Author(s): Marzieh Saeidi* and Abdolkarim Karimi
Background: Fear-avoidance beliefs (FAB) are related to disability, postural stability, and chronicity of low back pain. The aim of this study is to investigate the impact of specific training for FAB on postural stability, disability, pain, abdominal and back muscle endurance, and FAB in patients with non-specific chronic low back pain (NCLBP).
Methods: In this queasy experimental study, 51 subjects (27 females and 24 males) with NCLBP were evaluated. Pain intensity, FAB and disability were measured using questionnaires and Postural stability was measured using force plate. Abdominal and back muscle endurance were measured respectively by sit up and Sorensen tests. All the tests were repeated one week and one month after a short-term specific training for FAB. Mixed model repeated measure test was used to compare variables before and after intervention and to evaluate the relation of changes in FAB and pain intensity with changes in parameter of postural stability.
Results: After the intervention, pain intensity, FAB score, and disability score decreased significantly, the time of sit up, Sorensen and single leg stance tests increased significantly. Center of pressure (COP) excursion and velocity decreased significantly but they were not related to FAB significantly.
Conclusion: Specific training for FAB resulted in decreasing pain intensity, FAB and disability scores and improved postural stability as well as increasing the time of sit up, Sorensen and single leg stance tests in patients with CLBP.
The trend of changes in pain intensity and FAB (physical activity subscale) were related to the trend of changes in center of pressure displacement and velocity
Low back pain (LBP) is one of the most common health problems which affect 60% to 80% of adults at some time during their lives About 85% of patients with back pain, are classified as nonspecific chronic low back pain [1-3]. Although most of the time, LBP is a self-limiting disorder and a majority of these patients will improve rapidly, half of them has a long history of multiple episodes and in a small group of them (about10%), pain will become chronic [4-8]. This group of patients allocate about 80% of costs to themselves [9]. Consequently, LBP is a major public health problem with an immense socioeconomic burden in most developed and developing countries. Investigations on patients with acute and sub-acute low back pain indicated that several factors influence on chronicity of LBP such as psychological disorders, job dissatisfaction, existence of radicular pain, previous history of LBP and high level of disability [6, 10-12]. Psychosocial factors such as fear avoidance beliefs (FAB) and attitudes, fear of movement, stress, depression, job satisfaction, self-esteem and self-respect have impacts on patients with chronic low back pain (CLBP) [13-14].
Fear-avoidance believes have been hypothesized as the most important psychosocial factor in predicting disability and work time loss among patients with CLBP [15]. The cognitive-behavior concept of developing acute pain in to chronic situation, is likely to be fear-avoidance behavior at early stage. Lethem explain in a model why some individuals with acute pain develop chronic pain while others recover [4,16]. This model states that the patient’;s fear of pain, and subsequent avoidance behavior, are defined according to the association between sensory and emotional components of pain, so that, the patients believes and fears of increasing symptoms and unpleasant feeling during activities lead to unhelpful ways of
managing LBP, including avoidance behaviors, activity restriction and depression. These behaviors in turn activate sedentary lifestyle and inactivity which causes situation to be more problematic. In addition, inappropriate diagnosis will direct the therapists and physicians to use a wrong treatment approach when there is no clinical indication for it. Although biomechanical factors such as muscle endurance, strength and flexibility, neurophysiological factors and spinal stability should be mentioned as well [17- 19]. Therefore, it is important for the physicians and therapists to evaluated the patients exactly from both biomechanical and psychosocial aspects and adopt an appropriate strategy accordingly in managing the patients.
On the other hand, several studies have shown that postural control is impaired in patients with CLBP have [20-21]. Also according to the investigations, postural control is influenced by co-existing factors including age, pain, fear of pain, adoption of an alternate movement strategy and poor muscular function [22-27]. Many studies have assessed the relationship of either impairment or psychosocial factors with disability and pain, but regarding to biopsycosocial model for treatment of CLBP and different cultural background which could be a factor for effectiveness of treatment strategies in these group of patients, there is not clear that which strategy could be the best way of improving psychosocial aspects in patients with NSCLBP [28-31].
