Author(s): Sam Wakim*, Rina Ramirez, Stephen Abel, Sarah Walker, Howard Lavigne and Laura O’Shea
Introduction: Patients living with HIV/AIDS (PLWHA) have more unmet oral health care needs than the general population, outpacing unmet medical needs [1]. Poor oral health can impact a person’s confidence and ability to speak, eat, work, sleep, and socialize [2]. Lack of access to dental care is a national issue for HIV patients; providing access is a challenge faced by many health centers and practices, including Zufall Health in New Jersey, a federally qualified health center (FQHC). In collaboration with Northeast/Caribbean AIDS Education and Training Center (NECA AETC), Zufall embarked on an initiative to improve access to quality dental care for PLWHA. AETC is the training component of the Ryan White Program, a federally funded program that provides medical care, support services, and medications for PLWHA who are low income, uninsured, or underserved [3-5].
Materials and Methods: In 2019, Zufall Health launched a quality improvement project to increase oral health access and services for Ryan White patients by integrating all partners involved in providing health care: medical, dental, psychological, behavioral, and HIV/AIDS providers and case managers. The project goal was to increase the number of patients receiving dental care to improve oral and overall health.
Results/Observations: As a result of the project, there were significant quantitative and qualitative improvements in the oral health and quality of life of PLWHA: more dental encounters, a higher percentage of patients with a dental home, and the surpassing of the project goal of a 10% increase in dental referrals.
People living with HIV/AIDS (PLWHA) have more unmet oral health care needs than the general population, outpacing unmet medical needs. This health disparity particularly affects African Americans, the uninsured, Medicaid recipients, and those living within 100% of federal poverty limits [1]. Untreated oral disease not only impacts a person’s ability to eat, sleep, work, learn, and socialize, but also may be associated with infections, diabetes, weight loss, and malnutrition [2]. These health outcomes can be serious in HIV patients [6]. Lack of oral health care also affects quality of life, diminishing confidence and self-esteem, and limiting career opportunities [2]. While oral lesions and conditions are indicators of certain diseases, the evaluation of the oral cavity by providers is often neglected, especially when providers are faced with the management of chronic, complex conditions such as HIV/AIDS. This is compounded by the stigma patients may feel, when adding one more problem to a long list of check-ups [3].
Since 2010, Zufall Health, a federally qualified health center (FQHC), has been meeting the medical needs of HIV/AIDS patients through the Ryan White Program, a federal initiative that provides comprehensive primary medical care, essential support services, and medications for low-income people living with HIV [5]. Established in 1990, Zufall serves patients in northwest and central New Jersey. In 2019, the center supported over 40,000 patients with more than 143,000 visits across six suburban/urban counties and nine sites, including seven dental offices and two mobile medical/dental units. Zufall serves low-income, medically underserved populations, with a special focus on homeless individuals, public housing residents, and farm workers: 87% of patients are below 250% of the federal poverty level, 52% of patients are uninsured, 70% of patients identify as Hispanic, and 56% of patients are best served in a language other than English.
In 2018, Zufall served a total of 184 PLWHA. Fifty-five percent of newly diagnosed patients at Zufall were Hispanic/Latino; 86% of the newly diagnosed MSM patients (men who have sex with men) were Hispanic/Latino. Zufall’s Ryan White patient group was 72% male and 26% female. The racial breakout was 65% White, 27% Black American, 3% Asian American, and 5% Unreported; of the total group, 40% were reported as Hispanic. The age distribution consisted of 10% of patients in their 20s, 21% in their 30s, 22% in their 40s, 27% in their 50s, 17% in their 60s, and 3% above age 70. Forty-six percent of the group were at or below the federal poverty level.
To address the unmet need of access to dental care, Zufall collaborated with the Northeast/ Caribbean AIDS Education and Training Center (NECA AETC) on a quality improvement project to increase the number of PLWHA receiving an annual oral exam by a dentist during the project measurement year of 2018-2019. Due to COVID-19, different strategies were created for 2020; patient outcomes will be examined in the future. An established training partner, NECA AETC is part of a national network of eight regional and two national AETCs. It works with individual health care providers, teams, and clinical sites in New Jersey, New York, Puerto Rico, and the US Virgin Islands to provide education and training programs, as well as capacity-building assistance to improve clinical care along the HIV care continuum [4].
