence of obesity. A combined effect of the results demonstrated that 1196 (21.8%) Nigerian females and 519 (9.4%) Nigerian males were obese. The effect size indicated a statistically significant mean difference of 17.17 (95% CI, 12.64, 21.70) between the obese Nigerian females and males (figure 2). Although obesity was more common among Nigerian females, the number of Nigerians with class I and class III obesity were higher in the males. Approximately 70% (n= 369) of the Nigerian males had a BMI of 30.0- 34.9 kg/m2 (class I obesity) and nearly 9% (n= 43) were severe obese. However, among the Nigerian females, the percentage was slightly lower. Nigerian females that were diagnosed with class I obesity was 64.5% (n=772) and 8% (n= 96) had class III obesity. Class II obesity was more common among the Nigerian females (27.4%, n= 328) compared to the males (20.6%, n= 107) (Table 1 and 2).
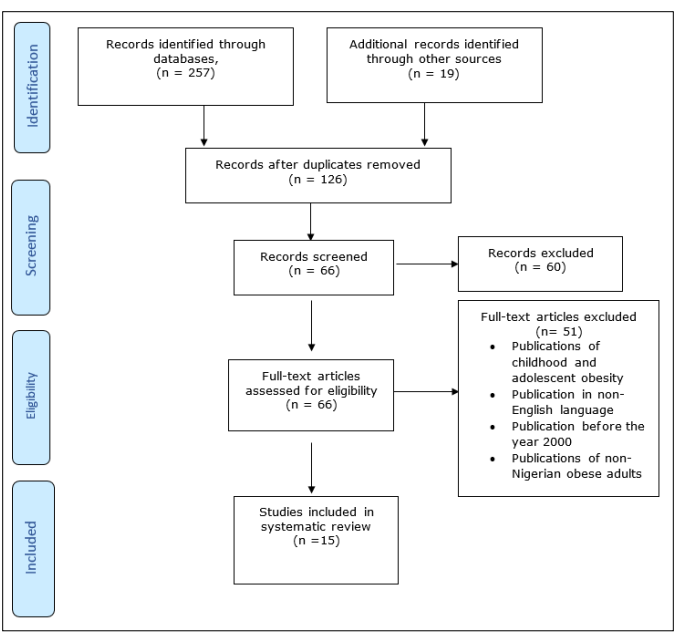
Figure 1: PRISMA Flow Diagram Identifying Studies Included [17]
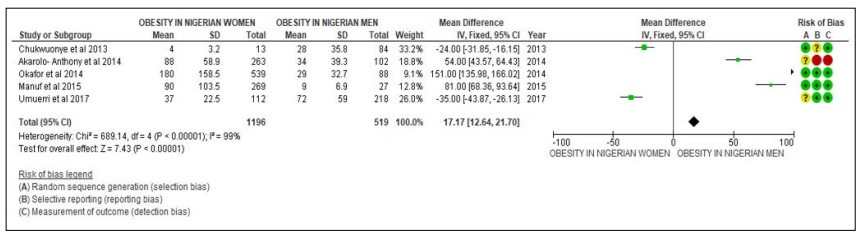
Figure 2: Forest Plot of Comparison: Association between Socio- Economic Status and Prevalence of Obesity in Nigerian Women and Men Outcome: Women were More Likely to Become Obese Affected by Low Socio- Economic Status
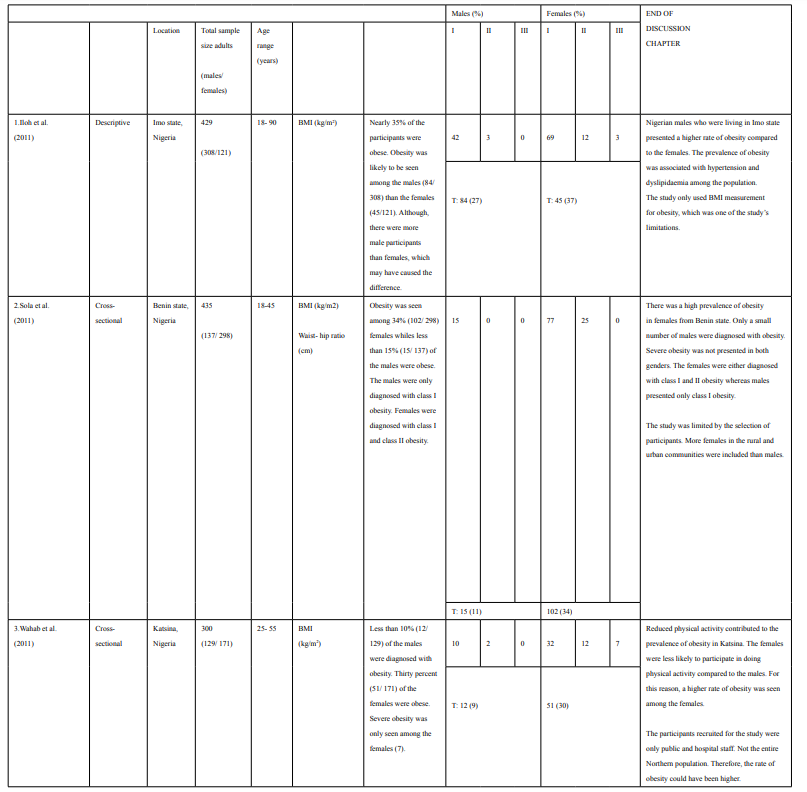
| Obesity Classification | ||||||
|---|---|---|---|---|---|---|
| Class I (BMI 30.0- 34.9 kg/m 2 ) |
Class II (BMI 35.0- 39.9 kg/m2 ) |
Class III (BMI > 40.0 kg/m2 ) |
||||
| % Females | % Males | % Females | % Males | % Females | % Males | |
| Socio- economic Status | 64.5 | 71.1 | 27.4 | 20.6 | 8 | 8.7 |
| Sedentary Lifestyle | 67.3 | 65.1 | 27.6 | 34.0 | 5.1 | 0.8 |
| Diet | 71.1 | 80.2 | 20.6 | 16.1 | 8.3 | 3.7 |
