Author(s): A Taqaddas
AlignRT® is a form of Surface Guided Radiotherapy (SGRT). Its use has recently been increased in various parts of the world. The aim of this study is to find out the current status of Surface Guided Radiotherapy especially AlignRT® in Proton therapy treatment and identify challenges and benefits associated with the application of Align RT from point of view of Radiation oncology professionals. A survey was created to assess clinical, technical, organizational and Educational strategies and resources employed to provide Surface Guided RT mainly AlignRT® based Proton therapy treatment in the responders’ Radiation Oncology centres . Another objective of the study is to discover if AlignRT® can completely replace IGRT. Survey was sent to four Radiation oncology professionals in USA and Germany. This has led to four case studies. The responses provide understanding of the current AlignRT® practices and though these responses are important they should not be considered to be representative of radiation oncology as a whole. The study was conducted in 2020.
Surface Guided Radiotherapy (SGRT) consists of surface imaging (SI) technology and Surface imaging is a form of optical Image guidance used in Radiation therapy to position patient accurately, to monitor intra-fraction motion and to carry out respiratory gating. Surface imaging technology uses 4 different types of optical surface scanning techniques i.e. Laser scanners, Time of Flight systems, stereovision systems and Structured light systems [1-4].
Various SGRT systems are operational in Radiotherapy worldwide such as AlignRT®, Optical surface monitoring system (Varian Edge Radiosurgery system), Catalyst, Identify (Humedi Q), Active Breathing Co-ordinator (Elekta), Real time position management system (Varian) [5]. AlignRT® and Catalyst utilize 3D optical stereovision scan of the body surface to verify patient position. AlignRT® is developed and marketed by vision RT (London, UK) to track patient skin surface in real-time with sub millimetre accuracy. If patient moves the AlignRT® automatically send signal to delivery system to pause the Radiation beam [6]. The AlignRT® system consists of three ceiling mounted scanners which in turn consists of two stereoscopic camera to produce 3D surface of the patient using passive triangulation, texture camera to provide grey scale image of the patient and a projector to project grey
scale pattern onto the patient to reduce inaccurate reflections and a light flash [5,7]. The 3D surface images from two scanners are combined by the AlignRT® software to generate a full 3D surface of the patient. This 3D surface is then registered with reference image. The align RT uses rigid registration whereas Catalyst uses Deformable registration algorithm [8]. Catalyst system is developed by C-Rad Uppsala, Sweden and consists of three ceiling mounted scanners and associated c4D software (Carl et al, 2018). For detailed knowledge of Catalyst System readers are referred to [9,10].SGRT is associated with a number of advantages such as no radiation dose (visual tracking of the Patient surface), availability of large surface for patient positioning compared to a few isolated marks such as in traditional tattoo and laser based setup, ability to monitor intra-fractional motion of the patient surface and isocentre in 6D and radiation is permitted when patient is within the given threshold [11-13]. All these capabilities have resulted in increasing use of SGRT in Radiation oncology departments. However the uptake of SGRT has been slow and many centres using SGRT are not availing all the features and full potential of the SGRT systems (AlignRT® and Catalyst). This warrants a case study of various Radiation oncology institutes where SGRT is being installed and used to determine not only its current status but also to identify the challenges facing the implementation and uptake of AlignRT® and Catalyst technologies especially in proton therapy centres and hospitals
1. Determine the current status of mainly AlignRT® and to some
extent Catalyst SGRT system in USA and Germany.
2. Identify the challenges and problems that Radiation oncology
professionals face when implementing SGRT in their
departments
3. Determine what organizational, clinical, treatment and
technical resources and strategies are employed with respect
to SGRT treatment and delivery
An E- questionnaire was designed to evaluate the current status of Surface Guided RT in the USA and Germany and to achieve better understanding and awareness of challenges faced in its implementation. The study evaluated AlignRT® (Vision RT) and Catalyst (C-Rad) surface guided Imaging systems in four proton therapy centres. The questionnaire was designed in MS word and consisted of 30 questions, most of which were close ended questions. Survey questions were structured in four sections namely i) Demographic, ii) SGRT institutional Background & Organizational resources, iii) Information about SGRT Technology, iv) Proton Therapy System Information and Problems associated with AlignRT®. A sample questionnaire is shown in Appendix A under supporting Information section.