Since implementing the Ryan White Program in 2010, Zufall has successfully integrated the medical treatment of PLWHA in the arenas of nutrition, pharmacy, case management, and behavioral health. Expanding the integration of resources to increase access to oral health services was a logical next step. In 2018, 38% of HIV patients were seeing a Zufall dentist, 16% were seeing an outside dentist, and 46% did not have a dentist. Goals of the project in collaboration with NECA AETC included: 1) increasing by 10% the total number of Ryan White patients having an annual oral exam and 2) improving the HIV/AIDS Bureau (HAB) health performance measures in four key areas: Dental and Medical History, Dental Treatment Plan, Oral Health Education, and Periodontal Screening or Examination.
The project collaboration to increase Ryan White patient visits to a dental provider and to improve the HAB health performance measures began in 2018. There were four steps in the Zufall/NECA AETC collaborative process: 1) needs assessment and buy-in; 2) monthly phone calls with the site team and completion of pre-work for on-site training of the integrated team; 3) implementation (oral health assessments by the medical team followed by referrals to dentists, as needed); and 4) follow-up calls and surveys. AETC resources enabled decision-support training for medical, dental, and case management staff, facilitated process changes, and supported the integrated team in devising solutions to barriers to care, such as making changes in scheduling for enhanced access and improving systems of care.
Interaction and dialogue were lynchpins of process change. Regular calls, feedback, and meetings throughout the project to discuss challenges and issues resulted in additional, evolving education sessions and support. Zufall relied on NECA AETC’s experience and resources to address concerns, such as patients arriving without the proper medical clearances and chart documentation.
NECA AETC ensured a smooth process improvement by clarifying implementation and assessment of the four HAB Measures. All efforts were supported with resources, such as patient brochures on the importance of oral health, posters, videos, and assessment cards for clinicians with tips on how to approach patients, ask questions, and document results of interactions.
The strategy of cross-training all staff on oral health resulted in an integrated approach and was especially invaluable in Zufall locations without an on-site dental team. Regular team meetings reinforced the holistic, combined dental/medical approach to HIV management. Ongoing training and check-ins fostered crossdisciplinary efforts to meet the goal to increase access to and improve oral health.
The collaboration also included regular reviews of data and outcomes, resulting in refinements, as needed. NECA AETC helped Zufall close the loop, working with the core team to incorporate successful process changes into the center’s policies and procedures.
To integrate oral health care into its overall health care program and improve HIV patient outcomes, Zufall used the Care Model and the Model for Improvement, including the PDSA method (Plan Do Study Act). The Care Model included interventions in training staff, changing processes and workflow (scheduling, etc.), ensuring leadership support, empowering teams, engaging patients, addressing trauma and stigma, and collecting data.
Training to promote staff integration was a principal driver in the quality improvement process. The integration effort had several components: conducting a needs assessment, encouraging buyin, planning, training, implementation, evaluation, and course correction, as needed. The training and technical assistance to help facilitate integration varied per discipline (medical, dental, case management), and included topics such as mental health, adolescent needs, substance use, crisis intervention, motivational interviewing (MI), identification of oral lesions, and integration of oral health into primary care. The overarching goal of ongoing training was to improve skills, facilitate communication, enhance patient navigation, and improve overall patient health.
Coordinated treatment is vital in PLWHA, especially for riskbased preventive services and medical clearance requirements. Training HIV case managers on oral health emerged as a critical step in the integration process. Case managers have frontline access to patients: providing frequent communications, scheduling appointments, and being their most trusted partner in care. It was vital they were comfortable with oral health and primary care messaging. An equally important reason for including case managers was to ensure patient safety and continuity of care: reconciling medications, providing prompt health status updates, and ensuring effective sharing of information. Building good relationships with the case managers, inviting their support, and training them in oral health would be critical to Zufall’s project success. Case managers were instructed on the importance of oral health and how to appropriately review a dental risk assessment tool.
NECA AETC used role-playing and provided techniques on how to successfully incorporate oral health education into case managers’ interactions with patients.