The aim of this study is to investigate the impact of specific training for FAB on postural stability, disability, pain, abdominal and back muscle endurance, and FAB in patients with NCLBP.
This study may help finding a simple method of screening in patients with CLBP to prevent the interventions which are not suitable for these patients. It may also help improving postural stability via decreasing pain related fear and correcting pain related behaviors of these patients.
In this queasy experimental study, 51 subjects (27 females and 24 males) with NCLBP were evaluated. The subjects were referred from some private and public clinics and hospitals in Isfahan during 6 months.
Patients with CLBP (more than 3months), aged between19- 65-year-old were included to this study. Patients with current pregnancy, signs of spinal cord injury, history of lumbar spine or any major surgery during last year, history of osteoporosis or spinal fracture, epilepsy, addiction and any signs of neurologic disease were excluded [32].
Eligible subjects received an informed consent to be included in the current study. Then they were invited to the place of performing the project and were asked to fill the following questionnaires respectively (demographic, Fear-Avoidance Belief Questionnaire (FABQ), Visual Analog Scale (VAS) and Oswestry Disability Index (ODI)) [33-35]. After that they were asked to stand quietly on a force plate for 90 seconds and then on the dominant leg for 30 seconds in order to measure parameters of postural stability [36].
Demographics: Basic demographic information will be collected using a questionnaire. These include gender, age, height, weight, education levels, smoking situation, working environment (manual, desk bound, retired, unemployed), pain medication (yes or no) [37].
History of Disease: Onset of pain, cause of pain, past history of episode, increase frequency episode, pain region, aggravating factors and relieving factors (sitting, standing, walking, others) will be asked from the participants using a check list [37].
Fear Avoidance Beliefs: Iranian version of Waddel’;s FearAvoidance Belief Questionnaire (FABQ) was used to evaluate psychosocial status of the participants; higher numbers indicating increased levels of fear-avoidance believes [33]. The questionnaire is divided into subscales for physical activity (FABQ-PA) and work (FABQ-W). The FABQ consists of 16 items, which assesses patient believes regarding the effect of physical activity and work on their LBP. Each item is a statement on the degree of patients' agreement on a 7-point Likert scale (0 = completely disagree, 6 = completely agree). In this study only FABQ-PA were used which consists of 4 questions (maximum score = 24) because some participants would not have any job, this method has been used before in another study [38]. A higher score indicates higher level of Fear Avoidance Beliefs.
Pain: The Visual Analog Scale (VAS) was used to measure pain Intensity of the patients. That is a horizontal 100 millimeters line which is marked in both sides: one side 0(no pain) and the other side 100(maximum pain). Participants were asked to indicate a point on this line according to their pain intensity [34].
Disability: An Iranian version of the original Oswestry Disability Index (ODI) was used to evaluate condition-specific disability and pain [35]. This score has 10 questions about pain and painrelated disability in activities of daily life and social participation. Each question has 6 different response alternatives. The sum is calculated and presented as a percentage, where 0 represents no pain and disability and 50 represents the worst possible pain and disability.
Parameters of Postural Stability: A force plate (Kistler 50*60 made in Switzerland) will be used to measure parameters of postural control. The examinations were performed in the musculoskeletal research laboratory of the school of rehabilitation sciences within Isfahan University of medical sciences. The participants were asked to stand quietly on the force plate for 90 seconds and then 30 seconds in single leg stance on dominant leg. One minute rest were considered between trials [36]. The COP measures included frequency, velocity and displacement of COP in sagittal and frontal plan by the software (Qualizer, sampling frequency:120 HZ, cut off frequency:10 HZ,3 trials).
Abdominal Strength Endurance: Strength endurance of the abdominal muscles were measured with the patient in the supine position, knees bent at a 90° angle and with unsupported feet flat at the surface with straight arms, a slow curl-up were performed until the finger tips just touched the proximal border of each patella. The time of maintaining this position by each subject was measured Performance with jerks or heels rise from the surface will not be accepted (maximum 240 seconds was considered for this test) [39].