Five studies with 3424 participants reported the association of sedentary lifestyle and obesity in Nigeria. A combined effect of 685 (20%) Nigerian females and 241 (7%) males were either diagnosed with class I, II or III obesity. The effect size indicated a nonstatistical significance between obese Nigerian women and men with an effect size of 27.92 (95% CI, 11.41, 44. 44) (see figure 3). The result showed obesity was more common in Nigerian females than males. Furthermore, class I obesity was found among 67.3% (n= 461) of the 685 Nigerian females, whereas class II was seen in 27.6% (n= 186) females. Less than 10% (n= 38) of the females were severe obese (BMI >40 kg/m2). Class I obesity was also higher among Nigerian males (65.1%, n= 157), whereas 34% (n= 82) of the males were diagnosed with class II obesity. Only 0.8% (n= 2) of the males appeared to have class III obesity (Table 1 and 2).
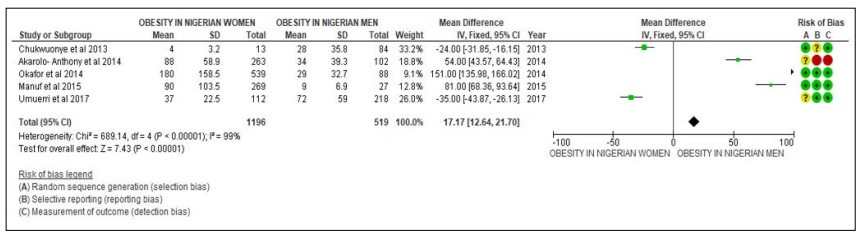
Figure 3: Forest plot of comparison: Association between sedentary lifestyle and prevalence of obesity in Nigerian Women and Men outcome: Significantly, a higher number of Nigerian women became diagnosed with obesity as result of sedentary lifestyle compared to Nigerian men
Five studies with 2430 participants investigated how diet increased the risk of obesity in Nigeria. A combined effect of 519 (21.4%) Nigerian females and 243 (10%) males were either diagnosed with class I, II or III obesity. This indicated the prevalence of obesity was more common in Nigerian females than males when diet influenced the obesity rate. More so, the effect size indicated a nonstatistical significance between obese Nigerian women and men with an effect size of 15.59 (95% CI, 11.83, 19.35) as shown in figure 4. Class III obesity was the least seen among the participants. Nearly 50 (8.3%) of Nigerian females and only 10 (3.7%) Nigerian males were severe obese due to unhealthy dietary pattern. Approximately 400 and 200, Nigerian females and males respectively, had a BMI of 30.0- 34.9 kg/m2. More so, the difference in the number of Nigerian females and males with class II obesity was nihil. One fifth (n=107) of the females and 16.1% (n=39) of the males were moderate (class II) obese as shown in table 1 and 2.