Medical staff received didactic and hands-on education on headand-neck exams and oral lesions. NECA AETC provided helpful tools and guidance. The oral health assessment process for primary care providers included four steps: Ask, Look, Act, Document. “Ask” includes asking patients if they had a dentist, had noted any oral health changes, and how often they were brushing. “Look” is looking in the patient’s mouth and performing the head, neck, and intra-oral examination. “Act” is to give treatment or refer to a dentist, as needed. “Document” is to write down findings regarding the examination, treatment, referral, and follow-up into the patient’s medical record via a newly updated dashboard. After the didactic presentations, staff broke into groups for the hands-on training. A staff dentist was assigned to each site to support the medical staff training on how to perform head-and-neck exams. With dental team support, medical staff learned how to probe the mouth more thoroughly and assess whether they could treat the patient themselves or should refer to dental staff. Motivational interviewing training (MI) enhanced patient-clinician interactions by fostering trust and partnership. A simple yet effective tool in the hands-on training was the addition of head lamps for the medical providers to facilitate examinations with both hands available.
The NECA AETC needs assessment of the dental team revealed ongoing training needs in the following areas: dental management of the medically-complex patient, substance use and oral health, management and identification of oral lesions, and the seamless integration of oral health into primary care. Other topics included mental health, stigma, cultural competency, behavioral health, motivational interviewing, adolescent needs, and crisis intervention.
Communication was fundamental between interdisciplinary team members, as well as through the EMR (electronic medical record). Using a shared EMR, dental and HIV case managers and providers are able to easily communicate findings, referrals, and notes. Because effective referral communications were an established part of the Zufall culture, the center could seamlessly and quickly get patients into care, either at the site where the patient was receiving medical care or at another Zufall location if the site did not provide dental services.
Patient workflow solutions included improved processing of new patients, prompt medical clearances, designated scheduling blocks reserved for PLWHA, warm hand-offs, pre-appointment planning, and enhanced follow-up. These process changes would facilitate increased access to dental care, and improved patient engagement with dental clinicians.
Zufall’s new workflow began with a cross-disciplinary team review of the patient’s needs. During the patient’s visit, the dentist joined the infectious disease doctor, pharmacist, nutritionist, behavioral health specialist, and HIV/AIDS case managers to screen for health issues, including oral health. The integrated team conducted a risk assessment, established self-care goals, and scheduled the patient for a dental appointment in a pre-designated follow-up schedule block at the Dover dental site. This new process addressed issues such as missing clearance or laboratory results prior to the dental appointment, which previously had necessitated rescheduling the visit, exacerbating feelings of being stigmatized. The expanded team, including dental residents, reviewed the patient’s chart, laboratory results, and medical clearance with the infectious disease doctor prior to the dental appointment.
Once this process was in place, the integrated team expanded the review of the medical records of all patients with upcoming visits during the month. The team prepared a report on each patient for the dental staffs; medical clearances were obtained from the infectious disease providers and documented in the EMR; and the integrated team discussed lab results. These additional preplanning steps streamlined the process and optimized seamless patient care upon arrival to the dental clinic.
An important change to the Zufall process was to ensure appointments were available for Ryan White patients soon after the initial screening to capitalize on patient/provider engagement and reinforce the importance of a timely dental exam. Due to extended waits for dental appointments, the team created scheduling blocks for PLWHA. After implementation of block scheduling, patients continued to exhibit a high no-show rate for their appointments, necessitating a new process cycle. A warm hand-off was created: the case managers and medical providers introduced the dentists to Ryan White patients when patients were at their medical visits. The warm hand-off, combined with a readily available follow-up appointment, was intended to ensure patients kept their appointments while still engaged and interested.
Along with the medical and dental process improvements, patient engagement enhancements were implemented. These enhancements included demystifying the oral health process and assuaging fear of dental visits. Partnering with patients’ HIV/AIDS case managers and positioning them as the liaison between the two disciplines (medical and dental) facilitated those enhancements, along with patient engagement training and process improvements in the areas of cultural competency, substance use disorder, health literacy, self care/home care, motivational interviewing, traumainformed care, mental health disorders, guest experience, service recovery, warm hand-off, and ongoing follow-up
Patient satisfaction surveys drove process change in both the delivery of services and organizational culture: enhancing services and assessing providers’ interpersonal skills. The surveys asked patients how clearly the provider explained medical conditions; whether or not the provider treated the patient as an active partner in decision-making and goal setting; if the provider used understandable language; how well the provider answered questions; if the provider empowered the patient with self-care tips; and whether or not the patient would recommend the provider and practice to others. Zufall utilized Luma Health, a third-party, multimedia education software system, to engage patients and conduct patient surveys. The center deployed Luma’s simple, intuitive patient engagement and survey software. The software streamlines the collection of comments and ratings from patients digitally, and then quickly and seamlessly shares real-time feedback with the care team [7]. The goal was to use the invaluable, in-themoment patient insights to drive process change, exceed patient expectations, and enhance satisfaction with services.