Back Muscle Endurance (Biering-Sorensen test): Isometric endurance of trunk extensors were evaluated by measuring how many seconds (maximum 240 seconds) the patient was able to maintain the unsupported upper part of the body horizontal, when placed prone on a couch with legs fixed and the arms across the trunk [40].
Single-Limb Stance: Each patient stood two meter in front of a checked curtain so that one of the longitudinal lines of the curtain was in line with the spine. The contra-lateral leg was lifted about 60° of flexion at the hip. The patient was asked to stand with the spine as vertical as possible and with the arms hanging down. The time was measured and the test was stopped if the spine deviated from its original vertical position, or if the subject did a compensatory movement made by the contra-lateral leg or the arms (maximum 240 seconds was considered for this test) [41].
Intervention: All patients were educated by a physiotherapist in a 60 minutes session on addressing their fear which was based on the information of "The Back Book" which was prepared by 5 researchers who are the most influential researchers on back pain [42].
All data were collected one week and 3 weeks after intervention (60 minutes educational class) by repeated all the tests and filling the questionnaires.
Ethical issues: All subjects will read and sign a written informed consent. The cost of transportation of the participants will be paid by the researcher. This study will be approved by a local bio-ethics committee in Isfahan University of medical sciences.
Statistical Analysis: Mixed model repeated measure test was used to compare variables before and after intervention & to evaluate the relation of changes in FAB and pain intensity with changes in parameter of postural control with adjusting for covariate variables age, Body Mass Index (BMI) and physical activity. All data were analyzed by SPSS software (ver:15) at level of P< 0.05.
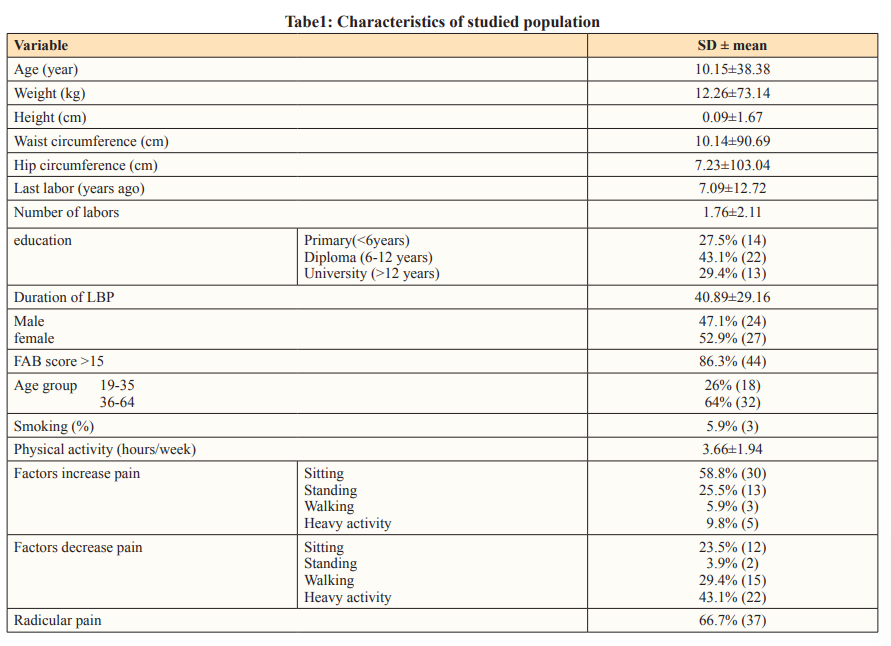
Data distribution was normal according to kolmograph Smirnov test (P< 0.05). Table 1 shows characteristics of studied population. FAB (physical activity and job subscales), pain intensity and disability decreased one week and 4 weeks after the intervention significantly (p<0.05) (Table2). Time of single leg stance, Sorensen and sit up tests were increased significantly one week and 4 weeks after intervention (p<0.05) (Table2).