Social media Website platform (LinkedIn) was used to reach out the respondents and provide them with a Questionnaire and study participation invitation letter. Professionals from Four different Radiation Centres from United States and Germany participated in this study. Three respondents were from Proton therapy Centre based in three states of USA (Cleveland, Ohio, Miami, Florida and Iowa city, Iowa) and one from Germany (Cologne). This resulted in 4 case studies (three in USA and one in Germany). Thus the present study is based on the views and opinions of four Radiation therapy professionals working in four different Proton therapy Radiation centres. The views and experiences of these professionals showed the clinical practices with respect to SGRT in 4 Institutes and these views provide important awareness about clinical, technical, organizational and Educational strategies and resources employed in these institutes with respect to SGRT. However by no means these views are representative of entire Radiation oncology field. The study was carried out in 2020. The Questionnaire length was 10-15mins depending on the experience of the respondent.
This study was deemed IRB exempt as it was a quality enhancement and evaluation study. Responses were anonymous so no ethical approval was required. No patients were approached. No medical or personal data of participants collected. By answering the questionnaires, the professionals agreed to give their informed consent.
Descriptive analysis was used to examine the results of the study
Four professionals from USA and Germany responded to E-survey. All four professionals worked in different institutes/organizations. Each respondent is assigned a code as shown in Table 1. The socio demographic profile of respondents is summarized in Table II.
| Respondent code | Countries | N (4) |
|---|---|---|
| R1US | USA | 1 |
| R2US | USA | 1 |
| R3US | USA | 1 |
| R4DE | Germany | 1 |
75% (3) of the respondents were male and 25% were (1) females. The most common age range was 40-50 years among respondents i.e. 50% of respondents belonged to 40-50 years of age range. Three respondents were married (75%) and one was divorced (25%). One respondent was Radiation therapist from USA, two were medical physicists from USA and one was Research medical physicist from Germany. Results are show in Figures 1-2.

Figure 1: Socio-Demographic profile of Respondents: Gender & Marital status
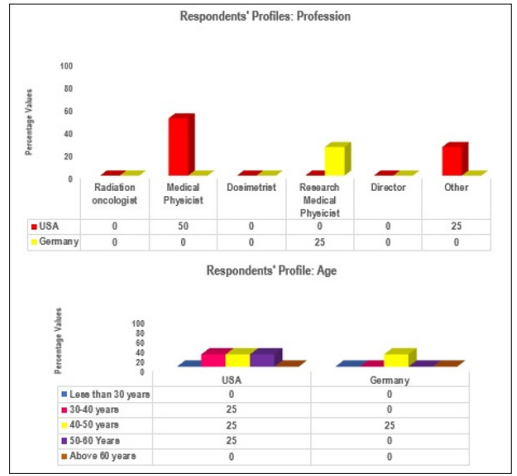
Figure 2: Socio-Demographic profile of Respondents: Profession & Age
Note: RT = Radiation Therapist, MP= Medical Physicist, RMP= Research Medical Physicist, OH= Ohio, FL= Florida, IA= Iowa. SGRT institutional Background & Organizational resources: Results are shown in Figure
R1US who was a Radiation therapist (25%) was working in a public Institute (hospital) in Cleveland Ohio, R2US was working in a not for profit institute in Miami, Florida and R3US, a medical physicist was working in an academic institute (University) in Iowa city, USA whereas R4DE, a Research Medical Physicist from Germany was working in a multinational Radiation oncology Hardware and software manufacturing (vendor) company in Cologne. Results are shown in Figure. 3

