Author(s): Gunasekaran S, Raju Subramaniam, Rajesh VT, Navamani Prabakar, Sivagurunathan P, Nandhini Kumaran, Vilvanathan, Gnanapandithan GM, Prashanth Sankar and Mahbub-E-Elahi K Chowdhury
Background: Prompt risk assessment and early intervention is essential to improve outcomes in children with anemia. Resource-poor settings mandate the use of tests that are inexpensive, noninvasive, reliable, and durable. This study aimed to utilize the Noninvasive Screening of Anemia (NISA) color shade card to present the real-world user experience of medical practitioners in using the tool among children aged 6- 60 months.
Methods: The NISA shade card was used to determine the presence or absence of anemia and grade the severity by comparing the natural color tint of palpebral conjunctiva with the shade card. A feedback questionnaire was used to assess the experience of using the tool. Descriptive statistics were analyzed using R software.
Results: Nine pediatricians participated in this user experience and observations from 173 children were included. The sensitivity and specificity of the NISA shade card for risk assessment of anemia were 80.83% (95% confidence interval [CI], 72.64%–87.44%) and 66.04% (95% CI, 51.73%–78.48%), respectively. The tool was rated from good to very good by the pediatricians for its utility as an anemia risk assessment shade card. It was agreed that caregivers could effectively use it with proper training.
Conclusion: The NISA shade card may serve as an additional screening aid to clinicians in their routine practice. The ease of use and simplicity of interpreting combined with other clinical clues could make it an effective risk assessment tool in identifying children at risk of anemia.
Anemia is a severe global public health problem affecting over half of preschool children and pregnant women in developing countries [1, 2]. In 2019, the global prevalence of anemia among children aged 6-59 months was 39.8% (95% confidence interval [CI], 36.0%-43.8%) [3]. In India, 67% of children aged 6-59 months were anemic (hemoglobin [Hb] levels were below 11.0 g/ dL), which was higher than the National Family Health Survey-4 estimate of 59%. Anemia is more prevalent among children younger than 35 months than among older children, with a peak prevalence observed among children aged 12-17 months [4]. During infancy and early childhood, the presence of anemia can lead to long-term adverse effects on physical and neurocognitive development [5]. Iron deficiency is the most common type of mononutrient deficiency seen in children from low- and middle- income countries. Many preschool children in these countries remain vulnerable to iron deficiency anemia [6, 7].
Prompt risk assessment and early intervention can improve outcomes in infants and children with anemia [5]. Point-of-care diagnostic tests for anemia enable the identification of the condition among patients presenting at healthcare facilities. However, the use of such tests in peripheral health units where resources are scarce as well as in individual homes may not be viable, especially in low- and middle-income countries [8]. Hence, such settings mandate the use of tests that are inexpensive, noninvasive, reliable, durable, and independent of a power source [9, 10]. Multiple such simple tests have been developed, but they still rely on the use of either standard reagents or equipment and are often difficult to use. The Hemoglobin Color Shade card (HCS) developed by the World Health Organization (WHO) does not require any reagents but needs either a finger prick or venipuncture to draw blood for color-matching. This may not be practical when the supply of instruments and sterilization are not reliable [11]. Moreover, a noninvasive method is likely to be better received by children. Kramer’s scale and transcutaneous bilirubinometry are two non- invasive tools used to diagnose neonatal jaundice. However, their utility is restricted to a screening method due to subjectivity in visual assessment [12].
Hence, researchers worldwide have attempted to develop screening shade cards for anemia that use hue guides to match the conjunctival pallor [8, 9,13]. Such shade cards are believed to reduce the subjectivity in the visual estimation of conjunctival pallor.
One such tool, the Non-Invasive Screening of Anemia (NISA) color shade card was developed based on the user experience by Chowdhury et al. as a 13 ordinal shade guide with each shade denoting a code ranging from nonanemic to severe anemia. Hence, the objectives of the present study were to evaluate the real-world experience of medical practitioners in using the NISA shade card as a risk assessment tool among children between 6months to 60 months of age and to further provide recommendations to potentially improve its usability in the Indian setting.
