Author(s): Maura Mancini*, Claudio Brancato, Gregorio Lo Giudice and Antonino Pioppo
Introduction: Intraocular foreign bodies (IOFBs) are unusual and can cause serious eye damage.
Case Presentation: We present a case report of a 62-year-old male patient who presented to our ophthalmic emergency department with an intraocular foreign body following a domestic accident.Imaging evaluation with facial CT scan confirmed the presence of a foreign body, made of glass, without any associated bone fractures.
Conclusion: Previous studies have emphasized the potential complications and visual consequences associated with these injuries.This case report contributes to the existing literature on intraocular foreign bodies and reinforces the importance of prompt diagnosis and appropriate management.
Intraocular foreign bodies (IOFBs) are unusual and can cause serious eye damage. These are foreign objects that end up inside the eye due to an injury. They can cause a range of problems inside the eye and can affect your vision. Most of these IOFBs are found in the back part of the eye [1, 2]. The seriousness of the damage depends on the size of the foreign object, where it entered the eye, and any problems that came up after the injury [3]. In case of serious injuries that puncture the eye, we look at the furthest point the injury reached, not where it first entered the eye. These IOFBs can cause direct damage as they enter the eye. They don't always travel in a straight line and can bounce around, causing more damage [1]. The amount of damage an IOFB causes depends on many things. For example, the length of the wound can tell us if the retina might be hurt. A shorter wound could mean that the IOFB traveled further into the eye and could have reached the retina. IOFBs that enter through the white part of the eye, the sclera, are more likely to cause internal damage than those that enter through the clear front part of the eye, the cornea [4]. Most IOFBs are made of metal. When doctors need to find an IOFB, they might use different imaging techniques depending on what the IOFB is made of [5].
We present a case report of a 62-year-old male patient who arrived at our ophthalmic emergency department with a history of accidental ocular trauma in a domestic setting, resulting in damage to the right eye. The patient has signed the informed consent for the processing of personal data. On presentation, the patient had light perception visual acuity in the right eye and reported no ocular pain but significant discomfort and burning sensation. General medical history was unremarkable. The patient reported a domestic accident that transpired during the preparation of a fireplace fire. Anterior segment examination revealed anterior chamber synechiae, traumatic cataract, marked conjunctival hyperemia, and two scleral lacerations. The posterior segment was unexplorable. The left eye exhibited normal findings on clinical examination of both the anterior and posterior segments. A facial CT scan was performed, which revealed the presence of a hyperdense foreign body measuring up to 1.3 cm in the anterior portion of the right eyeball, accompanied by gas within the eye. No traumatic bony lesions were detected. (Figure 1) The patient immediately underwent emergency intravenous antibiotic therapy (vancomicin). The decision was made to proceed with surgical removal of the intraocular foreign body in the right eye. Under general anesthesia, the scleral breach was visualized upon opening the conjunctiva. The anterior chamber exhibited irispupillary synechiae and a traumatic cataract. Touching the scleral breach resulted in immediate vitreous emergence. Subsequent fundus examination revealed the foreign body near the optic disc, suggesting it had previously been embedded in the crystalline lens but fell down upon contact with the scleral breach. Cataract surgery was performed, with phacoemulsification complicated by nucleus drop. The foreign body, made of glass, removed through the corneal access (Figure 2). Typically, extracting IOFBs via the entry wound is not advisable, as it could lead to further damage during the removal process [1]. Posterior vitreous detachment was induced,
followed by triamcinolone-assisted vitrectomy. Laser treatment was applied to an iatrogenic paramacular tear, and cryotherapy was performed on the scleral breaches to prevent tractional consequences on the incarcerated vitreous. The sclerotomies were sutured, air tamponade to conclude the procedure. Ocular therapy included a regimen of broad-spectrum oral and topical antibiotics in conjunction with topical corticosteroids. Postoperative course was uneventful, and the patient did not experience any ocular infections. Three months postoperatively, the patient demonstrated a Best Corrected Visual Acuity (BCVA) of 0.5. The patient remains aphakic with a trophic iris. Ocular adnexa appear to be in good condition, and normal ocular motility is observed. However, the pupil exhibits slight irregularity and reduced reactivity to light stimulus. Currently, the patient is awaiting scleral fixation lens implantation, and the planned procedure is presumed to follow the Carlevale technique. Further follow-up and assessment will be necessary to monitor the patient's visual outcomes and the success of the planned scleral fixation lens implantation procedure. At three months postoperatively, additional imaging was performed using the Zeiss Clarus 700 retinal camera UWF. The findings are as follows: Retinal flattening is observed, indicating a stable retinal configuration. A laser-treated area is present temporally at the macula, suggesting previous laser photocoagulation treatment. The optic disc appears normal, without any evident abnormalities. Laser photocoagulation marks are noted beyond the vascular arcades, indicating the extent of the previous treatment. (Figure 3). In the blue light fundus autofluorescence imaging, the lasertreated area demonstrates hyperautofluorescence, indicating increased metabolic activity or altered retinal pigmentation in that region. Similarly, the laser photocoagulation marks exhibit hyperautofluorescence, confirming the presence of treated areas. In contrast, the fovea demonstrates classic hypoautofluorescence, suggesting normal retinal pigment epithelium function in this central area. (Figure 4) These imaging findings provide valuable insights into the postoperative status of the patient's retina and the effects of the previous laser treatment. Continued follow-up and monitoring will be essential to assess the long-term stability and functional outcomes of the retina following the planned scleral fixation lens implantation procedure.
