Author(s): <p>Shamima Nasrin Shadia, Sadia Afrin, Ken Yoshimura and Moazzem Hossain*</p>
Antenatal care (ANC) is a care given to pregnant women to timely identify and mitigate pregnancy related problems that can harm mother and/or fetus. Most of the Bangladeshi women present late for ANC. This study aims to determine the time of ANC initiation and the number of visit for ANC among pregnant women attending Filaria & General Hospital between January 2016 and December 2018. The study population had adequate knowledge regarding ANC except for pregnant women who had visited minimum number for ANC. Among 1761 study population, 1268 (72%) had registered for ANC, and 493(28%) had not registered. Out of 1268, 651 (51.34%) had their first ANC within the recommended time (before or at three months), and 617(48.66%) started late initiation of their ANC care. Here, 649 (51.18%) of the study population received more than three visits for ANC.
Antenatal care (ANC) is essential for the wellbeing of the mother and the child. All pregnant women are recommended to go for their first antenatal check-up in the first trimester to identify and manage any medical complication as well as to screen them for any risk factors that may affect the progress and outcome of their pregnancy [1]. This ANC should be provided by a medically trained provider to ensure the health of mother and fetus through early detection of risks in pregnancy, prevention of pregnancy and labor complications and ensures the safe delivery of mother and child to be most effective and there should be regular ANC throughout pregnancy [2,3]. Almost 90% of maternal deaths occur in developing countries where over half million women die each year due to pregnancy and childbirth related causes [4]. For example, Sub-Saharan Africa and Southern Asia accounted for approximately 86% (254 000) of the estimated global maternal deaths in 2017. However, at the same time, between 2000 and 2017, Southern Asia achieved the greatest overall reduction in MMR: a decline of nearly 60% (from MMR of 384 down to 157). The high number of maternal deaths in some areas of the world reflects inequalities in access to quality health services and highlights the gap between the rich and the poor. The MMR in low income countries in 2017 was 462 per 100 000 live births versus 11 per 100 000 live births in high income countries [5]. Studies demonstrating the high levels of maternal mortality in developing countries and research identifying causes of maternal death have repeatedly emphasized the need for prenatal care and the availability of trained personnel to attend to women during labor and delivery [6]. The use of ANC in developing countries is still low compared to developed countries (97%) [7]. In developing countries, women often encounter serious health risks during pregnancy either for themselves (e.g., anemia, edema, and eclampsia) or for their children (e.g., sepsis and pneumonia, birth asphyxia and injuries, tetanus, congenital anomalies and with low birth weight) of the 210 million women who become pregnant each year, 30 million, or about 15%, develop complications, which are fatal in 1.7% of cases [8]. The risk of maternal mortality and morbidity, as well as neonatal deaths can be reduced substantially through regular, proper ANC check-up and delivery under safe and hygienic conditions. In other words, a large majority of these deaths are preventable by providing ANC and assisting child birth via skilled birth attendants [9]. In Bangladesh, 64 percent of women who gave birth in the three years preceding the survey received antenatal care from a medically trained provider, up from 55 percent in 2011.This increase was mainly due to an increase in ANC from skilled birth attendants. Thirty-one percent of women have four or more antenatal care visit during pregnancy, an improvement from about one in every four (26 percent) in 2011 [3]. However, the number is still large.Available information suggests that about 12,000 women in Bangladesh die due to pregnancy-related complications10. Although proper ANC is one of the essential ways to reduce maternal and child morbidity and mortality, many women in developing countries including Bangladesh, do not receive such care [11]. Besides, considering WHO newest ANC guideline, which recommends that each woman attend eight of more routine ANC contacts between conception and birth, the percentage is to be even lower [12,13,14].
Bangladesh has made a significant improvement towards achieving the Millennium Development Goal (MDG) target the 5 of 75% reduction in the MMR between 1990 and 2015 [15]. ANC is potentially one of the most effective health interventions for preventing maternal morbidity and mortality, particularly in places where the general health status of women is poor. The present study highlights the time of initiation of ANC and number of ANC visit among the pregnant women in Savar, Dhaka.
This is a hospital based retrospective study on the antenatal women attending the outpatient department of Obstetrics and Gynae of Failaria & General Hospital with study duration of three years (2016-2018). The study groups include all pregnant women attended in the department of obstetrics and Gynae in Filaria & General Hospital. Descriptive statistics were used to compute percentage and average. The result was presented in a table and figures and expressed as percentage/proportion, mean and average.
