Author(s): Adrián P. Huñis* and Melisa Huñis
Although the primary intraosseous angioma or hemangioma, although it rarely affects the bones of the orbit, it should be taken into account in the differential diagnosis in those patients who present a fixed mass in the orbit or signs of progressive proptosis, sometimes not painful. For the therapeutic approach, it is critical to assess the exact location and extent of the lesion by CT and MRI, and to establish whether it has a vascular origin, since improper management can lead to severe bleeding. Surgical treatment is indicated for progressive proptosis or cosmetic deformity. We present the case of a patient with primary intraosseous hemangioma of the supralateral rim of the orbit, we review the bibliography of this very low prevalence disease and we trust that in this way, we contribute to the casuistry.
Angiomas and vascular malformations are the most common neoplasms in the soft tissues of the orbit. However, angiomas with a primary location in bone represent less than 1% of all bone neoplasms. More than 50% appear in the vertebrae and the skull, affecting in the latter location especially the frontal and parietal. About 5% are diagnosed in the bones of the orbit. Primary orbital intraosseous hemangiomas are benign neoplasms that present as a hard mass that in its slow growth can cause significant facial deformity, as well as headaches and eye problems such as proptosis, diplopia and visual loss (Photo 1)

Those located in the super-lateral region can grow towards the middle cranial fossa posteriorly or affect the roof of the superior orbit and therefore can cause symptoms more frequently. Their etiological diagnosis is generally difficult as they rarely show characteristic clinical signs that suggest a vascular lesion. Therapeutic management should consist of local excision of the lesion with a margin of healthy bone, and immediate reconstruction of the orbit with autogenous bone grafts to minimize aesthetic and functional deformity.
The objective of this work is to present our clinical and therapeutic experience in a patient with primary intraosseous angioma of the orbit, with special consideration in the diagnostic and therapeutic aspects in a patient who when we first evaluated her, the lesion was already unresectable, being surgery the only therapeutic method with curative criteria.
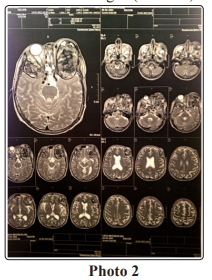
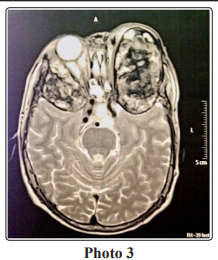
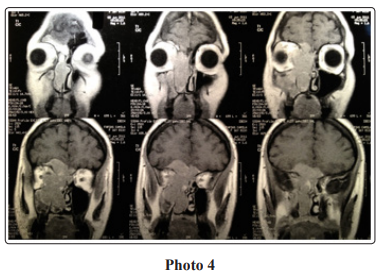
This is a 48-year-old woman who was referred to us for the study of a painless tumor in the right supraorbital region that appeared a year earlier, which had evolved with a slow and progressive increase, causing proptosis in the right eyeball (Photo 1). The patient’s medical history did not refer to a history of interest or previous trauma. There was no ocular, neurological or systemic alterations. The patient presented an initial MRI that showed a zone of bone expansion with a marked periosteal reaction on the lateral rim of the right orbit, which had been reported as chondrosarcoma or metastatic lesion of a primary tumor of unknown origin. (Photos 2, 3 and 4)
The clinical examination revealed a mass of hard consistency, non-displaceable and slightly painful on pressure in the right superior-lateral orbital rim, approximately 4 x 3 cm in size. The overlying skin was also erythematous with an incipient fistulous orifice.
Expansive processes in both orbits, predominantly on the left, of bone origin, which may correspond to different causes.
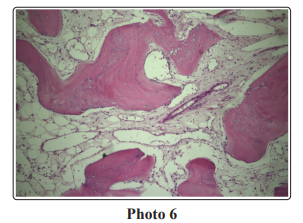
The lesion was accessed through a incision approach, and a biopsy was taken that was reported as compatible with an intraosseous angioma. (Photos 5 and 6)
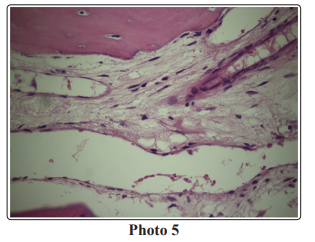
A) Several bone fragments each measuring 0.5cm in diameter.
B) Blood clots that together measure 4cm in diameter.
C) Fibrin hematic clots, collagenized fibrous tissue and bone
structure made up of mostly laminar trabeculae with signs of
superficial apposition separated by adipose marrow with areas
of fibrosis, observing marked edema and numerous dilated
vascular lumens with thin walls lined by endothelium. There
are no signs of atypical infiltration.
D) Fibrin-hematic clots with isolated fragments of fibrous tissue
with marked vascularization.
E) Compatible with Intraosseous Angioma.
Angiomas are classified into three types: cavernous, capillary, and mixed. Most of those diagnosed in the head and neck are of the cavernous type. In our patient, we believe that it is a “capillary” type. The pathogenesis of this neoplasm is unknown. Some consider them as developmental vascular malformations, although previous trauma has also been implicated, a history that was not collected in our case. Intraosseous angiomas are three times more common in women than in men. They are typical of the 4th-5th decade, although they can appear at any age.