Figure 3: Socio-Demographic profile of Respondents: Type of practice & Geo-graphic location of working place
| Respondents | Gender | Age Range | Occupation | Marital status | Geo Location of Institute |
|---|---|---|---|---|---|
| R1US | Female | 50-60 | RT | Divorced | Cleveland, OH, USA |
| R2US | Male | 40-50 | MP | Married | Miami, FL, USA |
| R3US | Male | 30-40 | MP | Married | Iowa city, IA, USA |
| R4DE | Male | 40-50 | RMP | Married | Cologne, Germany |
100% of respondents said that they use SGRT in RT delivery. Results are shown in Figure 4
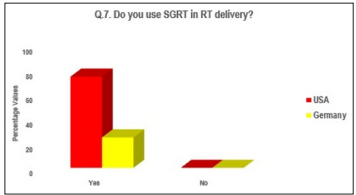
Figure 4: SGRT usage in RT
75% of the respondents said that they use AlignRT®. One respondent (25%) from USA said that they use Catalyst (C-Rad). Results are shown in Figure 5
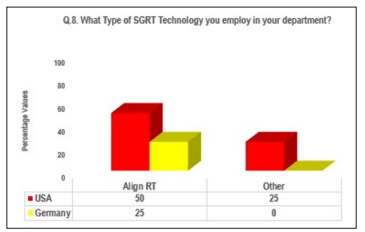
Figure 5: SGRT Technology
Do you think SGRT Usage Has Resulted in Needing More Staff? All the respondents from USA (75%) said No but respondent from Germany said Yes (25%) Results are shown in Figure 6
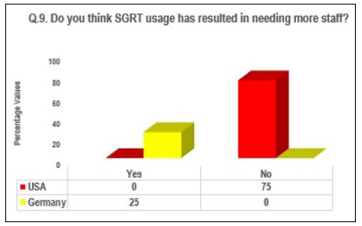
Figure 6: SGRT and staff requirements
Only two (50%) respondents from USA specified the number of professionals needed to give SGRT treatment where as other two respondents only specified which professionals are needed to give SGRT treatment. R2US said 4 professionals are involved in SGRT treatment delivery i.e. 1 medical physicist, 2 Radiation technologists and one dosimetrist whereas R3US said 5 professionals are needed to give SGRT treatment i.e. one Medical Physicist, 2 radiation technologists, one dosimetrist and one Radiation oncologist.
The Respondent (25%) from Germany said Implementation & integration of SGRT is complicated whereas Radiation therapist (25%) from Cleveland, Ohio said it can be confusing if procedures are not well defined. The Medical Physicist (25%) from Iowa said he do not know as he was not present in the institute at the time of SGRT implementation whereas the other Medical Physicist (25%) from Miami, Florida considered SGRT implementation an Easy process. Results are shown in Figure 7
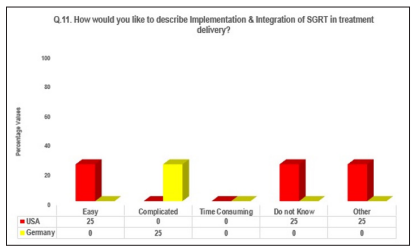
Figure 7: SGRT implementation in the department
The radiation Therapist from Cleveland, Ohio, USA said Lack of knowledge, training and Lack of compatibility with proton delivery system are some of the challenges faced during Implementation of SGRT for Proton therapy. The Medical Physicist from Miami, Florida said shortage of QA guidelines for SGRT setup and implementation was challenging whereas the other Medical Physicist from Iowa did not answer the question. The research Medical Physicist from Germany said timing delays in proton therapy are some of the challenges faced by them. Results are shown in Figure 8.
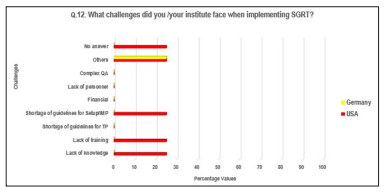
Figure 8: Challenges
Results are shown in Figure 9 -18
50% of respondents said that they have been using SGRT for 5 years. Both these respondents were from USA (R1US, R3US). One respondent (25%) from USA (R2US) said he has been using SGRT for 2 years and the Research Medical Physicist from Germany (R4DE) said he has been suing SGRT for 1 year.
