Author(s): Aravind Reddy Kuchkuntla
Plasmacytomas are localized tumors of monoclonal plasma cells, typically affecting the axial skeleton and present as solitary bone lesions known as solitary bone plasmacytomas (SBP). Another type of plasmacytomas are extramedullary plasmacytomas (EP) that are localized plasma cell neoplasms affecting the soft tissues such as skin, brain lymph nodes etc. These tumors are account for 5-10% of all plasma cell disorders and among these tumors a rare entity is a multiple solitary plasmacytoma (MSP). MSPs are rare and account for only 5% of all SBPs. MSP presents with multiple SBPs with or without EPs with no bone marrow involvement as multiple myeloma. Literature is limited on MSP as it is a rare diagnosis. Here, we present a case of a 64-year-old male who presented with shoulder pain after a fall, found to have an SBP of the right shoulder, SBP of left femur and a left hypopharyngeal EP. The tumors were excised and he was treated with 6 cycles of bortezomib and dexamethasone. After chemotherapy and radiation patient showed good response and remained in remission on follow up.
Plasmacytomas are plasma cell tumors of monoclonal origin, commonly affecting elderly males and present as a single lesion (solitary plasmacytomas) or with multiple lesions [1]. Solitary plasmacytomas (SBP) comprise less than 5% to 10% of plasma cell neoplasms, seen predominantly in males with a median age of diagnosis around 55 years of age [2]. Multiple solitary plasmacytomas (MSP) are reported to be 5% of all the SBP cases.
The International myeloma working group classifies solitary plasmacytoma has biopsy-proven solitary lesion of the bone or soft tissue (extramedullary plasmacytomas) with clonal plasma cells, a normal skeletal survey, and absent systemic symptoms [3]. Multiple Myeloma (MM) on the other hand presents with systemic symptoms of hypercalcemia, renal insufficiency, anemia and multiple lytic bone lesions [4]. The most common presentation of SBP is a single painful lesion that usually occurs in the axial skeleton, such as the vertebra and skull. However, these lesions can be found incidentally in asymptomatic patient during roentgenographic studies for evaluation of other bone related complaints as well.
Extramedullary plasmacytomas (EP) are rarer than SBP comprising approximately 1-3% of all plasma cell neoplasms and are described as localized plasma cell neoplasms that arise in tissues, especially in the head and neck with the upper airway being most common. Plasmacytomas of bone can progress to multiple myeloma over a course of 2-4 years, however extra-medullary forms seldom progress to MM.1 The International Myeloma Working Group recognized a new classification of plasmacytomas in 2003 known as MSP with multiple lesions present in bone, soft tissue or both with no M protein in serum or urine and with normal bone marrow.5 There have been only a few cases with MSP published in the literature, We present one such case of MSP successfully treated with chemotherapy and surgical resection of the lesion.
A 64-year-old male with a history of a cerebrovascular accident (CVA) and recurrent falls presented to the hospital with worsening right shoulder pain. He had residual weakness in his right upper and lower extremity from his CVA and fell on his right shoulder prior to presentation. He complained of progressively worsening shoulder pain, especially with overhead movements. His past medical history is significant for right-sided hemiplegia after a stroke 10 years ago and gait instability. He smoked one cigar per day for the past 30 years, did not consume alcohol or use illicit drugs. Review of systems otherwise was negative. On physical examination patient had weakness in the right upper and lower extremities. No palpable mass was appreciated in the right shoulder region and there was restriction of range of movement due to residual weakness. Physical examination was otherwise unremarkable.
Erythrocyte sedimentation rate was 18 [ normal range 0 to 20 mm/h], alkaline phosphatase was 3.4 [ normal range: 6.5-20.1 UG/L], hemoglobin was 14.6 g/dl [ normal range: 13.0-17.0], serum calcium was 9.2 mg/dl [normal range: 8.6-10.3]. X-ray of the right shoulder revealed an expansile, cystic, and septate structure within the distal clavicle and acromioclavicular joint space (figure 1). Further evaluation by MRI demonstrated a large lobulated osseous lesion in the distal clavicle and within the superior-lateral scapula measuring with a size of around 5.7 x 2.7 x 2.7 cm (figure 2). There were areas of cortical thinning anddestruction with mild edema concerning for a possible malignancy. Therefore, the patient was scheduled for a biopsy of the shoulder lesion. Pan imaging of the chest, abdomen, and pelvis were negative for primary malignancies.
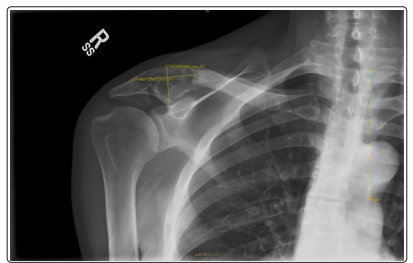
Figure 1: X-ray of the right shoulder showing a septate cystic mass in the distal clavicle and acromioclavicular joint space
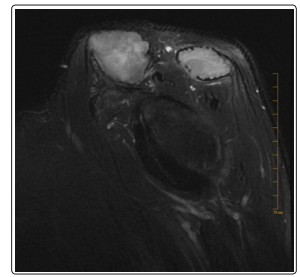
Figure 2: Cross sectional MRI view of the Right shoulder showing the large lobulated osseous lesion in the distal clavicle
During intubation before the procedure, an incidental left hypopharyngeal mass was noted. CT soft tissue neck showed a 2.2 x 4.1 x 4.2 cm mass, nearly effacing the airway (figure 3). The right shoulder biopsied tissue and the excised hypopharyngeal mass revealed to be monoclonal plasma cell neoplasms on histopathological examination. A whole-body PET scan demonstrated intensely metabolically active lytic lesions of the femoral neck, clavicle, and hypopharyngeal areas. Bilateral medial clavicular lesions along with a left anterior rib lesion were also observed.
