Author(s): Aravind Reddy Kuchkuntla
Necrotizing fasciitis (NF) is a serious, life-threatening subcutaneous soft tissue infection. NF can progress rapidly and evade detection as it may or may not be visible on the surface of the skin, which makes high level of suspicion crucial in early and rapid identification of high-risk patients to improve clinical outcomes [1]. Two types of NF are generally recognized, Type I which is a polymicrobial infection, and Type II which is a monomicrobial or polymicrobial associated with group A Streptococcus (GAS) infection [2]. NF involves the groin, abdomen and extremities more commonly, but it may involve the head and neck as well [3]. Predisposing factors include old age, immunocompromised status (such as diabetes and chronic illness, etc.) and malnutrition.
Between 2003 and 2013, the overall mortality rate for NF related death was 4.8 per 1,000,000 person-years. Streptococcal infection was the most common cause of NF where a pathogen was reported, but most cases do not have a microbiologic diagnosis [1].
A 24-year-old male with no significant past medical or surgical history, presented to the emergency department with complaints of right sided facial swelling and pain. Five days prior to presentation, he had 2 of his wisdom teeth extracted (#1 and #32). Surgery was uneventful and patient was discharged home with a prescription for pain killers and NSAIDs. He had a follow up appointment with the dental clinic 5 days after the surgery due to pain and swelling of the right face, worsening for 3 days. Upon evaluation, an attempt to drain a suspected abscess under local anesthesia was unsuccessful and no purulence was obtained (Figure 1). Patient was prescribed Augmentin empirically for 10 days.

Figure 1: Suspected post-op abscess
About 8 hours later, on the same day, patient was noted to be febrile, sweaty and ill-looking with a near syncopal episode which prompted a visit to the emergency department. On presentation, patient had significant right sided facial pain and swelling extending from the inferior border of right mandible to the right temple. Swelling was firmer with pitting edema at the mandibular angle and softer towards the temple without crepitus. Patient did not have any difficulty breathing or muffled voice, but he had trismus, dysphagia mostly to solids and his right eye was swollen shut (Figure 2).
Computed tomography (CT) scan of neck and soft tissue with contrast showed extensive right facial cellulitis with a small abscess and a 1.9 x 1.3 x 1.8 cm peri-mandibular collection of air throughout the soft tissue with subcutaneous air tracking superiorly to the right temporal soft tissues. Mild cervical lymphadenopathy of the submandibular and jugular chain regions was noted. No masses were identified and parotid, thyroid and submandibular glands were intact (Figures 2,3,4). These findings along with clinical presentation raised suspicion of necrotizing fasciitis.
Empiric antibiotic therapy was started with Clindamycin, Piperacillin-Tazobactam and Vancomycin, and patient was urgently evaluated by surgery then taken to the OR. No necrosis was appreciated but a boggy and edematous temporalis muscle with purulence lateral to right masseter muscle was identified. Intraoperative cultures were obtained, and multiple Penrose drains were placed.
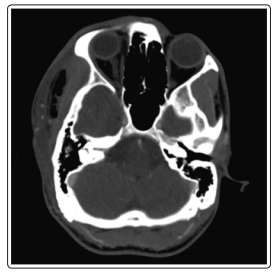
Figure 2: Subcutaneous air in the right temporal soft tissue
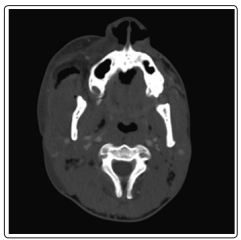
Figure 3: Subcutaneous air in the right maxillary soft tissue

Figure 4: Subcutaneous air in the right peri-mandibular soft tissue
clinical presentation raised suspicion of necrotizing fasciitis.
Empiric antibiotic therapy was started with Clindamycin, Piperacillin-Tazobactam and Vancomycin, and patient was urgently evaluated by surgery then taken to the OR. No necrosis was appreciated but a boggy and edematous temporalis muscle with purulence lateral to right masseter muscle was identified. Intraoperative cultures were obtained, and multiple Penrose drains were placed.