Figure1 shows that 1268 (72%) out of 1761 pregnant women registered for ANC in this study. The re meaning 493 (28%) had not registered for ANC. Out of those registered women for ANC, 51.34% (651/1268) had registered in the 1st trimester followed by 31.39% (398/1268) and 17.27% (219/1268) in the 3rd trimester and the 2nd trimester respectively. Hence 617 (48.66%) women started late initiation of their ANC. Figure 2 shows that out of 1268 women, 651(51.34%) had their first ANC within the recommended time (1st trimester). More than half 649 (51.18%) of the study population received more than three antenatal visit and 619(48.82%) respondents received up-to three antenatal visit. Table.1 shows that the majority of the mothers were 20-25 years of age which 750(42.59%), 26-30 years 466 (26.46%), less than 20 years 290 (16.47%) and more than 30 years 255 (14.48%). The reasons given by the individual women for not attending ANC were found to be the absence of illness (being healthy), being too busy, costly, poor quality of services and others.
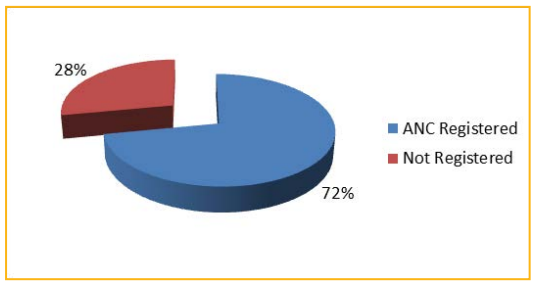
Figure 01: Distribution of study population according to their ANC registration status.
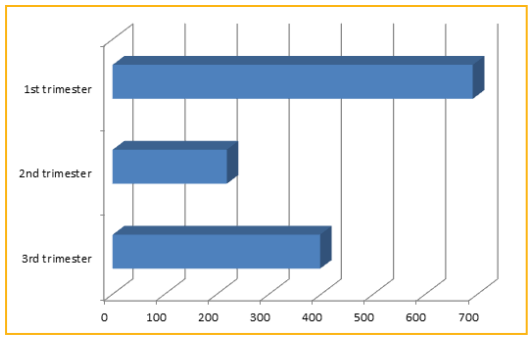
Figure 02: Distribution of registered population according to their time of ANC.
| Age | Number | Percentage (%) |
|---|---|---|
| <20 years | 290 | 16.47 |
| 20-25 years | 750 | 42.59 |
| 26-30 years | 466 | 26.46 |
| >30 years | 255 | 14.48 |
| Total | 1761 | 100 |
Table-1: Distribution of study Population according to age.
In the present study, nearly 70% of respondents belonged to the age group 20-30 years. In a study conducted by Rozliza et al., the majority of the respondents (46.2%) were from the age group 20-29 year [16]. A Study conducted by Shirin S et al., the mean age of women was 33.5±10.4 years [17]. In a study conducted by Alam AY et al., the mean age of women was 29.57±7.1 years [18]. This may be explained by the fact that mothers between this age group, their twenties have enough information on maternal healthcare services. A Similar study conducted by Manas Petal., most of the respondents were more than 25 years old [19]. Out of those registered for ANC, 51.34% (651/1268) had registered in the 1st trimester followed by 31.39% (398/1268) and 17.27% (219/1268) in the 3rd trimester and the 2nd trimester respectively among this respondents. This results are in contrast to Javali who reported 56.5% and 42.9% women under ANC registration in the 1st trimester and the 2nd trimester respectively, and Berhe who reported that 48%, 42.4%, and 1.8% women made their first visit in the 1st trimester, 2nd trimester and 3rd trimester respectively [20,21]. Also, higher rates of the tune of 63.9% were reported by Mumbare [22]. 1268 (72%) out of 1761 pregnant women had registered for antenatal care, the remaining 493 (28%) had not register for antenatal care in our study. This result is higher than the result of Bangladesh Demographic and Health survey 2014 that 64 percent received ANC from a medically trained provider [3]. This is because the pregnant women who had registered for antenatal care were under our follow up and Filaria & General Hospital places in the urban area as urban women are more likely than rural women to have more antenatal visits [23,24].
It is assumed the most of our study’s population had understood the importance of ANC since approximately 72% pregnant women had registered for ANC, and approximately half of them (51.34%) had registered in the 1st trimester. Although the pattern of follow up was found to be in appropriate in most cases, our study’s result was better than other result.
We need to emphasize that early registration should be utilized for the continuation of care and institutional delivery. If there was relatively high ANC utilization among the study population, but half of the mothers 617 (48.66%) started utilizing ANC in their second and third trimester of pregnancy. Considering the late initiation of ANC visit of the study population, the effectiveness of the visit to reduce maternal morbidity and mortality could be hindered.
Since this study was a retrospective descriptive study, we didn’t analyze such as correlation between ANC visit and participant’s background (salary, mediaexposure,place of residence).