The present user experience was conducted in Tamil Nadu, India, between February 2022 and April 2022. The NISA color shade card was compared with the routine laboratory Hb estimation, and its real-world user experience was recorded.
The NISA color shade card consists of a color spectrum that is matched with the natural color tint of the palpebral conjunctiva of children with different Hb levels. The color shade card has been developed based on the criteria provided by Chowdhury et al., who suggested the inclusion of 13 ordinal shades of pink, ranging from nearly paper white appearance to deep pink. These were coded 1 to 13 respectively. The shades were developed by mixing specific proportions of color on Microsoft PowerPoint 97 and printed at a resolution of 1440 × 720 dpi [9] (Figured as Figure 1).
The screening was done by comparing the conjunctival pallor with the NISA color shade card. The lower eyelid was everted, and the color of the palpebral conjunctiva was matched with the closest available shade on the card. A corresponding code and its interpretation were noted. Codes ranged from 1 (paper white color) denoting severe anemia to 13 (deep pink) denoting non-anemia.
The reference for the NISA shade card was Hb levels estimated by using an automated blood analyzer (Gold standard test).
A total of nine pediatricians working in private clinical settings across Tamil Nadu, India, participated in the user experience study between February 2022 and April 2022. A brief demonstration of the correct method of use of the NISA shade card was provided. Pediatricians were provided with NISA cards for use.
Before clinical history taking and physical examination, the practitioners were asked to use the NISA shade card and determine the presence or absence of anemia and grade the severity where relevant. Anonymized information from only those patients presenting with various anemia etiologies and scheduled to have their Hb levels measured via a complete blood count as part of their routine clinical care were considered.
The WHO criteria for grading anemia were used. Children under the age of 5 years were classified as anemic when their Hb levels were below 11 g/dL [14]. Severe anemia was defined as Hb levels below 7.0 g/dL, moderate anemia as Hb levels 7.0-9.9 g/dL, and mild anemia as Hb levels 10.0-10.9 g/dL [15].
At the end of 2 months, the doctors were revisited, and their user experience was recorded using a semi-structured, validated, 06-item questionnaire (Annexure 1). The questionnaire recorded the convenience of use, the feasibility of this shade card when used by caregivers, challenges in using the NISA shade card, and recommendations.
Statistical analysis was done using R software version 4.2.1. Criterion validity in terms of, sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood value, negative likelihood value, and accuracy was calculated with standard formulas using the confusion matrix. The Hb level estimated using an automated blood analyzer was considered the gold standard. Different components of the confusion matrix were defined as:
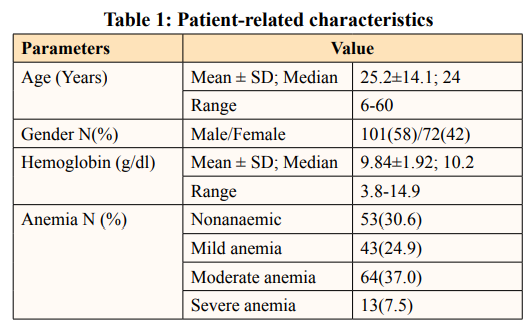
Nine pediatricians participated in this user experience. Information from a total of 173 children was included. The average age was 25.2±14.1 months (6 months-60 months). Among the included 173 children, 101 (58%) were males and 73 (42%) were females. The mean Hb concentration was 9.84 g/dL. Hb estimation with laboratory investigation indicated that 7.5% of the children presented with severe anemia, 24.9% had mild anemia, and 37% had moderate anemia. Around 30.6% of the user experience population was found to be nonanemic (Table 1).
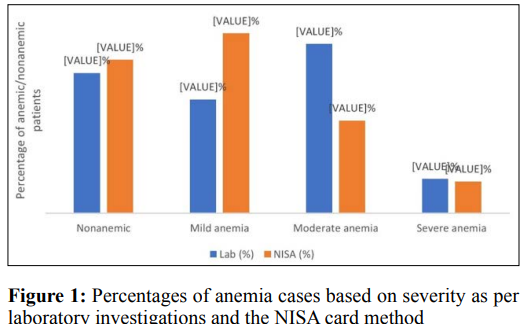
A risk assessment by the NISA color shade card revealed that the percentage of cases presenting with severe anemia was lowest (6.9%), followed by moderate anemia (20.3%) and mild anemia (39.3%). Approximately 33% of the population was found to be nonanemic.