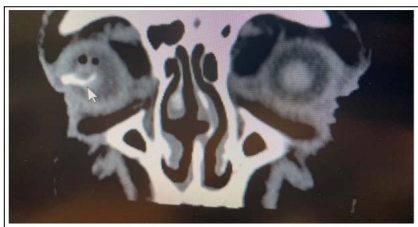
Figure 1: A facial CT scan: Hyperdense foreign body measuring up to 1.3 cm in the anterior portion of the right eyeball (white arrow), accompanied by gas within the eye. No traumatic bony lesions were detected.

Figure 2: The foreign body (glass nature)
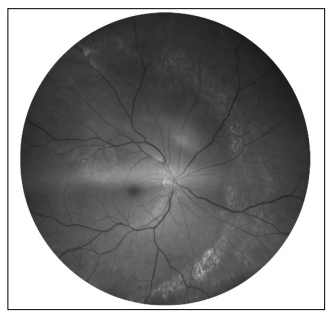
Figure 3: Fundus Photography at three months postoperatively (Zeiss Clarus 700 retinal camera UWF): Retinal flattening is observed, indicating a stable retinal configuration. A laser-treated area is present temporally at the macula, suggesting previous laser photocoagulation treatment. The optic disc appears normal, without any evident abnormalities. Laser photocoagulation marks are noted beyond the vascular arcades, indicating the extent of the previous treatment.
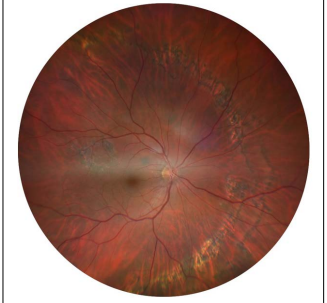
Figure 4: Blue light fundus autofluorescence at three months postoperatively (Zeiss Clarus 700 retinal camera UWF): The laser-treated area demonstrates hyperautofluorescence, indicating increased metabolic activity or altered retinal pigmentation in that region. Similarly, the laser photocoagulation marks exhibit hyperautofluorescence, confirming the presence of treated areas. In contrast, the fovea demonstrates classic hypoautofluorescence,suggesting normal retinal pigment epithelium function in this central area.
The case presented herein describes the successful surgical management of an intraocular foreign body and traumatic cataract resulting from ocular trauma. Ocular trauma can vary significantly in severity, ranging from mild injuries that only require basic medical care to severe injuries that necessitate urgent surgical interventions. It is important to note that specific statistics can vary depending on factors such as geographic region, age of patients, and type of ocular trauma. In general, ocular trauma is a significant cause of morbidity and can lead to serious vision-related consequences. An essential step in the pre-operative management of IOFBs is to collect a detailed history. The patient's background should underscore the injury's cause, the environment in which it transpired (e.g., occupational setting), and the precise date and time of occurrence [1]. Previous estimates suggest that there are approximately 2.5 million ocular traumas annually in the United States, with approximately 10-15% of cases requiring urgent surgical intervention [8, 9]. The most common consequences of ocular trauma requiring urgent surgical intervention can include corneal injuries, orbital fractures, intraocular hemorrhages, retinal detachments, iris or ciliary body lacerations, and scleral perforations. These complications can result in vision loss, infections, glaucoma, traumatic cataract, and other ocular pathologies [10, 11]. The presence of an intraocular foreign body in the eye is a rare occurrence, and its timely identification and appropriate intervention are crucial to minimize potential complications and preserve visual function. Patients sometimes do not experience pain or changes in visual acuity and are unaware that objects might have entered their eyes.