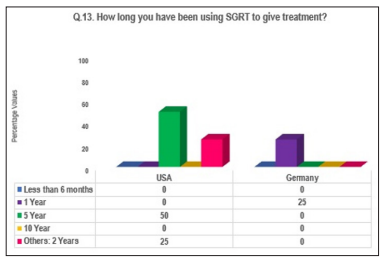
Figure 9: Figure 9 Duration of SGRT usages in the department/ organization
Research Medical Physicist from Germany said they use both types of registration techniques in their institute whereas the 50% of the respondents from USA (Cleveland and Miami centres) said they use Deformable registration in their institutes. Medical Physicist from Iowa, USA said they only use SGRT to monitor SBRT treatment and for DIBH (Deep Inspiration Breath Hold). The results are shown in Figure 10
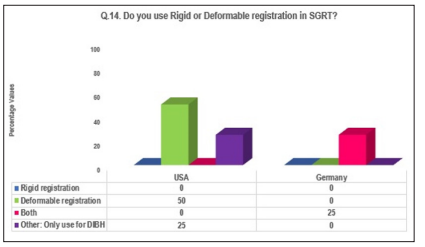
Figure 10:Rigid versus Deformable registration
The translational setup errors are indicated in x, y, and z directions where x= RT/LT, y= AP and z= Sup/Inf. The Radiation therapist from Cleveland Ohio, USA said they found 3mm Translation setup Uncertainty in their institute for lung and breast cancer patients whereas Medical Physicist from Iowa said they found 5mm or less. Medical physicist from Miami, Florida did not answer the question for Carcinoma of lung. However he said they found 8mm translational setup certainty for breast cancer patients. The Research Medical Physicist from Germany did not answer the question. Results are shown in the Fig. 50% of the respondents (RIUS, R2US) reported 3mm residual setup error for breast using both AlignRT® and Sentinel / Catalyst C-Rad SGRT systems while 50% of the respondents did not answer the question. 25% (R1US) of the respondents reported 3mm residual setup error for lung cancer patients with AlignRT® while 75% of the respondents did not answer the question.
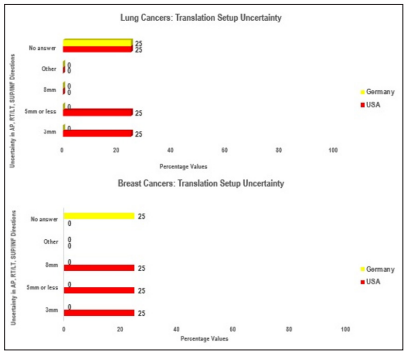
Figure 11: SGRT translation setup uncertainty in breast and lung cancer patients
100% of the respondents said that Breast cancer patients are suitable for SGRT treatment, 50% said lung cancer patients are suitable for SGRT, 25% said SGRT is suitable for Pancreas, Liver and for Mediastinal cancers. The radiation Therapist from Cleveland Ohio (R1US) said they find Breast, Pancreas and Liver cancer patients more suitable for SGRT setup. Medical Physicist from Miami, Florida (R2US) said they find SGRT suitable for Breast and Mediastinal cancer patients whereas Medical Physicist from Iowa (R3US) and Research Medical Physicist from Germany (R4DE) both said they find SGRT suitable for Breast and Lung patients. R3US further said that they use AlignRT® with DIBH in Breast cancer patients and for monitoring of SBRT treatment for lung cancer patients. Results are shown in Figure 12
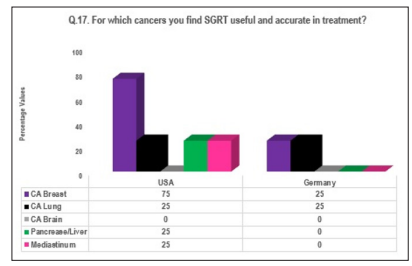
Figure 12: Cancers suitable for SGRT
50% of Respondents said to achieve more precise treatment delivery and another 50 % said to reduce treatment times, 25% said to reduce patient exposure, another 25% said to carry out online patient positioning monitoring and still another 25% said for Clinical research. Results are shown in Figure 13
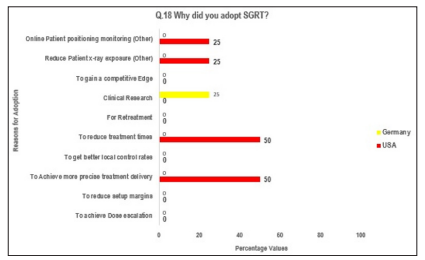
Figure 13: SGRT adoption reasons
R1US (25%) said SGRT system consists of Vision RT, the R3US (25%) from Iowa, USA said camera and work station whereas R2US (25%) from Miami Florida was not sure what question is about and R4DE (25%) from Germany did not answer the question. Results are shown in Figure 14.
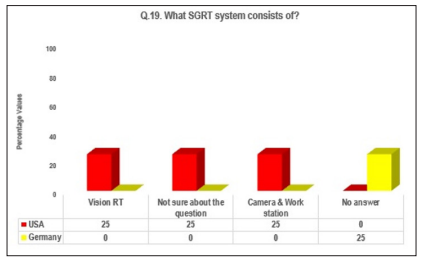
Figure 14: Responses regarding SGRT system components
Results for Question 20 and 24 are shown in Figure 15. All respondents (100%) said that they use SGRT in combination with other IGRT techniques i.e. SGRT complements plus other IGRT techniques such as Cone beam CT and KV orthogonal imaging. No respondent said SGRT can replace entirely KV or MV imaging. 50% of respondents from US (R1US,R2US) said that they do not think SGRT can replace entirely KV or MV imaging. R3USA said do not know and R4DE did not give any answer.