The EMR used by Zufall captures information critical to the care of PLWHA and is the principal tool used for tracking progress towards the project goals. The EMR integrates both medical and dental patient information in one system. The project data capture and reporting improvements included broadening the capacity of a custom-designed dashboard and uploading information from structured data fields, generating reports, validating data, and reviewing charts. Oral health metrics critical to the continuum of care, as well as the measurement of access, included the number of dental visits, patient risk assessments (low, medium, or high), tracking of patients’ self-management goals and education, patient engagement and satisfaction, and general dental health diagnoses and treatments (incidence of caries, treatment, and recall/followup).
Zufall also instituted a chart review of every Ryan White patient who presented at dental appointments to track HAB measures in four key areas. Every HAB measure quantifies the number of oral health clients who received a clinical oral evaluation during the measurement year. The HAB Measure Dental and Medical History uses data from a variety of sources to quantify the number of oral health clients who had a dental and medical health history started or updated at least once in the measurement year. The Dental Treatment Plan measure assesses the number of oral health clients who had a dental treatment plan developed and/or updated at least once in the measurement year, with a goal of measuring the rate of dental emergency visits. The HAB Measure Oral Health Education analyzes the number of oral health clients who received oral health education once in the measurement year, with a goal of determining the rate of dental disease/oral pathology and the rate of tobacco cessation. The Periodontal Screening or Examination measure evaluates the number of oral health clients who had a periodontal screen or examination at least once in the measurement year, with a goal of measuring the rate of tooth loss due to periodontal disease. Systematic, monthly reviews of the dashboard and charts were conducted and shared with the core team, NECA ATEC staff, the care team, and at Dental, Medical, and QA/PI Committee meetings. Tracking of data and outcomes allowed for process changes, celebration of successes, and identification of areas in need of improvement.
Zufall exceeded its project goals to improve the oral health of Ryan White patients and has established process changes as part of a patient-centered approach. In 2019, Zufall served 229 patients in 3088 encounters, and enrolled 52 new patients. Dental encounters for PLWHA increased steadily from 371 in 2017 to 408 in 2018, a 10% increase. In 2019, there were 502 dental encounters, a 23% increase from 2018. Services included checkups, cleanings, fillings, extractions, partials, dentures, crowns, bridges, and periodontal surgery
In 2018, 38.04% of HIV patients were seeing a Zufall dentist, 16% were seeing an outside dentist, and 46% did not have a dentist. Process changes improved those percentages in 2019, exceeding the process improvement project goal of increasing dental referrals by 10%: 48.91% were seeing a Zufall dentist (up approximately 11%), 15% were seeing an outside dentist (down 1%), and 36% reported having no dentist (down 10%). The increase in the number of patients seeing a Zufall dentist during the project year was statistically significant (p=0.0273; 2-sided). Additionally, the proportion of patients seeing any dentist was statistically significant, increasing from 53.80% in 2018 to 64.19% in 2019 (p=0.0327; 2-sided).
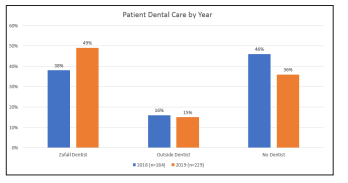
Chart 1: Percentage of Zufall HIV/AIDS patients receiving dental care during the process improvement period of 2018 and 2019 exceed the process improvement project goal.
Zufall goals on improving HAB measures were also met. For PLWHA using Zufall for dental care, at year-end 2019, 100% had a new or updated dental/medical history versus 96% in 2018; 100% had a dental treatment plan versus 93% in 2018; 71% received oral health education versus 40% in 2018; and 64% received periodontal screening or examination versus 49% in 2018.

Chart 2: Improvement in Zufall HAB (HIV/AIDS Bureau) Health Performance Measures during the process improvement period.