Three days after initial I&D, swelling slightly improved but patient continued to have fevers despite antibiotic therapy. An increasing amount of purulence was expressed from the hemicoronal incision. Patient was subsequently taken to the OR for a washout. During surgery, a necrotic right temporalis muscle (Figure 5), confirmed by intra-op frozen section (Figure 6).
The necrotic tissue was debrided, and the temporalis muscle was excised. Another set of cultures obtained during the procedure. Blood cultures showed no bacterial growth, but wound cultures grew Streptococcus Constellatus, K. Pneumoniae, S. Epidermidis, Parvimonas Micra and normal oral flora.
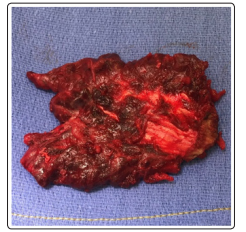
Figure 5: Necrotic right temporalis muscle
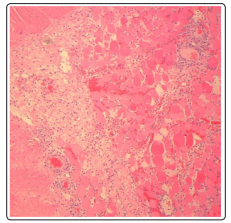
Figure 6: Frozen section of the excised right temporalis muscle
Six days after initial I&D, one of the drains from oral cavity to the neck had concerning smell and a part of the underlying muscle at the wound edge appeared to be edematous. CT Scan showed areas of right masseter pyomyositis, abscess and poorly drained areas of fluid collection. Patient was taken back to OR on day 7 for a further washout and debridement. The right masseter muscle was resected, pathology confirmed necrotizing fasciitis in this specimen as well. Cultures grew K. Pneumonia, S. Epidermidis, Veillonella Parvula, Peptostreptococcus sp.
Ten days after initial I&D, patient was taken to the OR for another washout and exam under anesthesia. He had a temporary tracheostomy placed due to difficult intubations and recurrent procedures. He had open wet-to-dry wound continued to be hospitalized, on intravenous antibiotics. He had repeated CT scans with close monitoring by oral and maxillofacial surgery and infectious disease teams.
Over the course of the following two weeks, patient had a smooth recovery, tracheostomy was down-sized then reversed. Patient was continued on oral antibiotics with outpatient follow ups. Patient started physical therapy with jaw-stretching prosthesis. Due to the deformity caused by the excision of the right temporalis muscle, he is scheduled to get an implant to fill the right temporal area.
Necrotizing fasciitis is a rare, complex and life-threatening infection of the skin and soft tissues. It commonly involves the groin, abdomen and extremities and to a lesser extinct the head and neck. Treatment involves prompt surgical intervention with extensive and aggressive debridement with the concomitant use of broad-spectrum empiric antibiotic therapy
Initial therapy should aim to cover polymicrobial infections as they account for about half of NF cases. Therapy should include coverage for Methicillin-resistant Staphylococcus aureus, MRSA (with vancomycin, linezolid, etc), coverage for gram-negative pathogens (with piperacillin-tazobactam, ampicillin-sulbactam, etc) and an agent with anerobic activity if the selected antibiotics lacks it (with metronidazole or clindamycin).
Surgery remains the mainstay of NF therapy with many studies suggesting that early and aggressive debridement is the most important intervention. Traditionally, surgical training dictates the removal of all necrotic tissue, but adequate debridement has not been defined [1]. Other adjunctive treatments include intravenous immunoglobulin IVIG and hyperbaric oxygen were found to be ineffective and not recommended [2].
In conclusion, Necrotizing Fasciitis (NF) is a medical emergency that can be challenging for both clinicians and surgeons. It requiresa quick recognition as it can be fatal if not early diagnosed and managed. As depicted in this case, the rapid progression of cervicofacial edema and swelling shortly after any dental or head and neck surgery or trauma should raise suspicion of a possible NF [4-6].