In the literature, there are several published reports of intraocular foreign bodies causing ocular trauma. Smith et al. conducted a systematic review on ocular injuries from intraocular foreign bodies, highlighting the varied nature of these injuries and the importance of prompt diagnosis and management [6]. Similarly, Johnson et al. provided a comprehensive review of the diagnosis and management of intraocular foreign bodies, emphasizing the potential complications and visual consequences associated with such injuries [7]. The timing of IOFB removal relies on various factors. These include the patient's general health condition (such as the presence of life-threatening injuries and surgical tolerance), the specifics of the injury (for instance, heat-sterilized projectiles are probably less prone to causing infectious endophthalmitis compared to contaminated IOFBs from farm injuries), and the IOFB's composition (for example, pure copper IOFBs trigger a strong inflammatory response, whereas glass IOFBs are typically inert and better tolerated) [1].
Ensuring coverage for commonly encountered pathogens in this context, such as Bacillus, Clostridium, and coagulase-negative Staphylococci species, is crucial. [1] In our case, the presence of an intraocular foreign body was confirmed by facial CT scan. The decision to proceed with surgical removal was based on the potential risks posed by the foreign body, including the possibility of infection, inflammation, and further damage to ocular structures. The surgical procedure involved a combination of cataract extraction and vitrectomy, aiming to remove the foreign body and address the associated traumatic cataract.
It is worth noting that the management of intraocular foreign bodies can be challenging, requiring a multidisciplinary approach involving ophthalmologists, radiologists, and trauma specialists. Previous studies have highlighted the importance of collaboration among these disciplines to achieve optimal patient outcomes [12, 13]. Comparing our findings with other published reports of intraocular foreign bodies, similarities can be observed in terms of the varied nature of foreign bodies encountered. For instance, previous cases have reported the presence of metallic, glass, or organic materials as foreign bodies [6, 7].
These reports further emphasize the need for a thorough evaluation and tailored surgical approach based on the specific characteristics of the foreign body. In our case, careful surgical planning, including precise localization and removal of the foreign body, was essential in restoring visual function and minimizing potential complications. Continued follow-up and monitoring will be crucial to evaluate the long-term stability and functional outcomes of the retina, particularly following the planned scleral fixation lens implantation procedure. Long-term assessments will help determine the impact of the treatment on visual acuity and overall retinal health. These findings highlight the importance of comprehensive postoperative care and ongoing surveillance in optimizing patient outcomes. The CARE Checklist has been completed by the authors for this case report, attached as supplementary material.
In conclusion, this case report highlights the successful management of an intraocular foreign body and traumatic cataract through surgical intervention. The prompt identification, accurate localization, and meticulous removal of the foreign body are crucial for preserving visual function and preventing potential complications. Our findings contribute to the existing literature on intraocular foreign bodies, emphasizing the importance of a multidisciplinary approach and individualized surgical strategies for optimal patient outcomes.
Through this report, we aim to increase awareness among clinicians about the clinical manifestations, diagnostic challenges, and therapeutic considerations associated with intraocular foreign bodies. By sharing our experience and discussing the management approach employed, we hope to contribute valuable insights that can aid in improving patient outcomes in similar cases. Further studies and case reports are warranted to expand our knowledge on the management of intraocular foreign bodies, including the development of standardized protocols and guidelines. These efforts will help improve clinical decision-making and enhance patient care in similar cases of ocular trauma.
This manuscript did not require ethical approval in accordance with local/national guidelines. This published case report complies with the guidelines for human studies in accordance with the World Medical Association Declaration of Helsinki. The patient provided written informed consent for publication, including publication of images.
All authors declare no conflict of interest.
No funding or grant support was received for publication of this clinical case.
A.P was Head of the Unit Board. G.LG revised the manuscript. M.M and C.B. wrote original draft of this case report.
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