Patient surveys rating newly-integrated staff encounters and engagement were positive: in 2018, patient satisfaction was 98.2% with medical providers and 98.3% with dental providers; in 2019 it was 99% and 98.8%, respectively. Luma Health patient feedback scores for October 2019 through February 2020 were 97%. Patients also highly ranked providers’ interpersonal skills.

Chart 3: Patient engagement/encounter surveys show high satisfaction with medical providers.
Surveys of Zufall medical staff who received oral health training revealed 63% performed more detailed head and neck exams, 70% understood what to look for in an oral exam, 77% referred patients to a dentist or consulted with a dentist after noting a suspicious oral lesion or related complaint, and 83% expressed interest in additional cross-training on the head and neck exam. The dental team and case managers also reacted favorably to trainings. Case managers rated the course on the importance of oral health in primary care very highly and expressed high comfort levels with the material and their new role.
As a result of process improvements, PLWHA experienced increased access to dental visits and greater satisfaction with services by the end of the measurement period.
Staff Integration: Medical, Dental, and HIV Case Management The integration of medical, dental, and Ryan White case managers and other HIV/AIDS support staff was the cornerstone for the project. Zufall has a history of successfully integrating medical and dental staff in health care services, including blood pressure screening; nutrition education (diabetes and BMI); and oral cancer prevention, such as education on tobacco use, substance abuse, and HPV [8]. Integration enabled the teams to establish relationships with each other and with patients to enhance communications, address trauma and social stigma, overcome barriers, support the effective management of schedules and dental visits, and improve patient satisfaction. Building relationships with Ryan White case managers and involving them in the oral health project were critical to our success, due to their trusted relationship with the patient. As a result, when PLWHA were referred to us from outside agencies, we included the referring agency’s case managers in our process because of this relationship. Staff integration, with appropriate cross-training, increased the number of PLWHA utilizing dental services. Interdisciplinary training and teambased, patient-centered care by dental and medical providers are successful models and will be the norm in the near future. Our staff found meaning and job satisfaction from making a difference in the lives of patients. Unsolicited, positive testimonials from PLWHA about the impact of good oral health care on their quality-of-life inspired the staff.
Improving workflow processes (scheduling blocks, timely medical clearances, cross-disciplinary teamwork) resulted in transitioning more patients into care; therefore, optimizing health outcomes.
Engaging patients (communicating in a way that reduces stigma and making them feel welcome) minimized fear of dentists, facilitated getting patients into oral health care, and improved patients’ quality of life. Being able to meet patients where they are proved to be very important, since each patient is unique, as are their challenges. For example, counseling a patient about brushing more often became moot because substance abuse was affecting the patient’s overall health. The priority had to be shifted to a more emergent need.
No matter how good a program is the patient needs to be ready to enter into care. PLWHA often experience stigma because of their condition, and we found a large proportion experienced childhood adverse events and life trauma. Motivational Interviewing revealed that patient readiness was fundamental to starting and maintaining oral health treatment. When dealing with a complex patient facing an array of serious issues, both medical (in terms of viral load and medications) and social (in terms of living conditions and safety), it is unrealistic to expect patients to connect with all oral health prevention messages and recommendations in one visit. The timing of information exchanges was reassessed to better match the individual patient’s acceptance level. Motivational interviewing helped in determining when and how to convey information and suggest interventions to patients. It also led to a change in the sharing of guidance, in digestible bites, based on the patient’s readiness. The practice of gentle persistence when patient acceptance was low resulted in excellent patient satisfaction reviews.
Integrating all data into one EMR (to include both medical and dental patient information) improved our process, our training, how we used the data to measure access, and ultimately, oral health as well as systemic health for Ryan White patients.
While we have been serving Ryan White patients across all nine Zufall sites, the primary project teams were located in our Dover and Somerville locations. To increase the number of PLWHA receiving dental care, we plan to implement the program throughout the Zufall Health system, including those sites without an in-house dental clinic. We will also refine our data and dashboard to enhance the type of patient information we can access, improve our processes for scheduling and warm hand-offs, and continue to train the teams in MI skills, patient engagement, and goal-setting. The project QA best practices were implemented in 2019. Due to COVID-19, different strategies were created for 2020. The impact of those process changes on patient outcomes will be examined separately.
Melanie Raskin, Medical Writer
Sarah Christenbury, Graphics
