Author(s): Sushila B Ladumor
Adrenal incidentomas are becoming more due to increase in imaging for other reasons. Adrenal myelolipomas are unusual, mainly non-malignant lesion and usually found incidentally during US or other imaging studies done for other indications. It mainly composed of mature adipocytes. Estimated autopsy prevalence of 0.1-0.2% of this unusual lesions. They are usually seen in adults and may complicated by hemorrhage. There is no gender predilection
Clinical History: 25 years old gentleman admitted to urology,
presented to ED with right flank pain He has history of sleeve
gastrectomy 3 months ago, previous weight was 120 kg, and He
lost 25 kg since surgery.
Denied any headache/palpitations/sweating
No symptoms suggestive of Cushing syndrome
No history of hypertension
No family history of hormonal disorders or malignancy
Imaging: CT Urinary tract to R/O stone and obstruction: Unenhanced Urinary tract CT:
Two tiny right renal stone Tiny right vesico-ureteric stone with mild proximal hydrouretero neprosis .
Incidental note of a large well-defined retroperitoneal lesion in the hepatorenal space measuring 11.7 x 13.6 x 14.8 cm in maximum TR, AP and CC dimensions respectively. The lesion showing heterogeneous density predominantly of fatty density with tiny calcific foci representing right adrenal myelolipoma, other possibility could be large exophytic right renal angiomyolipoma. The right kidney is displaced inferiorly. Right adrenal gland cannot be seen separately. Left kidney and adrenal gland appears unremarkable. Surrounding fat is clear with no stranding or free fluid. Evidence of previous gastric sleeve surgery.
MRI with IV gadolinium for better evaluation and characterization: Re-demonstration of a well-defined large mixed intensity lesion mainly composed of fatty component showing areas if signal drop in opposed phase compared to in-phase as well as in T1 fat sat in the right retroperitoneal suprarenal region measuring approximately 13 x 13 x 15 cm in its AP, transverse and CC dimensions respectively. It is mostly non-enhancing but contains small patchy areas of post-contrast enhancement. The right adrenal gland is not seen separately from the mass, which suggests adrenal origin. Unremarkable left adrenal gland and left kidney. The right kidney is compressed and displaced inferiorly by the right suprarenal mass, no imaging features to suggest exophytic renal angiomyolipoma. Small amount of right perinephric free fluid and mild prominence of the pelvicalyceal system. The liver, spleen, pancreas and gall bladder appears unremarkable. Imaging features are keeping with right adrenal myelolipoma.
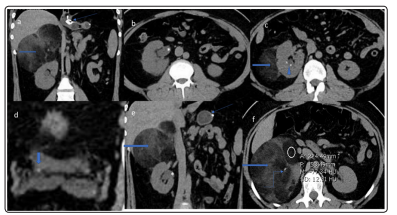
Figure 1: Unenhanced Urinary tract CT:Incidental note of welldefined retroperitoneal lesion in the hepatorenal space (transversearrow in a,c,d &e)) measuring 11.7 x 13.6 x 14.8 cm in maximum TR, AP and CC dimensions respectively. The lesion showing heterogeneous density predominantly of fat (measures in image f) with tiny calcific foci (curved arrow in f). The right kidney is displaced inferiorly. Right adrenal gland cannot be seen separately. Surrounding fat is clear with no stranding or free fluid. Two tiny right renal stone (Triangle in c). Tiny right vesico-ureteric stone (vertical arrow in d). Proximal hydro nephrosis (Asterisk in b & e). Evidence of previous gastric sleeve surgery (Thin arrow in a & e). Incidental note of welldefined retroperitoneal lesion in the hepatorenal space (transverse
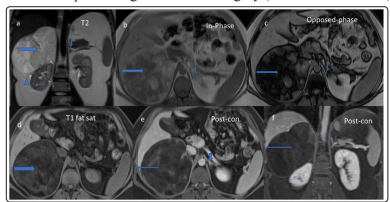
Figure 2: MRI with and without IV gadolinium: Redemonstration of a well-defined large mixed intensity lesion mainly composed of fatty component showing areas if signal drop in opposed phase compared to in-phase as well as in T1 fat sat in the right retroperitoneal suprarenal region (transverse arrow), measuring approximately 13 x 13 x 15 cm in its AP, transverse and CC dimensions respectively. It is mostly non-enhancing but contains small patchy areas of post contrast enhancement. The right adrenal gland is not seen separately from the mass, which suggests adrenal origin. Unremarkable left adrenal gland (vertical arrow). The right kidney is compressed and displaced inferiorly by the right suprarenal mass (Thin transverse arrow in a & f). Small amount of right perinephric free fluid (Triangle in a) and mild prominence of the pelvicalyceal system (image not shown).
Majority of fat containing lesions of the adrenals are benign. It is crucial to identify properly their imaging features, complications that will help in management plan as to leave the lesion, for follow-up or surgical resection. Fatty adrenal masses are usually asymptomatic, can cause symptoms when large, complicated with hemorrhage or very rarely malignant transformation. Usually inactive hormonally, often benign, such as myelolipomas, lipomas, angiomyolipomas, or mature teratomas, and are rarely malignant, such as liposarcomas [2,3,4]. Clinical symptoms vary, usually asymptomatic and discovered incidentally. When it is large it causes pressure symptoms, if it bleeds patient present with acute pain and also present with pain and pressure symptoms if it get large and rarely malignant transformation.
Myelolipoma manifests in four distinct clinicopathologic patterns:
1. Isolated adrenal myelolipoma,
2. Adrenal myelolipoma with hemorrhage
3. Extraadrenal myelolipoma
4. Myelolipoma associated with other adrenal disease.
In imaging(1,2,3,&4) due to its fatty components usually it is hyperechoic similar to retro peritoneal fat / heterogeneous echogenicity due to its typically non uniform architecture and rarely it can missed if US done for other indication or patient is obese (As US is operator dependent). In CT it is seen as hypodense due to predominant fatty component and density is fatty. Enhancement usually minimal in its myelo components. MRI is not indicated frequently as CT Is sufficicine to make diagnosis.
Rarely if patient complaints of increase in size and pain as well as it becomes heterogeneous by US and CT compared to previous exam with increase in size MRI can be helpful to characterize better in view of areas of diffusion restriction, early enhancement as well as readily detect hemorrhage which is seen as T1 hyper intense areas. Also fat seen easily by fat sat and dual phase imaging. Adrenal myelolipomas typically do not demonstrate avid FDG uptake and it is generally lower than that of the liver background. If adenomatous and hematopoietic elements present rarely it can show an increased FDG uptake. If the mass is large and predominantly fatty it is nearly impossible to detect at plain radiography
It is benign tumor histologically and have very rarely malignant potential [1,2]. If imaging features are diagnostic and the lesion is small, no treatment is required (Left alone lesion).
In cases where imaging findings are indeterminate/worrisome, percutaneous biopsy can be recommended. In case of larger lesions with pressure symptoms or where hemorrhage has occurred surgical excision is required, it can be laparoscopic or robotic. No recurrence is observed in case of complete resection.
Fat containing lesions of the adrenals are mostly benign. Crosssectional imaging is helpful in making a pre-operative diagnosis. The diagnosis is usually made by various imaging techniques, in particular CT. The fundamental characteristics indicating the necessity of surgical intervention are required when patient presented with symptoms, acute pain as well as volume of the mass (>5 cm), and the increase in size and symptoms of the tumor as shown in two consecutive imaging studies.
