Author(s): Manuel GS Botelho*, Guilherme B Capitango, Sandra JM Capamba and Julio Neto
ABSTRACT
Leprosy is an infectious-contagious, chronic granulomatous disease, with a long incubation period (2-21 years), caused by the Mycobacterium leprae complex. It has tropism for skin, mucous membranes of the upper respiratory tract, and peripheral nerves.We present a clinical case of a 24-year-old patient, phototype VI, from the municipality of Huambo, Benfica neighborhood, with a history evolving for about 18 months, without actually making any consultation and with several empirical treatments.
Leprosy is a chronic infectious disease caused by the Mycobacterium leprae complex, an acid-resistant bacillus (macrophages and swann cells). The reservoir is man, although it has been identified in wild animals such as monkeys and armadillos; However, the passage of the bacillus from animals to hoens has never been proven. Transmission occurs through the respiratory route, through contact with multibacillary and rarely paucibacillary patients. It can eventually be transmitted cutaneously through skin continuity solutions. The disease mainly affects the skin, peripheral nerves, upper respiratory tract mucosa, and eyes. If left untreated, it can lead to disabilities in a small proportion of patients. Visible deformities are one of the main causes of stigma that affects health-seeking behavior and social inclusion. Early detection and prompt treatment with multidrug therapy (MDT) can significantly reduce the burden of leprosy.
MDT has been made available by WHO free of charge to all patients worldwide since 1995. More than 17 million patients have received MDT in the last four decades. In addition to early diagnosis and treatment, contact tracing and single-dose rifampicin prophylaxis for contacts are recommended as preventive measures by WHO. In 2023, 184 countries, areas, and territories shared information on leprosy, accounting for 182,815 new cases, of which 72,845 (39.8%) among women and 10,322 (5.6%) among children. Globally, 9,729 new cases with G2D were detected and 266 (2.7%) of them among children. Most of the countries with high detection rates of new cases are in the WHO regions of Africa and Southeast Asia.
A 24-year-old patient, phototype VI, from the municipality of Huambo, Benfica neighborhood, with a history evolving for about 18 months, characterized by a sensation of dysesthesia in the upper and lower limbs, appearance of erythematous/brownish spots of variable size and shape, initially on the back, but disseminating throughout the body. The patient reports that after six to eight months, papules and nodules appeared, initially with mild itching, and in the last few days she reported reduced sensitivity, distributed in the extremities, bilateral earlobe, nose.

Figure 1: Nodules on the Nose Wing Figure 2: Nodules in the Lobe of the Left ear
Objective examination showed a thin appearance, BP: 90-50 mmHg. Dermatological examination shows erythematous- brownish lesions on the trunk and extremities, with five centimeters and a larger diameter on the back with decreased sensitivity, concomitantly papules-nodules on the extremities, right and left wings of the nose and earlobes (Figure 1, 2, 3 and 4).

Figure 3: Papules and Nodules in the Upper Limbs. Figure 4: Papules and Nodules in the Lower Limbs.
Hematological and biochemical tests (blood count, HCV, HBS, HTLV, creatinine, HIV) were performed without enhancement alterations, and sputum smear microscopy was positive.
Biopsy of a black skin fragment revealed diffuse granulomatous dermal infiltrate with the presence of globias (Figure 5 and 6).
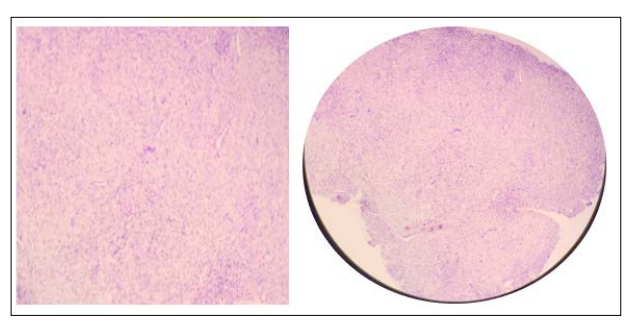
Figure 5: (Ziehl-Neelsen Staining Figure 6: (Ziehl-Neelsen Staining)
Oral treatment was instituted according to the WHO schedule (rifampicin 600 mg, dapsone 100 mg, clofazimine 300 mg). An active search for contacts and respective therapeutic prevention with rifampicin was also carried out.
Leprosy in Angola is still an important public health problem, with relevant morbidity and mortality. In 2023, according to the WHO, we had 839 new cases, 188 cases in women and 14 in patients under 15 years old.
In the case we present, the potential transmitting contact is a close relative who frequented the house and, like many, without follow-up in a specialist consultation and with various empirical treatments. In the active search, one more case was identified. The WHO leprosy case definition is M. leprae infection in an individual who has not completed a course of treatment and has 1 or more of the following:
Hypopigmented or reddish skin lesions with loss of sensation Peripheral nerve involvement, demonstrated by their thickening and associated loss of sensation. Positive skin smear for acid-fast bacilli.
This definition does not include patients who have completed a full round of treatment but still have residual deficiencies. The
WHO recommendation from 2018 onwards is to continue to base the diagnosis on the above clinical presentation combined with a confirmatory laboratory test, such as sputum smear or biopsy.
Skin biopsy, nasal swabs, or both are used to evaluate acid-fast bacilli using Fite staining. Biopsies should be of full dermal thickness taken from an edge of the lesion that appears most active. Serological assays can be used to detect phenolic glycolipid-1 (specific for M leprae) and lipoarabinomannan (commonly seen in mycobacteria). However, serological tests show low sensitivity for paucibacillary leprosy.Molecular probes detect 40-50% of cases missed in previous histological evaluations. Because probes require a minimal amount of genetic material (i.e., 104 copies of DNA), they may fail to identify paucibacillary leprosy.While the need for rapid and point-of-care diagnostic tests is recognized, these types of tests have yet to be developed.
Laboratory tests related to the follow-up of drug treatment include the following:
CBC count Creatinine level Liver function tests
The diagnosis of lepromatous leprosy is clinical and laboratory- based. Therefore, sputum smear microscopy and essentially biopsy must be done [1-12].
Applicants Declare no Conflicts of Interest
The Work We Presented had No Subsidies or any Financial Support.
The Authors Declare Strict Compliance With The Hospital’s Confidentiality Rules.
The Authors Declare to have the Consent of the Images Presented.