The clinical and radiological diagnosis of an intraosseous angioma sometimes poses serious difficulties, as is verified with our patient. Establishing the vascular origin of the injury can be critical, as improper bone biopsy or curettage can lead to severe bleeding. Plain radiography shows a characteristic diagnostic image, generally of bone rarefaction with well-defined margins. Sometimes they can present specific diagnostic patterns (fine striations, honeycomb-like reticulations, sunray images on the bone cortex, etc.), which were not verified in our case. CT is useful to know the location and extent of the neoplasm. MRI shows an increased signal on T1 and T2 images. The soft tissueof the lesion causes increased signal on T1 and blood stagnation and slow flow on T2. However, despite their specific radiological manifestations, most of these neoplasms can only be definitively diagnosed after being studied by biopsy and the specimen studied by a bone pathologist. Preoperative angiography is generally not necessary, since these lesions do not usually have a recognizable blood supply, it was requested in the patient with a minimal contribution to the diagnosis.
The differential diagnosis of slow-growing primary bone lesions in the orbit is very broad, since there are a large number of lesions with clinical and radiographic presentation similar to bone angiomas. These include fibrous dysplasia, aneurysmal bone cysts, giant cell tumors, osteomas, dermoid cysts, meningiomas, metastases, and malignant tumors of the skull base such as chondrosarcoma, multiple myeloma, or osteogenic sarcomas. Surgery, when it can be performed, is the only curative method and should consist of a local excision of the tumor in bloc with a margin of healthy bone when the diagnosis of intraosseous angioma is known pre or intraoperatively.
In this way, resection of a healthy bone margin allows the lesion to be completely excised and operative bleeding to be reduced. Curettage of the injury carries the risk of uncontrollable bleeding. When there is no ocular compromise (proptosis) or aesthetic, some authors recommend observation as an alternative measure. Partial resection with a superficial osteotomy leads to recurrence in a high percentage of cases, although other authors indicate it as a simple technique only to correct the bone deformity. If the diagnosis is uncertain or malignancy is suspected, bone resection should be greater in order to obtain tumor-free margins. If the lesion is located in the supraorbital, a craniotomy with subsequent reconstruction of the bone defect may be necessary. Supraselective embolization in the 24-72 hours prior to surgery and external carotid artery ligation significantly reduces intraoperative bleeding and can be effective in large lesions with rich vascularization.
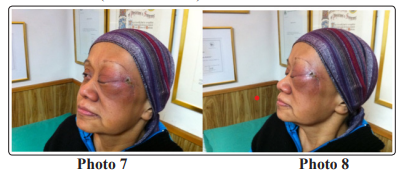
Radiation therapy treatment of these tumors can be used in unresectable cases, since it has been shown to be useful in stopping their growth, as indicated in our patient with a significant decrease in tumor mass. (Photos 7 and 8)
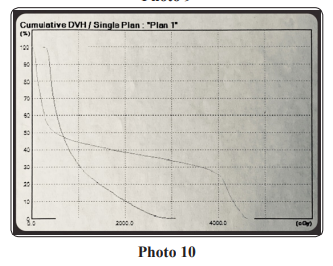
Radiant treatment was indicated according to the three-dimensional irradiation technique formed with a linear electron accelerator, using 6Mev photon radiation and multiple entry gates in different planes; laser localization and computed planning.
The computed planning for three-dimensional shaped field radiotherapy was performed with a three-dimensional computed planning system. MIRS version 4.0. Satellite collimators were made for each radiation gateway. The dose fractionation was done according to the following scheme: (Photos 9 and 10) Daily dose: 250cGy Weekly dose: 1250cGy Total dose: 4250cGy

There is no specific medical treatment for bone angiomas, since biologically they are benign tumors, they do not metastasize or comply with the precepts of neoplasms, on cell division and the “uncontrolled” growth of their cell volume, primarily in an exponential way and then logarithmic, none of that is seen in these tumors, they are biologically benign, but clinically “malignant”, because they invade by contiguity, destroy noble structures, in our patient the tumor destroyed the ocular bony orbit with destruction of the eyeball, and blindness of the eye left.
Corticosteroids, anti-inflammatories, analgesics, etc. are used, with palliative criteria. Chemotherapy is a treatment for cell populations that are proliferating (“proliferation chemotherapy”), add toxicity, with no clinical benefit. It is at this point, where we evaluate the incorporation of an antiangiogenic medication, bevacizumab, a monoclonal antibody, after radiotherapy.
Bevacizumab is a recombinant humanized monoclonal antibody that blocks angiogenesis by inhibiting VEGF-A. Originally, bevacizumab was approved by the US Food and Drug Administration (FDA) for certain metastatic cancers including lung, breast, renal, and brain as a systemic administration. Bevacizumab is an antiangiogenic agent drug capable of suppressing the pro-angiogenic signaling pathway, following activating mutations in the RAS gene. This gain of function mutation promotes angiogenesis. Since this pathway begins extracellularly with VEGF binding its VEGFR receptor, anti-VEGF is used for the treatment of angiosarcoma and Kaposi sarcoma.
Our patient received bevacizumab for 18 months, with a decrease in the tumor mass, and a clear improvement in her quality of life. The encephalocutaneous fistula never closed, which led to infection, sepsis and death of the patient after a year and a half. Our analysis is that bevacizumab is a useful drug in this disease “orphan” of specific drugs and should be used in the first line, in those patients who cannot operate or relapse to surgery (1-16).