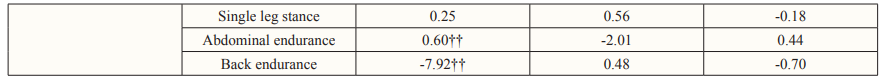
According to the table 2, copx copy, vcopx and vcopy decreased one week and 4 weeks after intervention in both anteroposterior (AP) and mediolateral (ML) plans and both position (quiet standing and unilateral standing) significantly (p<0.001). Although fcopx and fcopy decreased after intervention, the changes were not significantly (Table2).

Cop: center of pressure displacement, v: velocity, f: frequency, X: mediolateral plan, y: anteroposterior plan (vcopx: velocity of center of pressure displacement in mediolateral plan) FAB: fear avoidance beliefs
Trend of changes in pain intensity was related to trend of changes in fcopx in queit standing position and trend of changes in vcopx, vcopy, copx, endurance of back and abdominal muscles (Sorenson and sit up tests) in unilateral standing significantly (p<0.05) (Table3).
Trend of changes in FAB (physical activity subscale) was related to trend of changes in copx, copy, vcopx, vcopy and fcopy just in unilateral standing significantly (p<0.05) (Table3).
Trend of changes in FAB (job subscale) was related to trend of changes in disability and endurance of back muscles in unilateral standing but in quiet standing it was related to just back muscle endurance significantly (p<0.05) (Table3).
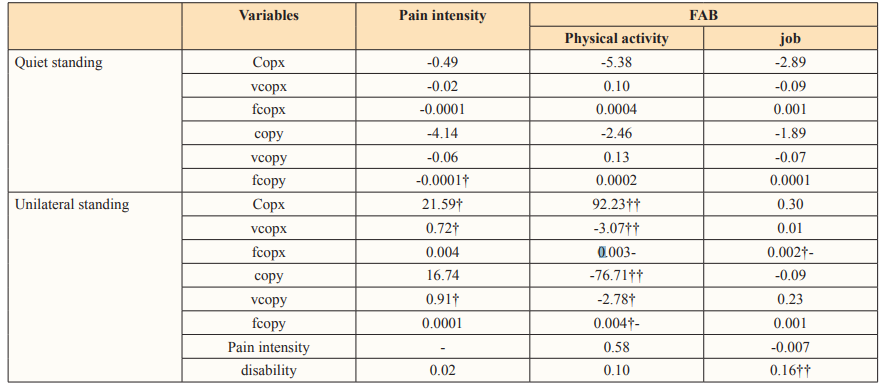
Cop: center of pressure displacement, v: velocity, f: frequency, X: mediolateral plan, y: anterioposterior plan (vcopx: velocity of cenyer of pressure displacement in mediolateral plan) FAB: fear avoidance beliefs, †p<0.05, ‡p<0.01
The finding of the present study was improving pain intensity, FAB (physical activity and job subscales), disability, back and abdominal muscle endurance and parameters of postural stability (center of pressure displacement, velocity and frequency). In addition, trend of changes in pain intensity and FAB (physical activity subscale) were related to the trend of changes in center of pressure displacement and velocity in unilateral standing in both AP and ML plans. These results were in contrary to the results of the study by Maribo, in which postural stability was not related to FAB significantly [43]. The possible reasons for this different can be include: different in methodology of these two studies, so that Maribo evaluated the association between FAB and postural stability after 14 weeks without any intervention while in present study a short-term specific education on FAB were accomplished and the time for evaluating the changes and association was 1 and 4 weeks, so both the intervention and shorter time can explain the difference between the results. In the other word, maybe in absence of any intervention, the time was not enough for change of parameters of postural stability in the study by Maribo or maybe in our study after a longer time, the association could be powerless due to reversal changes in FAB or parameters of postural stability. Another reason, could be due to use different instruments for measuring COP (in our study a fixed force platform was used but in the other study a movable force plate was used), also according to the methodological standards we used 3 trials for each condition and 90 second for quiet standing but in the other study they perform each condition two times and measured cop displacement for 60 seconds.
Another study has shown that there is not any relationship between FAB and postural stability; however, function of abdominal muscles and the reaction time of these muscles were evaluated to study the postural stability [20]. Furthermore they have studied the postural stability in a walking which is a dynamic posture while in our study, postural stability was checking in quiet and unilateral standing which are static postures.