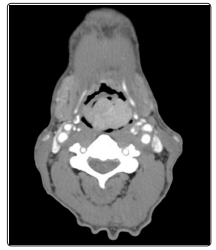
Figure 3: CT soft tissue showing a hypopharyngeal massDifferential diagnosis included multiple myeloma, waldenstrom macroglobulinemia and multiple solitary plasmacytoma and metastatic lesions of an unknown primary. Further work up showed elevated kappa light chain level of 493.5 [normal range 3.3-19.4 mg/L], lambda light chain level of 22.2 [normal range: 5.7-26.3 mg/L] with a Kappa to lambda [K/L] ratio of 22.23 (normal range: 0.26 -1.65 mg/L). Serum IgG was high at 1568 (Normal Range: 600 - 1,500 mg/dL) and serum electrophoresis showed an abnormal gamma region peak that can be occasionally seen in patients with SBP.
During follow up, the patient complained of left hip pain, and an x-ray of the lower extremity showed lytic lesions in the head of the femur. A CT of the lower extremity showed a lytic lesion concerning for malignancy with an associated pathological fracture (figure 4). The fracture was fixated laterally with a cephalomedullary nail and the lesion was treated with local radiotherapy

Figure 4: Ct scan of the left lower extremity showing lobulated lytic lesion in the intertrochanteric region of the left proximal femur
The patient underwent biopsy of the right shoulder mass and resection of the hypopharyngeal mass. He received radiation therapy (approximately 2000cGy of radiation to his right shoulder and left femur. Given the presence of extra-medullary plasmacytoma along with a solitary bone plasmacytoma, patient was treated with a regimen for multiple myeloma. Patient completed treatment with six cycles of bortezomib and dexamethasone with good response and eventually had normalization of immunoglobulins and light chains.
Post treatment PET scan showed resolution of all the lesions. The patient was followed up at six-month intervals. During follow up his kappa/lambda levels and IgG levels continued to drop, at one year of follow up his kappa light chain level was 13.5 (normal range: 3.3 - 19.4mg/L), lambda light chain level was 10.1 (normal range: 600 - 1500 mg/dL). To date patient continues to follow up with the hematology oncology clinic and remains in remission.
Monoclonal gammopathies include multiple myeloma (MM), asymptomatic (smouldering) MM, monoclonal gammopathy of undetermined significance (MGUS), non-secretory myeloma and solitary plasmacytoma [5]. MM is a plasma cell neoplasm with systemic involvement presenting with hypercalcemia, renal disease, anemia, and bone lesions along with proliferation of monoclonal antibodies in the bone marrow. On the other hand,rare entities of plasma cell neoplasms known as plasmacytomas, which occur due to localized proliferation of plasma cells without systemic signs of MM. There are two main categories based on the location of tumors: solitary bone plasmacytoma (SBP) that presents as a single osseous lesion and extramedullary solitary plasmacytoma that presents as a solitary lesion in the soft tissues. Multiple solitary plasmacytomas (MSP) occurs as combination of both bone and soft tissue lesions with no bone marrow involvement as in this patient [6]. Our patient fits the definition of MSP with multiple osseous lesions and a soft tissue lesion with pathology showing proliferation of plasma cells from both biopsies along with the absence of hypercalcemia, renal insufficiency, and anemia. Hence, this is a rare case where both SP and EP are seen together.
Treatment of plasma cell neoplasms depends on tumor extent therefore, diagnostic imaging with CT/MRI is essential to know the extent of disease and to evaluate for presence of multiple lesions. Radiation therapy with or without surgical intervention depending on location and extent of involvement is the mainstay of treatment for SBP and EP [6]. Clinical outcomes of SBP in patients treated with radiotherapy alone without neoadjuvant chemotherapy is reported to be around 7.5 years to 12 years [7]. Patients undergoing radiotherapy usually have disappearance of the monoclonal (M) protein on follow up, however in persistence of the M protein after radiotherapy is considered as a poor prognostic factor [8]. Other prognostic factors for MM progression in such patients are age > 60 years and abnormal serum free light chains [9].
Management of MSP depends on the patient age, sites of involvement and number of lesions. In patients with systemic involvement as our patient, such patients benefit from systemic therapy as indicated in multiple myeloma. Given the rarity of MSP, no clear guidelines of management are available, however case reports have shown good response in patients with bortezomib and with use of thalidomide in combination with dexamethasone [10,11]. Due to the number of lesions in our patient, decision was made to use adjuvant chemotherapy with bortezomib and dexamethasone after initial surgical intervention and radiation therapy. The patient demonstrated exceptional response with the treatment regimen and continues to remain in remission on active surveillance with our clinic.
