Author(s): Parli Raghavan Ravi* and Hilal Ali Hamed Al Rashdi
Central venous catheterization is a commonly performed procedure in operation theatre. After the advent of ultrasound (US) guided central venous catheterization (CVC), the incidence of life-threatening complications has reduced significantly and are rare. We present a case of haemothorax in a young patient after US guided, which was inserted at the end of surgery under anaesthesia. The operator had some technical difficulty while inserting the CVC. The Haemothorax was diagnosed post-operatively in the ward after was missed clinically by radiological investigation. It was treated by inserting a 36 Fr chest drain on the second post-operative day which was removed on the seventh postoperative day and the patient was discharged to home.
Central venous catheterization is one of the most common invasive interventions performed in anesthesia and critically ill patients [1]. It can be associated with many complications. The vascular complications being common can be both extra-thoracic, such as damage to the carotid artery which is easily detected and controlled with manual compression. The intrathoracic vascular injuries are not only difficult to diagnose and control but can be life threatening. Hemothorax, albeit a rare complication is a dangerous one and can cause fatal outcomes. The advent of ultrasound and its use for accessing the central lines dramatically reduces the complications secondary to the procedure. However, there is still no guarantee of safety since the real-time observations of the guidewire insertion, dilator, and catheter tip insertion and its course are not impossible [2,3].
We present here a case of massive hemothorax after central line insertion, under ultrasound guidance, which was inserted at the end of surgery and was diagnosed in the post-operative ward.
A 27-year-old, 51 kg patient with a BMI of 20.2, a diagnosed case of Non-Seminoma Germ cell tumor was posted for retroperitoneal lymph node dissection (RPLND) with residual mass excision. He had no history of any chronic metabolic disease. All the preoperative blood (Hb 13.4mg%) and radiological investigations had no significant findings. Monitors in the form of NIBP, ECG, and oxygen saturation were attached to the patient. An epidural catheter was placed in the T6-7 intra-spinous space for postoperative analgesia. The patient was premedicated with Inj. Fentanyl 100 micrograms intravenous (i.v), Inj Dexamethasone 8 mg i.v. He was induced with Inj. propofol 100mg and a 7.4 mm ETT was passed after administering 50 mg of Rocuronium. He was maintained on oxygen, air, and desflurane. After induction and intubation of the patient, an arterial line was placed in the left radial artery for blood pressure monitoring. A temperature probe was placed in the oropharynx. Intraoperatively the haemodynamic course was normal. The surgery lasted for about 6 hours. Since the venous access was poor, it was decided that a central venous line would be placed in the right internal jugular. At the end of the surgery, after repositioning the patient, a central venous catheter () was placed using ultrasound (Philips USG machine) guidance. The puncture of the vein was made under ultrasound guidance. There was some resistance in passing the guidewire. The guidewire was pulled out and the process was repeated. The operator did a smooth insertion of the guidewire and then passed the CVC over the guidewire. The central venous catheter was fixed at the 15 cm mark and was confirmed fluoroscopically. Blood was aspirable only in two of the three ports of the CVC. The patient was then extubated and sent to the post-anesthesia care unit (PACU). The last arterial blood gas was within normal limits.
The total blood loss was 300 ml. At the time of discharge from the PACU to the ward the vitals were stable (HR 68/min, NIBP 110/76mm of Hg, oxygen saturation 100% on room air, ECG WNL). Two hours after the patient was shifted to the ward there was a fall in the blood pressure (NIBP 90/60 mm of Hg). The patient was given a bolus of 500 ml of RL and the epidural infusion was reduced from 6 ml (0.125 percent Bupivacaine) to 4 ml. However, the patient persisted in having intermittent episodes of hypotension, which responded to boluses of fluid and small doses (3mg of ephedrine) of vasoconstrictors. The abdominal drains placed during the surgery had a minimal amount of slightly blood-tinged fluid. All the boluses were given in the peripheral line. On postoperative day 1 patient hemoglobin fell to 6 grams percent and the patient remained hypotensive, however responsive to fluid bolus and inotropes.