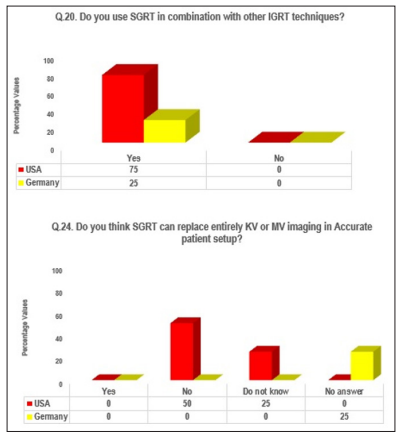
Figure 15: SGRT versus IGRT
R2US (25%) said offline review and better database Management is needed in SGRT system
SGRT and reduced setup margins whereas R4DE (25%) said that really fast reaction time is required with total delay less than 20ms. 50% of the respondents ( R1US and R3US) gave no answer. Results are shown in Figure 16
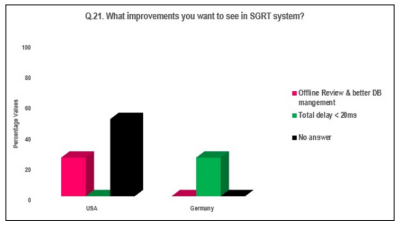
Figure 16: Improvements needed in AlignRT® & Catalyst SGRT systems
100 % of the respondents said SGRT has resulted in reduced setup margins in breast cancer patients. 50% of the respondents (R3US, R4DE) said SGRT has resulted in reduced setup margins in lung cancer patients. Results are shown in Figure 17
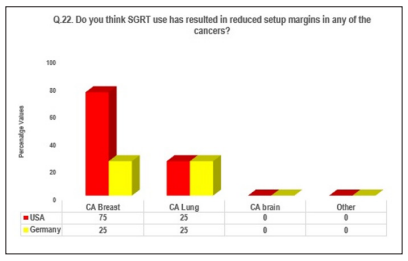
Figure 17: Reduction in setup margins with AlignRT® and Catalyst
50% of the respondents (R2US, R4DE) said yes. R1US said No and R3US said do not know. Results are shown in Figure 18
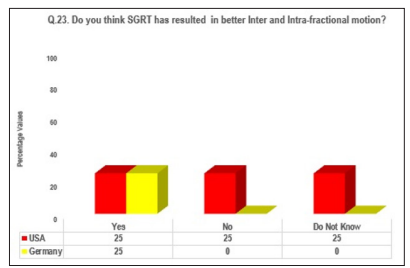
Figure 18: Intra & inter-fractional motion management with AlignRT® & Catalyst
In this section questions related to Proton therapy system and problems with AlignRT® were asked.
R1US said Mevion S250 Proton Therapy system, R2US said IBA (Author has assumed they meant IBA Proteus) and R3US did not give any answer. R34DE said Varian Probeam. Results are shown in Figure 19
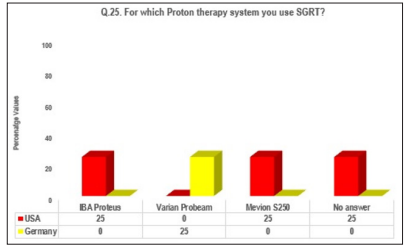
Figure 19: SGRT and Proton therapy system
R4DE (25%) from Germany said yes whereas R1US and R2US (50%) said No. R2US further said it find real time tracking useful but not sure about the accuracy of the internal organs. Author has taken his answer as a No. R3US (25%) did not give answer.