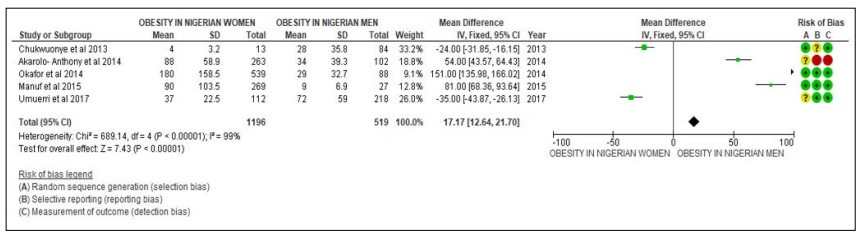
Figure 4: Forest plot of comparison: Association between diet and the prevalence of obesity in Nigerian Women and Men outcome: more Nigerian women were obese compared to Nigerian men as result of their diet
The first theme of this review investigated the association between socio-economic status and the prevalence of obesity among Nigerian adults. Five included studies (Akarolo- Anthony et al. 2014; Chukwonye et al. 2013; Maruf et al. 2014; Okafor et al. 2014; Umuerri et al. 2018) found there is a significant association between the socio-economic status and obesity in Nigeria. According to 4 of the studies (Akarolo- Anthony et al. 2014; Maruf et al. 2014; Okafor et al. 2014; Umuerri et al. 2018), higher rates of obesity levels were seen more in Nigerian females than males. The studies explained that low socio-economic status such as low educational levels among Nigerian adults contributed to the prevalence of obesity [22, 24-26]. Akarolo- Anthony et al (2014) advocated that there was an increased number of Nigerian adults who only completed primary school or did not have any formal education during their younger years. This prevented those adults, especially Nigerian females, to have sufficient knowledge on healthy lifestyle whiles growing and may had contributed to become obese [22].
Also, the study by Maruf et al. (2014) stated that there were more Nigerian females than males that did not attend school due to their parents’ financial instability or supported the parents by selling food products from an early age to sustain the family [26]. A recent article published by Unicef (2021) analysed only 47.7% (n= 2.5 million) of Nigerian females attended primary school in the Northern part of Nigeria in 2019. This meant that more than half of the females did not have education from a young age [27]. As a result, those females did not have the opportunity to learn how to read and found it difficult to understand or were unaware of the importance of a healthy lifestyle when they became adults [26]. According to Carlisle (2012), the disadvantage of being unable to read reduced the knowledge of an individual. For example, it prevented an individual from educating and increasing their awareness on obesity by reading books related to health or leaflets provided in hospitals. It also resulted in fundamental life skills and enhanced knowledge on aspects surrounding unhealthy lifestyle that led to the development of obesity to narrow [28].
More so, Vermon (2013) explained low literacy made it difficult for an individual to understand and follow health instructions given by health professionals. The findings showed low literacy contributed to nearly one third (n=189) of individuals experiencing health complications as a result of poor understanding to adapt to a healthier lifestyle (Vermon, 2013). However, Arena et al. (2018) recommended the government in Nigeria to organise health events to increase obesity awareness among Nigerian adults. Health events provided the opportunity for individuals to ask questions and have information explained in- depth to enhance their understanding [29].
High socio-economic status was associated with great odds for obesity to develop in Nigerians as well. The study by Chukwonye et al. (2013) investigated the rate of obesity in Lagos [24]. Chukwonye et al. (2013) found that among the 97 participants, nearly 87% (n= 84) were obese males. ’Unlike the other included studies (Akarolo- Anthony et al. 2014; Maruf et al. 2014; Okafor et al. 2014; Umuerri et al. 2018), where the findings demonstrated higher rate of obesity was seen in females, Chukwonye et al. (2013) study showed obesity appeared more in males [22, 24-26]. According to Amira et al. (2011), Lagos is one of the largest cities in Nigeria and the fourth wealthiest city in Africa. The presence of universities provided most Nigerian males who were living in Lagos the opportunity to achieve a high educational level, which secured a lucrative career and became financially more stable. The stability supported those males to adapt to a lifestyle they preferred, which was often adapted from the western lifestyle [30]. For example, Ayodele et al. (2019) analysed some Nigerian males tended to eat more outdoors. They consumed take- away foods (high in carbohydrates and saturated fats) purchased from international food chains sited in Lagos such as Domino’s Pizza and Kentucky Fried Chicken. As those Nigerian males adapted to such eating patterns, their energy intake increased and they gained weight easily [31]. Although, Renzaho (2014) insinuated that Nigerian males deliberately adapted to such eating patterns as a large body size symbolised high social status in Nigeria. Nigerian males who had a normal body size or a slim figure - remove number 1) showed signs of poverty and deprivation. Therefore, regardless of their awareness of health complications associated with obesity, the perception of large body image was usually accepted positively. It was characterised as having a status, being rich and culturally powerful [16].