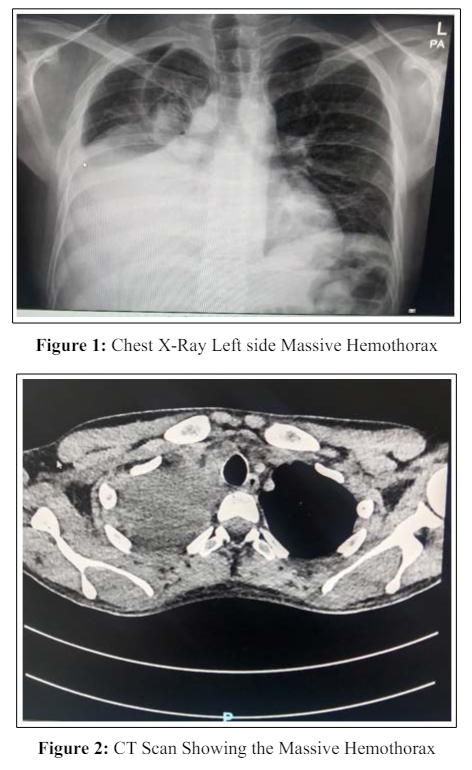
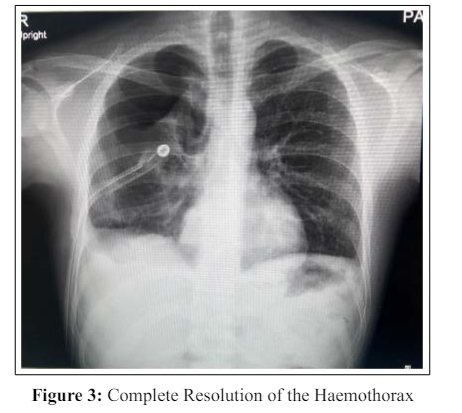
However, the abdomen was soft on examination. On auscultation, there was apparent decreased air entry on the right side of the chest. Two units of cross-matched blood were transfused. After 48 hours, the patient stabilized hemodynamically. The patient had an oxygen saturation of 92 to 94 % with the facemask O2 of 2-3L/min. so an ultrasound abdomen/chest and chest X-ray were done. Chest X-ray revealed a massive hemothorax of the right lung (Figure 1) and it was confirmed on CT scan too (Figure 2). A 36 size chest tube was placed and it drained almost 1.4 liters of blood. The haemothorax resolved completely (Figure 3). The patient was given one more unit of blood. The central line was removed on the 3rd post-operative day and compression was given. The patient’s hemodynamics stabilized. On day 7 postoperative day, the patient developed a low-grade fever of 37.8C. The patient was sent to the opinion of a cardiothoracic surgeon and was later discharged from the ward after the removal of the chest tube after 07 days. The hemothorax had completely resolved at the time of discharge.
The neck and the thoracic inlet have a complex network of major vessels. Hence Hemothorax can occur during the insertion of CVC when the intrathoracic artery or vein is damaged or perorated by the dilator, guidewire, or catheter [2].
The earliest and the most important sign of any vascular injury is hypotension, which is sudden and unexpected. In our case, the diagnosis of hemothorax was delayed. Probably the reason was that the hypotension did not occur immediately and the patient responded to boluses of fluid and small doses of vasoconstrictor, which clouded the decision of the clinician. Early diagnosis of hemothorax requires a high degree of suspicion and aggressive clinical and radiological examination of the patient, especially when the surgical drains are not draining commiserating blood [3,4]. We should have performed the portable X-ray or USG at the first instance of hypotension. Studies have shown that a bedside USG can diagnose the hemothorax faster than the X-Ray.
While inserting the CVC, the operator always predicts the entry of the needle and the catheter into the central vein by aspirating the blood. However, even aspiration of the blood is not always an assurance that the catheter is properly placed [4]. It must be presumed that when one of the ports is not aspirating blood, the catheter might be misplaced or is inappropriately located. In our case, we were not able to aspirate blood from one of the ports and hence it should have been considered a red flag in our case.
The introduction of ultrasound has dramatically reduced the incidence of vascular injury. Multiple studies have reported almost nil to low incidence of vascular complications after using USG. However, there are some reports of injury to the right subclavian artery (RCA) and right and left Brachiocephalic veins (BCV) [2,5]. The US guidance will always help in adjusting the insertion point and the depth of the vessel to avoid injury, however, there are some reports of vascular injuries, although few under US guidance also. Ultrasound guidance will not help prevent intrathoracic vascular injuries due to dilator, guidewire, or catheter insertion inside the thorax [5]. If the damage is in the arterial vessel, the deterioration of the vital signs will be rapid and can be a fatal event, in comparison to venous structures, where the clinical deterioration is slow and may even be missed or diagnosed late [5,6]. Arterial injuries may require immediate thoracic exploration.
In our patient most likely it was a venous injury of the thoracic vessel either of the right IJV or RT BCV.
Multiple mechanisms can be postulated while dwelling upon the literature for the possible mechanism of the injury in our case of BCV. Damage to IJV is rare as it is usually supraclavicular and can be easily made out by the US. Firstly, there is always a possibility of the guidewire from the right IJV advancing into the wrong vessel, such as into the right subclavian (SCV), azygous, or even left BCV causing injury to the vessels [5-7]. Although the proximal part of the guidewire will be within the IJV, that does not guarantee the distal part of it to be in the proper position in the thorax. This can especially be disastrous if the dilator is inserted with force after the guidewire has damaged the SCV. Forceful insertion of guidewire, hence, should never be done. In our case, the operator had got resistance in the first attempt. It is quite possible that in the second attempt when the dilator was inserted over the guidewire, it could have damaged the right SCV. Secondly, the dilator should never be inserted below the clavicle. It should be used to dilate the subcutaneous space only. A forceful and deep insertion of the dilator can damage the right BCV directly.
There is a two-step safety procedure described for Central venous catheterization. Firstly, both the short-axis and long view should be done for the real-time puncture of the needle insertion into the IJV [3,5]. The second is to verify the position of the guidewire in the BCV using a short axis and coronal view. This will help to detect the malposition of guidewire in the BCV [3,5].
The possibility of damaging the vascular structure exists during the insertion of CVC even though ultrasound is being used for guidance. It is important to aspirate to come out of all ports. It is also desirable that adequate knowledge of the technique is available when doing real-time guidance of the insertion of CVC. The guidewire, dilator, and catheter all are potent sources to cause damage to the intra-thoracic vascular structure. A high degree of clinical suspicion of hemothorax should be there in case of hypotension occurs in a patient with recent insertion of CVC as venous bleeding may trickle and cause massive haemothorax slowly without causing much clinical deterioration. Haemothorax developing on the same side, where the CVC has been established should be attributed to CVC until proven otherwise.