R1US (25%) said there is a lack of compatibility with the proton therapy delivery system components. The snout that is extended at the treatment position, obscures surface anatomy from infrared cameras. The treatment room is cold and patients can not be left uncovered for accurate alignment and surface tracking. R2US said when cameras are bumped we can not recalibrate ourselves. R3US said no answer. R4DE said positioning of SGRT systems is problematic i.e. facility room and gantry are different than in conventional Radiotherapy. He further mentioned gating requires much faster reaction time. Results are shown in Figure 20
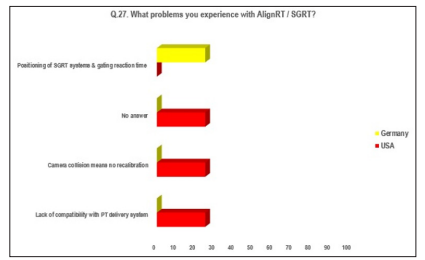
Figure 20: Problems with AlignRT® & Catalysts
Results are shown in Table III. 50% of the respondents do not answer the question. 25% said yes and 25% respondents do not use AlignRT® but use CRAD instead.
| Respondents | s Q.28. Do you find any couch error/deviation when using AlignRT® or SGRT? |
|---|---|
| R1US | Yes, sometimes when the proton components interfere with infrared camera on patient surfaces |
| R2US | Does not use AlignRT®. Use CRAD that does not have offline Review |
| R3US | No answer |
| R4DE | No answer |
25% of respondents consider AlignRT® useful in arm positioning if there are clear tolerances set. 25% of the respondents uses CRAD and finds this SGRT system specially good in this respect. 50% of the respondents did not answer. Results are shown in Table IV.
| Respondents | Q.29. Do you think arm positioning and surface alignment using AlignRT® in Breast Cancer is perfect or do you experience any problems? |
|---|---|
| R1US | Its definitely not perfect but is helpful in patient setup and arm positioning, If there are clear tolerances set for surface alignment in relation to bony anatomy and clear indication of which tolerances are acceptable and which are not. |
| R2US | CRAD is particularly good on this as it does project by how much arms need to be moved and where it is off. |
| R3US | No answer |
| R4DE | No answer |
Results are shown in Table V.
| Respondents | Q.29. Do you think arm positioning and surface alignment using AlignRT® in Breast Cancer is perfect or do you experience any problems? |
|---|---|
| R1US | No |
| R2US | Yes in breast cancer. Do not have experience with other sites |
| R3US | No answer |
| R4DE | Yes for positioning |
The present study is different from other studies as it has tried to uncover the current status of AlignRT® and C-Rad Catalyst based Surface guided RT in four Proton Therapy Radiation Oncology Centres/hospitals in USA and Germany. All of the respondents had SGRT in their organization. Half of the respondents have been using SGRT for 5 years.
The present study has shown that SGRT offers complementary information and cannot replace entirely KV or MV based Image guided Radiotherapy. The current study also showed that SGRT is used in combination with IGRT such as CBCT and KV orthogonal IGRT. Padilla et al. 2019 also argue that SGRT provides complementary and not contradictory information for image guidance and therefore despite the lack of correlation between surface and internal tumour motion, SGRT should not be rejected.
Majority of respondents reported Vision RT as their vendor that supplied AlignRT® SGRT system. In One respondent’s institute C-Rad, Uppsala acted as SI vendor and supplied Catalyst SGRT system.
The results of the present study show that SGRT is most commonly used for Breast cancer patients followed by lung, liver, pancreas and mediastinum cancer patients.
The study by Padilla also reported Vision RT, Varian OSMS and C-Rad as SGRT vendors while SGRT most commonly was used in Breast cancer patients [14]. A number of IG modalities such as KV imaging, MV imaging, CBCT or CBCT on rails and fluoroscopy were used to verify SI Gated position during the treatment.
A large proportion of respondents (75%) reported that SGRT (both AlignRT® and C-Rad) usage did not result in needing more staff. The data on number and type of professionals required to give SGRT based treatment is varied. Half of the respondents specified that in order to give SGRT based Radiotherapy treatment one Medical physicist, two radiation technologists and one dosimetrist are required.
Majority of the respondents found implementation and integration of SGRT complicated and confusing especially if procedures are not well defined. The present study showed that respondents faced various challenges when implementing SGRT for Proton Therapy. These challenges included time delay in Proton therapy, lack of QA guidelines, training and knowledge. This probably indicates the need for well-defined SGRT implementation and usage guidelines and perhaps standardization of SGRT usage and implementation protocols. This is in line with the recommendations of study conducted by Padilla that concluded guidelines and recommendations on commissioning and clinical use are needed to handle slow uptake of SGRT technology [14].
