Author(s): <p>Sujata Singhi</p>
Cancer is a disease that has a substantial influence on both morbidity and mortality, as well as quality of life. In addition to the constant endeavor to create better medicines with the objective of extending survival, complementary therapies that may improve the physical and mental well-being of cancer patients are gaining popularity.
Stress poses the greatest harm to the immune system, which is severely impaired in cancer patients. Stress prevents the body from working in the proper rhythms. Sound helps the brain calm down and enter a peaceful, sleeping state, which is beneficial for cancer patients. Vibration may be utilized in sound healing to massage particular places on the body, therefore strengthening systems such as digestion and liver function.
Sound therapy employs both audible and inaudible sounds and vibrations to have a therapeutic impact by shifting brain waves into alpha or theta states, so activating the body’s restorative pathways. These pathways promote cellular repair. During sound healing treatments, vibrations flow through tissues, massaging cells and facilitating brain alterations. This is known as brain wave entrainment (BWE),2 a technique that employs rhythmic stimuli to modify the brain’s state.
Brain waves may be synchronized (trained) using rhythm, vibration, and frequency to slow down the typical beta state (waking consciousness) and enter an alpha (relaxed awareness) or theta (meditative) state. Some clients may even attain a delta (sleep and healing) state. BWE has been explored and used since the late 1800s, but many physicians, scientists, and practitioners are now becoming aware of its presence.
Vibrational sound therapy can be applied “constructively” or “destructively.” Because sound has the inherent ability to control all matter, vibrations may be utilized to organize (or disorganize) molecules and reorganize cells
Certified Sound practitioners like the one’s qualified at the Divine Soul Sound Institute of Sound Therapies and Spiritual Sciences employ constructive sound to restore the brain to a normal, unexcited condition. This allows the immune system to relax, inflammation and swelling to recede, and the brain to be better equipped for a good, healthier reaction to stress and sickness.
The most productive sound is perceived. When used appropriately, vibrations can gently stimulate individual cells (20-2,000 hertz range).
Sound therapy has always been employed, particularly in palliative care. Certain sound therapies have been shown to have positive effects on anxiety, sadness, pain, and exhaustion in cancer patients.
This study looks at the impact of a pre-recorded self-administered 4-week sound intervention on physical and emotional well-being in cancer patients. In addition to the self-rated quality of life, sleep quality, pain, exhaustion, and fear of illness progression were also measured in a standardized manner.
Two self-applied sound therapies, which patients may do without the assistance of a therapist, were employed for this purpose and compared in terms of patient reaction.
This study was conducted in the outpatient department. It was planned as a prospective, randomized exploratory experiment. Because of the nature of the technique, blinding was not feasible.
This trial included patients with cancer who were over 18 and had been treated. They were randomly assigned to a self-applied sound intervention. Individual sound activity was used as a stratification criterion (Figure. 1, flowchart).

Standardized questionnaires were used to gather data at both the baseline and 4-week intervals. The timing and period of the sound intervention were recorded in a patient diary. After two weeks, a visit was conducted to evaluate compliance based on the logbook, detect any emotional stress produced by the intervention, and answer study participants? queries.
Gender, age, career, height, and weight (to determine BMI) were collected. In addition, research participants were asked if they were engaged.
Patients were asked to fill up self-assessment questionnaires about pain, tiredness, quality of life, worry about tumor growth, and sleep quality.
Patients were randomly assigned to one of two sound interventions: one is monochord and passive sound intervention (using an MP3 player and headphones to listen).
As noted by a patient logbook, all trial patients self-applied both therapies for approximately 15 minutes in the evening before bedtime throughout a four-week period. Patients in the active group were given an introduction to playing to achieve effective vibration transmission, the trial participants were asked to remain supine throughout the intervention and lay the monochord.
It was demonstrated that the instrument can be played at various volumes and speeds. They were requested to document the instrument’s tuning on a daily basis. During a follow-up appointment after two weeks, the instrument’s tune was checked and modified as needed. and >10 are frequently observed in chronic sleep disorders. The patients were then classified into three categories. Moving to a higher category relates to worsening or to a lower category to response.
The major goal of this exploratory experiment was to describe the percentage of patients who improved in at least one of the five survey instruments/questionnaires delivered between baseline and final evaluation (referred to as “response” in the following).
