Author(s): Sashank Ayalasomayajula*, Ganesh Uttam Shingade, Yogesh Nene and Subrata Kumar Singha
Pituitary tumors may be non-functional or functional. Tumors that over secrete a specific trophic hormone are considered functional and lead to distinct hormonal syndromes [1]. Classically, pituitary adenomas are classified according to size as micro adenomas (diameter <1 cm) and macro adenomas (diameter >1 cm) [2, 3]. 20%–40% of patients with functioning pituitary adenoma can develop central hypothyroidism and hypocortisolism [4, 5]. A 42-year-old hypertensive lady, weighing 62 kg had undergone subtotal resection for a multi-compartmental pituitary macro adenoma with a ventriculo-peritoneal shunt procedure one year ago. Patient had a history of hyponatremia and hypokalemia postoperatively managed conservatively and was discharged. She now presented with recurrent seizures (10-15 per day) since 1 day. Endocrinology opinion was sought due to history of pituitary tumor with dyselectrolytemias leading to a complex differential diagnosis of Cerebral Salt Wasting (CSW), Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH), Central Hypothyroidism, Primary Hyperaldosteronism, Renal Salt Wasting Syndrome (RSWS) and Adrenal Insufficiency.
On present admission her serum sodium (Na+) and potassium (K+) were 137meq/L and 3.86meq/L respectively. Initial management included fluid restriction (1.5L/day), Hydrocortisone, Thyroxine, Tolvaptan, Prazosin, Levetiracetam & Sodium valproate. Serum Aldosterone levels and Plasma Renin Activity were normal. On day 15, patient had a Complex Partial Seizure (CPS) terminated with Injection Phenytoin. Her Na+ level was 122meq/L for which 3% hypertonic saline was started and Tablet Spironolactone added. Next day Na+ was 116meq/L. After stabilization, she received four cycles of radiotherapy for residual tumor. On day 45, patient had four episodes of CPS followed by loss of consciousness (Glasgow Coma Score 8/15) and desaturation after which she was shifted to Critical Care unit (CCU) where she was intubated and maintained on mechanical ventilation for 6 days. On day 7, elective percutaneous tracheostomy was performed. Over the next 10 days, patient had persistent hypernatremia (Na+-146-153meq/L) with concomitant hypokalemia (K+- 3-3.5meq/L). From day 11-20, patient had hyponatremia (Na+-124-134meq/L) with hypokalemia (K+-1.93-3.6meq/L). Alternating hyponatremia and hypernatremia were associated with hypotension (needing vasopressors) and hypertension respectively. From day 21 to shifting out of CCU on day 40 to a step-down facility, patient had persistent hyponatremia with hypokalemia, with normomagnesemia. In CCU, patient was on intravenous antibiotics, antiepileptics (Sodium Valproate, Phenytoin, Levetiracetam), antihypertensives (Amlodipine, Telmisartan, Labetalol) electrolyte supplementation (3% NaCl, KCl) and diuretics titrated to her clinical condition. She also had alternating cycles of polyuria and oliguria with no correlation to serum electrolyte levels. Her GCS never improved beyond 4/15.
Such a picture of frequently fluctuating fluid and electrolyte disturbances refractory to all management, does not fit into any one diagnosis among the previously mentioned differentials but rather seems to be multifactorial such as the tumor and its post-operative complications, radiotherapy and persistent seizures.
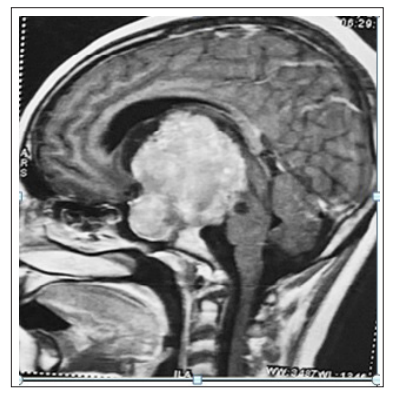
Figure 1: Sagittal section of MRI brain showing Giant Multicompartmental pituitary Macroadenoma
In such a clinical scenario where the patients’ neurological condition barely improved, all we are left with is to chase figures on monitor and laboratory parameters. This case poses a unique clinical challenge regarding the diagnosis and management due to its complex endocrinal pathophysiology, thereby encouraging scientific brainstorming to provide concrete suggestions which improve overall clinical outcome.
None