On the contrary, Agha (2017) suggested highly educated Nigerian females’ perspective on obesity differed from the males. Most females experienced low self- esteem when they were obese and rather desired having a normal weight according to the BMI [32]. For this reason, high socio- economic status contributed for the likelihood of obesity to be higher in Nigerian males than females as shown in the findings. The study reported only 13 out of 150 females were obese [24].
The second theme for this systematic review examined the association between sedentary lifestyle and obesity the based on the included five studies (Idung et al., 2014; Ngwogu et al., 2012; Oyeyemi et al., 2012; Raimi et al., 2015; Wahab et al., 2011), Nigerian adults gained weight as result of reduced physical activity [5, 19-21, 23]. Idung et al. (2014) found that among the 584 participants were living in Uyo, South- Nigeria, 257 were obese [23]. The rate of obesity was higher in females (n= 202) than males (n= 55). According to Idung et al. (2014), there were several socio-cultural barriers for Nigerian females to participate in doing physical activities, which resulted in the high prevalence of obesity [23]. For example, Nigerian females who exercised were often perceived as a persistent myth. Some Nigerians believed females became muscular and gained a posture of a male when actively involved in exercise. Such body shape appeared unattractive and often intimidated men [23]. Therefore, most Nigerian males preferred females with curvy hips and thick thighs, also known as a pear-shaped body. As such, the societal stereotyping of the gender role caused physical exercise and sports to appear more appropriate for Nigerian males than females. Nigerian females were therefore frequently excluded from participating in exercise, which promoted weight gain [33].
To eliminate the gender discrimination surrounding physical activity in Nigeria, several interventions and policies such as the National Gender Policy, were implemented. The National Gender Policy was established by the Government of Nigeria in 2006. The policy focused on promoting gender equality between females and males in Nigeria. One of the objectives of the policy was to adopt gender mainstreaming as an important value and practiced in social transformation, organisational cultures and in the general policy in Nigeria. The objective was to develop and strengthen appropriate educational, training and institutional frameworks that connected the macro- policy environment with the micro level where females, males and communities experienced gender inequality. This supported the minimisation of the traditions, customs and sexual stereotyping of social roles and cultural prejudice in Nigeria. Some Nigerian females enjoyed their rights and fully participated on an equal basis with the males in national development. Those Nigerian females felt empowered and motivated to participate in different life activities, which positively influenced their health. However, not all Nigerians were familiar with the policy. As a result, gender inequality was still present among Nigerians (Ajayi, 2021).
Research conducted by Arslan et al. (2017) coincided with the National Gender Policy. Arslan et al. (2017) agreed promoting gender equality changed the perception and cultural beliefs of people. Such intervention increased the awareness of males of the importance of allowing females to participate in physical activities and sport. Arslan et al (2017) highlighted females who were more physically active were for example less likely to experience gestational diabetes during pregnancy. It reduced the risk of females to encounter diabetes mellitus later in life or death of the baby before or after the birth. As such, less medical attention was needed during pregnancy [34]. Therefore, promoting gender equality had a positive effect on the health of predominantly females (Ajayi, 2021).
Besides socio-economic status and sedentary lifestyle, diet influenced the obesity rate among Nigerian adults as well. Traditional food in Nigeria contained high starch and saturated fats. For example, the most common local food in Nigeria, pounded yams and garri, were both rich sources of starch (Okeke, 2018). According to Raman (2017), consuming an adequate amount of starchy food stimulated weight gain. Starchy food contains a high number of calories. It added bulk to meals and thereby boosted the risk of an individual to become obese (Raman, 2017).