In a review conducted by Batista one of the challenges in implementing SGRT is the training and transition from using conventional 3 point setup to more complicated setup data and this can be managed by introducing SGRT related concepts such as troubleshooting, creation of clinical work flows and patient specific issues in the scope of RTT training [15]. Author of the present study thinks that same sort of SGRT based training and educational modules should be introduced in the curriculum and training of Medical Physicist and oncologists. Other methods described by Batista to improve SGRT training is by permitting sufficient time to practice, by removing other distractions so that clinical team can focus and acquire new knowledge, using SGRT in one cohort of patients (e.g. breast cancer patients) or learning about one of the applications of SGRT (e.g. use of SGRT for initial patient setup) before moving on to other cohorts of patents (lung cancer patients) and applications of SGRT (e.g. intra-fraction monitoring), vendor based training and assistance during commissioning and clinical implementation and vendors should communicate system and work flow pitfalls upfront to avoid violation of trust between users and vendors [15].
The reasons for SGRT technology adoption in the present study included online monitoring of patient positioning, to reduce patient X-ray exposure, to reduce treatment time, to achieve more precise treatment delivery and for clinical research purposes. A prospective study by Zagar showed that RT treatment with AlignRT® and DIBH in 18 left sided breast cancer patients resulted in no RT-induced cardiac perfusion abnormalities 6 months post-RT [16]. The results are based on Post-RT SPECT in 8 out of 16 evaluable patients. The mean heart does in all 18 patients was very low (range from 42 - 160cGy). A study by Marks without AlignRT® and DIBH resulted in 27% of the breast cancer patients developing volume dependent perfusion defects 6 months post-RT. 10-20% of the patients developed perfusion defects post-RT if less than 5% of the left ventricle volume was in the radiation field whereas 50- 60% of the patients developed perfusion defects if more than 5% of the left ventricle was in treatment field [17]. A case study of Northside Hospital Cancer Institute, Alpharetta was conducted to assess how AlignRT can improve treatment and work flow challenges. The study resulted in 50% decrease in patient treatment block times as a result of less frequent repeat imaging and more accurate initial setup with AlignRT®, 50% reduction in initial setup and verification appointment times and 14% reduction in tattoo-free in-room time [18].
The present study found a number of improvements that respondents want to see in SGRT system such as really fast reaction time with a total delay < 20ms, offline review and better Database management. This is something vendors need to work on to make SGRT more useful and accurate.
As far as inter and intra-fractional motion is concerned mixed responses were received with 50% of the respondents said that better inter and intra-fractional motion was achieved with SGRT whereas 25% said no and another 25% did not know. Similarly 50% of the respondents did not find SGRT based real time tracking accurate.
In the present study respondents found lack of compatibility of SGRT with proton therapy system components, camera collision and recalibration issues and slower reaction times in gating were some of the problems experienced by the respondents when using SGRT.
Translational errors can be rectified by moving treatment couch in Right and Left direction (i.e. laterally), in Superior and Inferior direction (i.e. longitudinally) and in up and down direction (i.e. vertically) in most Radiotherapy treatment machines where as rotational setup errors can be fixed by moving gantry and collimator to correct for target movements or by using 6D reposition device such as 6D couch [19,20].
In this study translational setup uncertainty was 3mm (25%) with AlignRT®, 5mm or less (25%) with AlignRT® and 8mm (25%) with C-Rad Catalyst in breast cancer patients in 3 proton therapy Radiation centres in USA i.e. in hospital in Cleveland, cancer institute in Miami and Academic institute in Iowa, USA respectively whereas Translational setup uncertainty was 3mm and 5mm or less in lung cancer patients in hospital in Cleveland, Ohio and Academic institute in Iowa, USA. A study found that smaller CBCT based 3D positional corrections are required for breast, Pelvis, abdominal and chest cancer patients when initially aligned with C-RAD Catalyst HD than those aligned with subcutaneous tattoos [21]. The results were statistically significant (p< 0.001). Breast cancer patients were found to have an average of postCBCT 3D corrections of 1.4 cm and 0.6 cm and standard deviation of 0.7 and 0.2 cm in three point localization and Surface imaging respectively. Chest and upper extremities patients were found to have an average of post-CBCT 3D corrections of 0.9 and 0.5 cm and Standard deviation of 0.6 cm and 0.3cm for three point localization and C-RAD Catalyst imaging techniques respectively. In the present study C-RAD based patient positioning in breast cancer patients reported 8mm translational setup uncertainty which is slightly higher correction reported by [21]. This could be due to the difference in registration technique and IGRT technique e.g. RIUS in Miami Cancer institute used deformable registration technique in SGRT and C-RAD positioning was confirmed using KV orthogonal and CBCT later.