Laboratory tests in the user experience population revealed that the percentage of non-anemia, mild, moderate, and severe anemia was 30.6%, 24.9%, 37%, and 7.5%, respectively. On the other hand, the percentage of nonanemic cases was a little higher in subjects evaluated with the NISA shade card, that is, 33.5%. The percentage of anemia cases classified as mild and moderate were 39.3% and 20.3%, respectively. However, the percentage of cases classified as severe anemia by the NISA shade card was only 6.9% (Figure 1) Around 3% of the cases were wrongly diagnosed as non-anemic by the NISA shade card. However, while distinguishing the cases based on severity, there was a difference of 15% in mild cases and around 17% in moderate cases compared to the gold standard test values. The NISA shade card diagnosed cases in concordance with the gold standard test for severe cases.


The positive predictive value was 82.85% (95% CI, 76.67%- 87.66%), suggesting that participants with a positive test truly have anemia and false-positive outcomes are minimal. The negative predictive value was 62.92% (95% CI, 52.84%-71.99%), suggesting participants with negative tests do not have anemia. The true positive rate was 84.37%.
The accuracy of the test was 75.95% (95% CI, 68.88%-82.11%), indicating the ability of this test to fairly detect a condition when it is present.
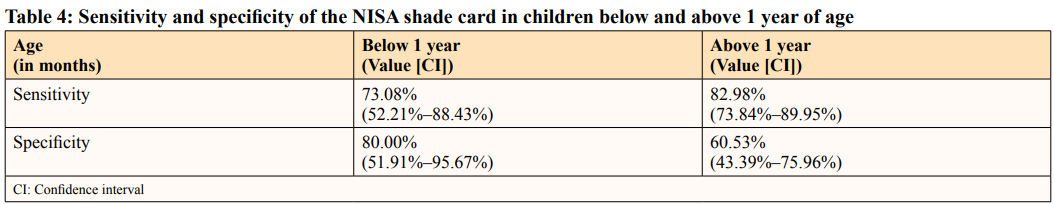
Table 4 indicated that below 12 months of age, the sensitivity was lower than the overall sensitivity, whereas it had a higher specificity. Above 12 months of age, the sensitivity improved, whereas the specificity decreased.
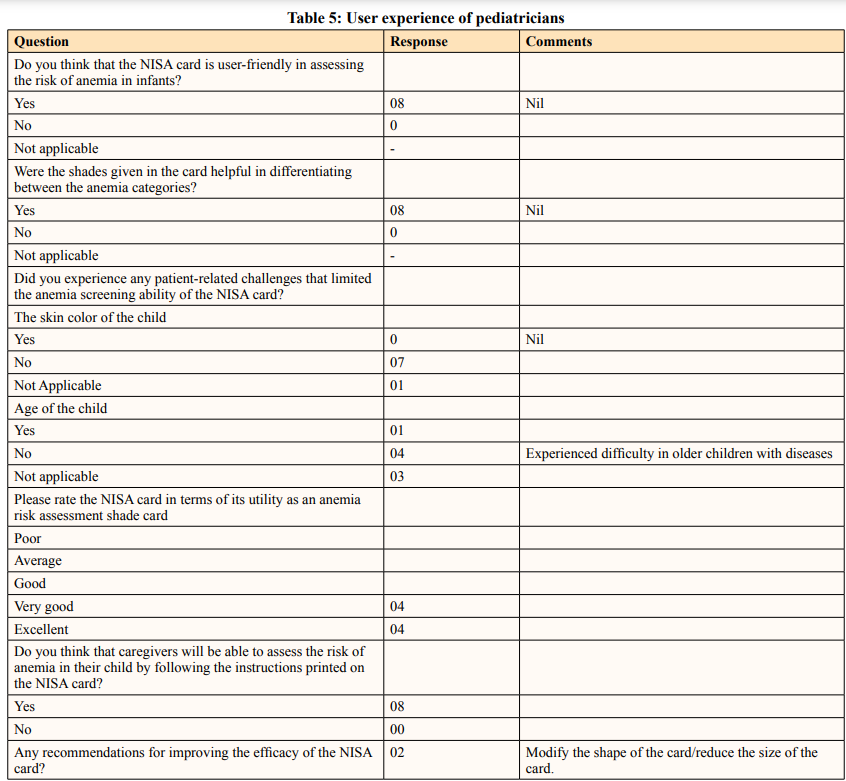
Eight of nine pediatricians participated in the feedback survey. All the pediatricians agreed that the NISA shade card was user-friendly in assessing the risk of anemia among children. They also reported that shades given in the card helped differentiate between anemia categories.