The findings of the included study by Sola et al. (2011) illustrated 34% (n=102) Nigerian females living in Benue state were diagnosed with obesity, whereas among the males only 11% (n=15). Sola et al. (2011) implied as Nigerian females were mostly home, they consumed high calorie snacks or an adequate number of meals in a day that were high in starch. This contributed to weight gain in Nigerian females especially if they were also less physically active during the day, unlike Nigerian males. Sola et al. (2011) suggested the low percentage (11%, n= 15) of Nigerian males being obese was due to the males usually being the breadwinners in the home [2]. Nigerian males were more occupied with work during the day and consumed less meals. Also, the work stimulated the males being physically active, burned calories effectively and thereby prevented weight gain [10]. For those reasons, the study showed the number of Nigerian males diagnosed with obesity was lower than in females [2].
More so, Adienbo et al. (2012) and IIoh et al. (2011) analysed Nigerian adults, predominately females and found they consumed meat in large quantities. Both studies found the rate of obesity was significantly higher among Nigerian females than males [18]. Obesity class I, II and III were seen in both genders. There were 47% (n=88) Nigerian females and 42% (n= 49) Nigerian males obese in the findings by Adienbo et al. (2012). IIoh et al. (2011) found a difference of 10% (n= 39) more Nigerian females obese compared to males who lived in Imo state [18]. According to Etukumana et al. (2012), traditional Nigerian dishes were prepared with a variety of meat (e.g., beef and goat meat) as Nigerian adults enjoyed the tenderness of meat flavour. Those dishes contained high amounts of saturated fats and low- density lipoprotein (LDL) cholesterol and thereby increased fat deposits in the body system. This resulted for Nigerian adults to become obese and at higher risk of experiencing chronic diseases like CVD and stroke (Etukumana et al., 2012). However, Ikunjenlola (2020) argued not all Nigerian adults were able to afford buying meat to include in their meals. There were other factors such as the eating patterns that contributed to the prevalence of obesity in Nigeria. Ikunjenlola (2020) explained Nigerian adults often consumed more than 2 large meals a day. They tended to overeat and consumed more calories than they burned daily (Ikunjenlola, 2020). However, Agha (2017) advocated Nigerian adults would have a better understanding of calorie consumption if they received nutritional advice. Nutritional advice increased the awareness and advantages of consuming a healthy diet, including portion size, in individuals. This promoted a healthy lifestyle behaviour and changed patterns of obesity, health and quality of life [32]. According to Pierce (2019), interventions such as selfbehaviour management, weight loss programmes and providing health professionals like nurses with nutrition programmes could also support tackling obesity in Nigeria. For example, nutrition programmes could further enhance nurse practitioners understanding about malnourishment. As such, nurse practitioners would be able to provide effective nutritional advice to obese Nigerian adults to control their weight and dietary behaviour [35]. Therefore, Huang et al. (2021) suggested without a suitable intervention, obesity will continue to be a public burden in Nigeria. The high number of patients with obesity and the severity (e.g., associated medical conditions) could further put pressure on nurses in Nigeria. For example, nursing workload may increase, which affects the nursing time required to deliver patients’ care. Nurses would be responsible to look after more patients as well. This could result in nurses feeling burnt-out, stressed and unable to clinically perform well. Also, a higher demand of nursing practitioners specialised in obesity may be required on the ward or in the community to meet the needs of the patients.
There were several limitations to consider in this study. The variety of measurement tools to investigate the prevalence of obesity was not used in all studies. Some studies only used the BMI whereas other studies also included additional measurements such as questionnaires and waist- hip ratio. The use of additional measurements would have supported a variety of results being obtained. More so, not all the studies mentioned the duration to monitor the prevalence of obesity. This could have provided information about the length of the experiment and a better understanding of how it was undertaken. However, overall, the studies included a high number of participants, which supported more findings to be obtained. Also, the findings of the studies provided useful information about obesity among Nigerian adults in different states, the cause and associated significant long- term health complications. The studies also provided information about potential interventions that could be used to tackle obesity in Nigeria.
In conclusion, socio- economic status, sedentary lifestyle and diet were factors that stimulated the high obesity rate in Nigeria. Low educational level, which reflects socio- economic status, appeared to be the most associated factor with obesity in Nigeria [26]. Most of the studies reviewed indicated obesity was higher in Nigerian females compared to males.
Several interventions implemented by the government may cause the obesity rate to decline. For example, raising the awareness of health consequences associated with obesity among the Nigerian population. More so, nurses in Nigeria could be provided with additional training to enhance their knowledge about obesity to stimulate Nigerians adapting to a healthier lifestyle. As such, this may reduce the burden on the public health and lower the mortality rate in Nigeria.