In this study residual setup error (RSE) was found to be 3mm when using AlignRT® and C-Rad SGRT systems in breast cancer patients. A study by Laaksomaa et al. [11] found the systematic residual errors of the bony structures 3mm or less with SGRT-only in AlignRT® and Catalyst groups in DIBH treatment of breast cancer patients. The study also found reduction in systematic error of 2mm or less (except for shoulder joint) in both groups when SGRT was used with daily IGRT. The same study concluded that a heart planning margin of 3-7mm may be required due to errors in Pitch and superior/inferior direction.
A study by Jimenez et compared the accuracy of tattoo based setup to a tattoo free patient setup using AlignRT® in 20 APBI patients. They found statistically significant mean 3D vector shifts for initial setup for patients in the no tattoo compared to tattoo group whereas individual vector directions were not different between the two groups (shifts for Initial setup) [22]. Random and systematic errors were larger in the no tattoo group especially in superior/inferior direction due to absence of tattoos to lead patient alignment. However these errors were compensated by surface imaging prior to IGRT. Mean 3D vector shifts detected after Xray imaging data for patients in the No tattoo group compared to tattoo group were not statistically significant i.e. 4.6mm vs. 5.9mm respectively. Similarly Random and systematic errors were also not statistically significant.
A Word of Caution: Author of the present study did not find LinkedIn platform very reliable and it resulted in lose of some data due to unreasonable behaviour of LinkedIn team. For future studies Author recommend that if anyone wants to use LinkedIn platform to distribute E- questionnaire or to communicate with or recruit the participants of a study, make copies of all the correspondence in some other media as data can be lost at any time. Secondly Author of the present study recommend that other professional bodies ( e.g. American Association of Medical Physicists and American society of Radiation Oncology and ASTRO) in USA and other professional bodies in rest of the world, must develop social media platforms with equal and /or better capabilities than current social media platforms so that there is no need to rely on a handful of social media as there is a tendency for current social media platforms to exercise undue power and authority over accounts of professionals.
The present study involved only 4 case studies which is a limitation of the present study. Although the study has shown the current status of SGRT in 4 Proton therapy institutes and have provided valuable information, these views and opinions are not representative of entire radiation oncology world. Studies involving more Proton therapy institutes and Radiation oncology professionals working there are needed. Studies involving Quality of life of patients undergoing SGRT treatment are needed to see psycho-social effects of this technology on the patient.
The current status of AlignRT® and Catalyst as shown by four case studies is that it is used to complement IGRT and at present professionals do not think it can entirely replace IGRT such as KV orthogonal imaging or CBCT. A number of improvements in AlignRT® are suggested by the respondents such as fast reaction times. A number of challenges were identified by the respondents in the present study such as lack of compatibility of SGRT with proton therapy system components, camera collision and recalibration issues and slower reaction times in gating
Majority of respondents found implementation of AlignRT® in the department complicated and there seems to be need for welldefined SGRT implementation and usage guidelines and perhaps standardization of SGRT usage and implementation protocols. All of the respondents found that SGRT resulted in reduced setup margins for breast cancer patients. Two of the most common reasons for SGRT adoption were to reduce treatment times and to achieve more precise treatment. Couch errors and deviations were found with AlignRT® when used with proton therapy. AlignRT® and catalyst are found to be useful in breast and lung cancer Volume 2(5): 9-12
patients as well as in liver, mediastinum and pancreatic cancer treatment. 50% of the respondents reported 3mm residual setup error for breast cancer patients using both AlignRT® and Sentinel / Catalyst C-Rad SGRT systems. SGRT based training and educational modules should be introduced in the curriculum and training of Medical Physicist and Radiation oncologists.Author would like to thank you all respondents of this study especially Medical Physicist and Clinical Assistant Professor Sridhar Yaddanapudi at University of Iowa Healthcare USA for their valuable input (Assistant Professor Yaddanapudi permitted the author of the study to disclose his name).
Author discloses no conflict of Interest.
No funding or financial support was taken to carry out this Research.
Supplementary Data: Supplementary data related to this article can be found below:
