Author(s): Barbero A*, Morales M and Roldán L
Until 2019, hearing aid molds were made with silicones that copied the shape of the ear, creating a positive and a negative mold to reproduce the shape and volume in cubic centimeters of the ear. This system had the disadvantage of lack of precision. Due to the pressure of the silicones during their placement in the ear, the soft tissues are deformed.
This is especially important when the deafness is severe or profound. Because a very high sound power is required and sound leakage occurs. That leaking sound is feedback into the hearing aid microphone and generates a “Larsen effect.” Patients describe this sound feedback as very high-pitched beeps from the hearing aid that can be heard by family and others close to them. During the time that the hearing aid is whistling, the user loses information and hearing, as well as being annoying for the family. In the case of high-powered hearing aids, it is difficult to balance the sound leakage that generates the “Larsen effect” and the excessive pressure that forms the canal. Also bear in mind that the user of this type of hearing aid uses it all day, so a little discomfort translates into anguish and nervousness.
This is not an easy task for the audiologist, nor for the laboratory technician making ear molds. They are known by the technicians as “High Risk Feedback Molds”. Recently, 3D laser light measurement has been used for measurements. By not having contact with the skin, this new technique allows the tissues not to deform. And it gives us a view from inside the ear (and this is another novelty) because they are done by means of a small probe that acts as a laser beam that we introduce into the ear canal itself.
For most experienced Audiologists, creating a mold by copying the shape of the patient’s ear is part of their daily job. This task has been carried out for many years, with mixtures of silicones dosed with spoons and injected into the canal, using syringes. This task was almost more artistic than technical. Because afterwards, the silicone molds had to be shaped and retouched to achieve the appropriate counter-molds, which would finally generate the final earmold. (See figure 1: Silicone earmold, syringe, spoons, and silicones:
Over the years, silicone already comes in dosing tubes with the exact quantities and the injectors became of the “gun” type either with manual mechanical systems to inject or with motorized systems to inject without using the strength of your hand.
In addition, cannulas are used for the injectors that mix the two components, at the same time that they pass from the injector to the cannula and from there to the patient’s ear. This makes the process of catalyzing and hardening the silicone more homogeneous (see figure 2: automatic and manual injectors; and figure 3:Two components silicone and cannula).
But… What happens when the mold that we need to make is intended for a patient who needs high sound amplification? Here the precision and accuracy of the mold become essential. Imperfections, air bubbles or excessive silicone pressure (or otherwise very weak), can generate invalid molds. Especially in patients who use UP (SuperPower / UltraPower) hearing aids because they suffer from quite high levels of deafness. (See figure 4 for output curves of a superpower hearing aid)
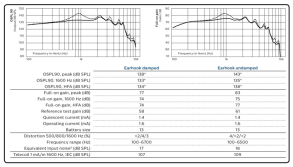
Figure 4: Ultra Power BTE curves
In addition, in the case of patients with significant hearing loss, the inconvenience is added that they wear their hearing aids for many hours, practically all day. For this reason, a perfect fit of the mold becomes essential. Comfort in use throughout the day is an aspect highly valued by the user. The accuracy of the ear copy is very important.
What is usually the problem? The problem is that the need to achieve a precise fit and a good seal of the canal (so that the power delivered by the hearing aid is used to the maximum without wasting decibels), sometimes causes that you have to put a lot of pressure on the silicone so that the mold is well adjusted. This pressure of the silicone when injecting, generates a force on the soft tissues of the canal, especially in its outermost area. When this copy is passed (using the mold and counter-mold technique) to the final mold that the patient must use in your daily life is not as comfortable as you would like, because the pressure has modified the natural shape of the pavilion. In obese people, this is especially significant.
On other occasions we find the opposite effect: that is, as there is not enough pressure in the injection of the silicone into the duct, the final mold that we will obtain will leave sound leaks. Which, in high-power devices, generates the “Larsen effect. That the user describes as an anguished beep, which takes away sound information, making his already precarious communication even more difficult. And it also becomes an annoying situation for family members who live with the hearing aid user. This effect occurs because the sound generated by the high-power earphone escapes from the ear canal, returning to the microphone that picks it up and amplifies it again in the electronic circuit. And so on, creating a re-amp loop. You have been able to see this phenomenon at concerts, when the singer approaches a speaker with his microphone or the mixing engineer turns up the power to the amplifier excessively, generating a very annoying beep to those attending the concert.
Today, technology and advances in microchips and the software that hearing aid manufacturers use to generate hearing aid processors have dramatically reduced this problem. “Larsen effect cancellers” are used to digitally detect and cancel those beeps. The current circuits are very good and very precise, some of them even go ahead and avoid the possible “risk” of sound feeback (Larsen), modifying the responses offered by their amplifiers when detecting these situations at the input of the microphones. But despite this, the audiologist often finds himself at an audiological border that is difficult to determine. Especially in cases of severe and profound deafness. The audiologist must “play” in a complicated balance. On the one hand you must obtain a few more decibels of power to provide information to your patient or on the other hand be conservative and avoid the risk of the annoying beep of the Larsen effect. They are called “HIGH RISK EARMOLDS FOR SOUND FEEDBACK”. That’s where a really good mold technician takes a risk, professionally speaking. That balance is very small and experience and expertise in these cases becomes the best tool.
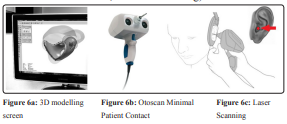
To try to alleviate this problem, since 2018/2019Laser Light systems for 3D measurements inside the ear have been incorporated [1]. Using a microscanner system that we introduce inside the ear canal with a thin emitter beam, we can digitally scan the ear without touching the skin of the canal. As there is no contact with the walls of the canal, we do not generate any deformity of the canal. The shape of the copy that we obtain, will be that of its shape and natural size in the resting position. (see fig 5: 3d laser scanning, 3D digital earmould, and Otoscan3D).

No deformities, or areas subject to pressure, as we did with injected silicones. We simply insert the tip of the beam into the canal, emit the light from the 3D scanner, and copy the exact shape of that canal, scanning every fold and every curve. This has been a great advance for audiologists when it comes to making copies of the ears and molds of their patients. But especially in the cases of “High Risk Sound Feedback EarMolds”, for significant deafness that require very high sound pressure and amplifications [2].
Another advantage of this new copying system is that the digitized mold that we obtain can be used as many times as we need, since the measurement is not lost in the copying and counter-mold process. These digitized systems are molded and sculpted on the screen, allowing us to create 3D models in which we can make virtual tests of how they will look when they are finished or how many components fit inside (in the case of CIC hearing aids, inside the canal), in which miniaturization is essential and size does matter, a lot. (see fig6: 3D modelling screen, Otoscan Minimal Patient Contact, and laser scanning)
These systems also do not require the placement of an “otoblock” obturator, prior to the eardrum (as with silicones). The mission of the otoblock is to avoid that when the silicone is injected deeply, it reaches the tympanic membrane (with the risk that this implies).
And they also avoid the problem of having to copy with silicone ears that have had previous surgeries and have important cavities that endanger the taking of the mold using silicones. The increase in use among Audiologists of this auditory canal copying system is being very fast. Because it offers a non-contact system, without allergies to silicone, clean, that does not deform tissues and is very visual to touch up or open vents on the 3D software screen. Digital scanning and 3D modeling allow you to make and undo the design as many times as you want (see Fig7-Otoscan Minimal Patient Contact Advantages).
This is causing the professionals to go from being called HIGH RISK MOLDS to being called LOW RISK MOLDS. And at the other extreme, that is, mild deafness with CIC (Completely In Canal) hearing aids, that we can reduce the size of our designs for CIC models and offer more aesthetics to our patients without losing sound efficiency [3]. Definitely in a few years it will become the new standard, because all the manufacturers of the BIG4 group have incorporated these systems into their manufacturing laboratories and already receive the orders for the molds that Audiologists make directly through the cloud (OtoCloud) on the Internet. This reduces the shipping time of the old silicone mold from the Audiologist’s office to the manufacturer’s laboratory by two days. Currently the copy of the patient’s ear is as close to the laboratory technician as a mouse click on our computer. This opens up new very interesting paths in Audiology and Anaplastology, we will see how far “the way forward” goes ...