We couldn't find any relationship between FAB and disability at present study while several investigations have shown a positive association between these two parameters. In some studies, it revealed that the higher levels of pain intensity were related to the FAB score, A new study showed that disability is related to duration of LBP, higher level of pain intensity, FAB and stability (velocity in the forward direction) [44-46]. So the lower level of disability of the studied population in our study comparing to the other studies can explain this controversy. Of course, at present study disability was just related to the job subscale of FAB, even after adjusting for covariate variables such as age, physical activity, body mass index and back and abdominal muscle endurance.
In our study FAB was related to the back-muscle endurance but not to the abdominal muscle endurance and the time of maintaining stability during single leg stance test. People who experience pain-related fear will avoid activities they associate with increased risk for pain or (re)injury. As such, pain-related fear should have a negative effect on the results of performance testing [47-48]. The relationship between pain related fear and performance appeared stronger in studies where patients were observed under strictly controlled conditions, and weaker in studies where patients were observed in a less controlled environment [49-50]. The relation between pain and pain related fear and functional performance is weak or non-existent in patients with CLBP [37]. A hospital casecontrol study, compared the psychological aspects between patients with low-back pain [51]. According to their results, patients' levels of depression and anxiety were related to occupational background whereas high level of job stress can lead to the psychological problems such as anxiety and depression. In addition, longer duration of LBP was accompanied by higher levels of anxiety and depression. So, identifying potentially modifiable determinants of disability in patients with LBP provides an opportunity to expand strategies of controlling socioeconomic problems [51].
Several studies have shown that postural control parameters change in CLBP however, there is controversy on relationship between pain and postural control parameters [21, 52-57]. In recent years, it has become evident that muscle pain can interfere with motor control strategies and different patterns of interaction are seen during rest, static contractions, and dynamic conditions [52]. In CLBP patients, postural stability under challenging conditions such as prolonged standing is maintained by an increased sway in anterior-posterior direction. This alteration in postural strategy may provide a dysfunction of the peripheral proprioceptive system or the central integration of proprioceptive information [58]. These findings point to possible neurophysiologic mechanisms that could help explaining why fear of pain is a robust predictor of pain-related disability [59]. Our findings support these studies, because FAB was related to the parameters of postural stability just in unilateral standing without any relationship in quiet standing. Being a more difficult condition for maintaining postural stability in unilateral standing comparing to the quiet standing can explain this idea.
Several studies have shown the impacts of different education methods such as back school, short term education, cognitive interventions and specific training for FAB in order to improving psychosocial aspects in patients with CLBP [60-67]. According to a systematic review and European guideline there is controversy on effectiveness of these methods for patients with CLBP [68-69]. However, there is strong evidence on effectiveness of behavior therapy for improving disability in these patients [67-69]. Also a few studies indicated that influence of behavior therapy is less than short term education [60]. On the other hand, some investigations have revealed that using the back book which is written by a group of investigators in order to improving patients' attitudes and beliefs on FAB and having more physical activity was effective [66]. In another study a short-term education with supplying this book and accompanying with telephonic fallow up were more effective in improving the patients' attitudes [67]. Another study indicated that relaxation and cognitive therapy improved the pain intensity and pain related fear [70]. In our study, a short-term specific education in related to FAB based on the back book and providing this book for the patients reduced pain intensity, FAB and disability and increased parameters of postural stability in unilateral and quiet standing as well as back and abdominal muscle endurance.
According to the relationship between FAB and postural stability and improving pain, disability, FAB, postural stability and back and abdominal muscle endurance after a short-term education based on the back book which is a specific training for FAB, could be recommended for management pf patients with NSCLBP, since this method is not expensive and time consuming.
This study has some limitations like having a short term follow up and absence of control group.
We recommend executing investigations with stronger methodology such as considering a control group, evaluating according to sex and age groups and job background of the patients as well as longer follow up.
This study supported by musculoskeletal research laboratory of school of rehabilitation in Isfahan University of Medical Sciences.