One of eight pediatricians opined that the older age of the child, especially those with illnesses, may limit the use of NISA cards. All the pediatricians rated the NISA card from “very good” to “good” and agreed that caregivers will be able to screen their child for anemia following the instructions printed on the NISA card. Among recommendations for improving the efficacy of the NISA card, the pediatricians suggested that the shape of the card could be modified for ease of use. Another suggestion was to add additional parameters to assess palmar pallor. Table 5 presents the user experience of the included pediatricians.
The results of this user experience indicate that the NISA card had a sensitivity of nearly 80% and a specificity of 66% in identifying children at risk of anemia. The overall user experience of the NISA card ranged from “good” to “very good,” and most doctors felt that the card can be used by caregivers to screen for anemia. It is reported that in children aged 28 days to 5 years, 1.8 million deaths may be avoided each year if their Hb levels are raised by 1 g/dL [14]. Timely detection of these cases is important to initiate early intervention. Accurate diagnostic tests can confirm the diagnosis of anemia; however, in resource-poor settings, these may not be viable as they require constant quality control by staff, the use of reagents, and consumables. To overcome this, the WHO introduced the HCS. Under ideal settings, this shade card was found to improve the diagnosis of anemia with a sensitivity of 85%-99%. Nevertheless, the diagnostic accuracy was found to be lower when the same shade card was studied under real-world conditions (sensitivity, 76%-88%). Moreover, the test is invasive, reducing its utility among the child population. Considering the variation in the diagnostic accuracy of the test when deployed in ideal and real-world settings, it was decided to investigate the user experience and diagnostic accuracy of the NISA shade card in the real-world setting [16].
Several studies have reported the use of a color shade card against pallor in the estimation of anemia [8, 9, 13]. Chowdhury et al. developed a color shade card to assist in the clinical assessment of anemia by measuring conjunctival pallor. They found that using the color shade card in assessing conjunctival pallor added an objective element to the screening of anemia. When used to detect pallor at multiple anatomic sites along with a detailed medical history of physical symptoms, it further helped to improve both sensitivity and specificity of the assessment. The color shade card was also found to be useful in raising the interobserver agreement (Chowdhury, 2002). Kalicki et al. investigated the usefulness of “HemoHue HH1”—a calibrated hue shade card for the noninvasive assessment of anemia by matching the pallor of the conjunctiva with the visual shade card. They reported discrepancies between the estimated and the measured Hb level and attributed this to varying degrees of degenerative ocular condition and vascular dysfunction seen in their user experience population who were principally aged and were on chronic hemodialysis [13]. Ugashoro et al. evaluated the ability of parents to recognize pallor using a simple Home-Based Anemia (HB-Anae) screening shade card. They reported that when parents, after brief training, used the home-based screening shade card, they could identify pallor better. Hence, among parents, the ability to detect pallor while using the shade card matched positively with the clinical detection of pallor by healthcare workers [8].
In the present user experience, the NISA color card was used to compare the conjunctival pallor with the shade guide and detect anemia in children. The results suggested that the NISA shade card was able to detect anemia with around 80% sensitivity and 76% accuracy, suggesting that the shade card can reasonably identify true-positive cases of anemia.
Clinical examination of anatomic sites where the capillary bed is visible through the skin or mucous membranes is a viable option for the detection of pallor [10]. Conjunctival pallor alone or in combination with palmar pallor may be used to predict severe anemia with high precision [17]. Trained healthcare workers can readily identify pallor, and physicians often utilize clinical assessment of pallor as a screening test and ask for a Hb test if any of the sites indicate the presence of pallor. This is a common practice in low-resource settings or crowded departments of public hospitals [18]. Severe anemia may be identified by visual inspection for the presence of significant skin pallor, pale nail beds, and palms. The conjunctiva provides a more sensitive and accurate estimation independent of skin pigmentation. However, this is mostly observer-dependent because the intensity of the conjunctiva color is not often matched with a reference hue [13]. In the present user experience, pallor in the palpebral conjunctiva was compared with the NISA color shade card. While most pediatricians were comfortable with the use of the card against conjunctival pallor, one practitioner suggested the incorporation of palmar pallor for improved detection. Stoltzfus et al. suggested that although imperfect, the use of pallor to screen for anemia is still a plausible test in areas of severe anemia. Furthermore, the authors ascertained that the sensitivity of examination can be improved by increasing the number of sites assessed for pallor, for example, palmar and conjunctival, which may be easily achievable [19].
The overall sensitivity of the NISA shade card was around 80%. On the one hand, laboratory tests in the user experience population revealed that the percentage of non-anemia, mild, moderate, and severe anemia was 30.6%, 24.9%, 37%, and 7.5%, respectively. On the other hand, the NISA shade card detected 33.5%, 39.3%, 20.2%, and 6.9% of cases with non-anemia, mild, moderate, and severe anemia, respectively. The difference in percentages of mild, moderate, and severe cases may be attributed to possible variations in the classification of positive anemia cases when using the NISA shade card. The color shade card developed by Chaudhary et al. when used along with clinical assessment offered a sensitivity and specificity of 83% and 91%, respectively [9]. The sensitivity and specificity of the HemoHue HH1 test were 50% and 73%, respectively [13]. Ughasoro et al. reported that the sensitivity and specificity of the home-based Anemia (HB-Anae) screening shade card used by parents when compared to the detection of anemia by healthcare workers were 77% and 84.7%, respectively [8].
Importantly, the sensitivity of clinical assessment of conjunctival pallor in diagnosing anemia was found to be 47.6%, whereas the sensitivity of the NISA card was substantially higher (80%) in this user experience [6].
With this card, the accurate assessment of the severity of anemia may not be as critical as the assessment of the presence of anemia itself. Here, over-screening cases as mild may be acceptable (24.9% of mild cases detected by laboratory test vs. 39.3% detected by NISA card) as the final decision of treatment still lies with the healthcare practitioner. Systematic reviews have substantiated our findings by concluding that most color shade cards are reasonably accurate in diagnosing mild and moderate anemia, particularly in circumstances where there is no access to a laboratory [2, 15].
It was found that the sensitivity of the test improved in children aged above 12 months. The National Family Health Survey of India-5 suggested that the peak prevalence of anemia is observed in 12-17 months. However, the improvement in sensitivity may be attributed to the child’s cooperation during physical examination.
The present user experience was performed in real-world settings to explore the user experience of the color shade card. While instructions for use were shared with the doctors, no attempt was made to standardize lighting to keep it as a real-world experience. It was insisted that the NISA card be used before any history taking or examinations were performed, to eliminate a potential source of bias like spectrum, review, and double gold-standard bias. There could be other reasons for the pallor of the conjunctiva like trauma, sepsis, viral suppression of bone marrow, lead poisoning, and metabolic-inherited or acquired diseases. These conditions limit the use of the NISA shade card. The healthcare practitioners were appraised and educated regarding the same. Another limitation could be the small sample size which may not give an adequate representation of the reference population. Sub-group analysis for age and severity of anemia was not performed. The user experience was assessed among pediatricians with the help of a 06-item questionnaire. Suggestions for change in the design of the card for greater dexterity and incorporation of palmar pallor were received. We believe this will enable future researchers to modify and assess the feasibility of this shade card in caregivers.
The NISA card serves as an additional aid to clinicians as an assessment tool in identifying children at risk of anemia in routine practice. The ease of use and simplicity in interpreting could make it an ideal screening shade for primary healthcare providers, in low-resource settings. It is, however, reiterated that it does not substitute clinical laboratory investigations, which remain the basis for the diagnosis and treatment of anemia. The screening validity of the NISA shade card can be validated by further studies with greater sample sizes and robust study designs in different populations. Sub-group analysis based on the severity of anemia and the age of children can provide more insight into the applicability of the tool.
Funding: The authors did not receive support from any organization for the submitted work.
Ethical Consideration: This retrospective study conducted in accordance with the Declaration of Helsinki and written informed consent was obtained from all participants before any study related activities.
Acknowledgement: All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval for the version to be published.
1.Public Health at a Glance (2003) Anemia. http://web.worldbank.org/archive/website01213/WEB/0 CO-50.HTM.
2.Critchley J, Bates I (2005) Haemoglobin colour shade card for anaemia diagnosis where there is no laboratory: A systematic review. Int J Epidemiol 34: 1425-1434.
3.WHO (2022) Anemia. Geneva: World Health Organization; 2022. Available at: https://www.who.int/data/nutrition/nlis/ info/anaemia.
4.International Institute for Population Sciences (IIPF) and ICF (2021) National Family Health Survey (NFHS-5) 1: 2019-2021
5.Jullien S (2021) Screening of iron deficiency anaemia in early childhood. BMC Pediatr 21: 337.
6.Chalco JP, Huicho L, Alamo C, Carreazo NY, Bada CA (2005) Accuracy of clinical pallor in the diagnosis of anemia in children: A meta-analysis. BMC Pediatr 5: 46.
7.Baker RD, Greer FR (2010) Committee on Nutrition American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age) Pediatrics 126: 1040-1050.
8.Ughasoro MD, Madu AJ, Kela-Eke IC, Akubuilo U (2019) Parental perception of childhood anemia and efficiency of instrument assisted pallor detection among mothers in Southeast Nigeria: A field validation user experience. Int J Pediatr 2019: 7242607.
9.Chowdhury ME, Chongsuvivatwong V, Geater AF, Akhter HH, Winn T (2002) Taking a medical history and using a color shade card during clinical examination of pallor improves detection of anemia. Trop Med Int Health 7: 133-139.
10.Montresor A, Albonico M, Khalfan N, Stoltzfus RJ, Tielsch JM, et al. (2000) Field trial of a haemoglobin color shade card: An effective shade card to detect anemia in preschool children. Trop Med Int Health 5: 129-133.
11.Stott GJ, Lewis SM (1995) A simple and reliable method for estimating hemoglobin. Bull World Health Organ 73: 369-373.
12.Varughese PM (2019) Kramer’s scale or transcutaneous bilirubinometry: the ideal choice of a pediatrician? can we trust our eyes?. Int J Contemp Pediatrics 6: 1794-1801.
13.Kalicki RM, Farese S, Uehlinger DE (2013) The validation of a new visual anaemia evaluation shade card HemoHue HH1 in patients with end-stage renal disease. Anemia 2013: 424076.
14.Scott SP, Chen-Edinboro LP, Caulfield LE, Murray-Kolb LE (2014) The impact of anemia on child mortality: An updated review. Nutrients 6: 5915-5932.
15.Onyeneho NG, Ozumba BC, Subramanian SV (2019) Determinants of Childhood Anemia in India. Sci Rep 9: 16540.
16.Marn H, Critchley JA (2016) Accuracy of the WHO Haemoglobin Colour Shade card for the diagnosis of anaemia in primary health care settings in low-income countries: A systematic review and meta-analysis. Lancet Glob Health 4: e251-e265.
17.Weber MW, Kellingray SD, Palmer A, Jaffar S, Mulholland EK, et al. (1997) Pallor as a clinical sign of severe anemia in children: An investigation in the Gambia. Bull World Health Organ 75: 113-118.
18.Kalantri A, Karambelkar M, Joshi R, Kalantri S, Jajoo U (2010) Accuracy and reliability of pallor for detecting anaemia: A hospital-based diagnostic accuracy user experience. PLoS One 5: e8545. Stoltzfus RJ, Edward-Raj A, Dreyfuss ML (1999) Clinical pallor is useful to detect severe anemia in populations where anemia is prevalent and severe. J Nutr 129: 1675-1681.
View PDF