To generate an accurate estimate of the proportion of respondents, a sample size calculation was performed. Patients were randomized in a 1:1 ratio using the following stratification criteria:
The quantitative variables were evaluated using the parameters of statistical analysis (N, arithmetic mean, standard deviation, median, minimum, and maximum), whereas the qualitative variables were evaluated using frequency tables. The categorical variables were analyzed using contingency tables. To compare two sound therapies, the χ2 test was employed. If the χ2 test conditions were not satisfied, Fisher’s exact test was applied.
The survey tools (PSQI, QLQ-C30, VAS for pain and tiredness, and FoP) were evaluated descriptively for both measurement time and intervention group. In addition, differences in baseline values were computed and descriptively analyzed. Furthermore, each survey instrument/questionnaire was categorized using the following answer criteria:
PSQI: The questionnaire has 19 items and 7 subscales, with values ranging from 0 to 21. Scores of 0-5 are typically regarded as acceptable sleep quality, 6-10 indicate severe sleeping issues,Standardized questionnaires were used to gather data at both the baseline and 4-week intervals. The timing and period of the sound intervention were recorded in a patient diary. After two weeks, a visit was conducted to evaluate compliance based on the logbook, detect any emotional stress produced by the intervention, and answer study participants’ queries.
QLQ-C30: The questionnaire includes 30 items and 15 subscales in three categories (global condition, functional levels, and symptom scales). The scores for each subscale range from 0 to 100.
A higher score on global health status or functional measures indicates a higher quality of life or level of functioning. However, in the symptom subscale, a higher score indicates a greater number of symptoms or issues. A change of +10 points indicates an improvement in QoL/level of functioning or an increase in symptoms, whereas a change of -10 points indicates a worsening QoL/level of functioning or a reduction in symptoms.
VAS: The VAS runs from 0 to 10. A difference up to > −1 conforms to deteriorating or > +1 to the response.
FoP: the questionnaire is comprised of 43 questions including 5 subscales (affective responses, partnership/family, occupation, losing of autonomy, and coping with anxiety). A difference up to > −14 corresponds to deteriorating or > +14 to the response.
The total response was calculated using separate scales and characterized as an improvement in at least one dimension while the other scores remained constant or improved between the baseline and final evaluation.
The research comprised 73 patients, including 29 (40%) males and 44 (60%) females. Patients were randomly assigned to passive sound intervention (n = 39, 53%).
The median age was 52.0 years (range: 21–79). The research participants were of normal weight, with a mean BMI of 25.2 ± 5.5 kg/ m2. The great majority of patients (41, 56%) were employed, while 18 (25%) were retired, six (8%) were jobless or househusband/ wife, and five (7%) worked for themselves. Only one individual (2%) was a student, and two research participants (3%) did not provide information about their occupation. 14 participants (19%) said that they were engaged (Table 1).

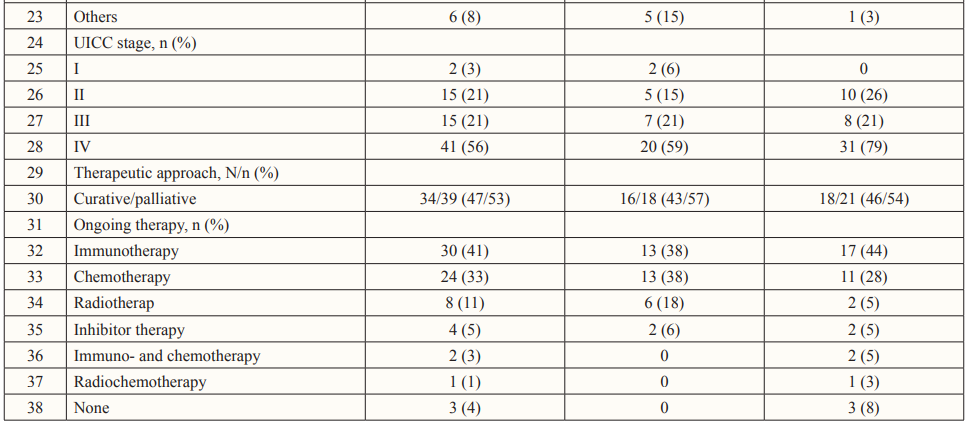
68 of 73 (94%) participants completed the patient diary. The sound intervention was carried out for a median of 26 days throughout a four-week period (range 5-28). In all, 57 patients (78%) incorporated the intervention into their regular routine for at least 24 days. In the active group, 28 study participants (82%) documented the intervention for at least 24 days, whereas 29 (74%) were in the passive intervention group (Table 1).
In terms of the primary goal, all patients in the group responded and improved in at least one dimension while not deteriorating in any other: n = 15 (39%) versus n = 9 (27%).
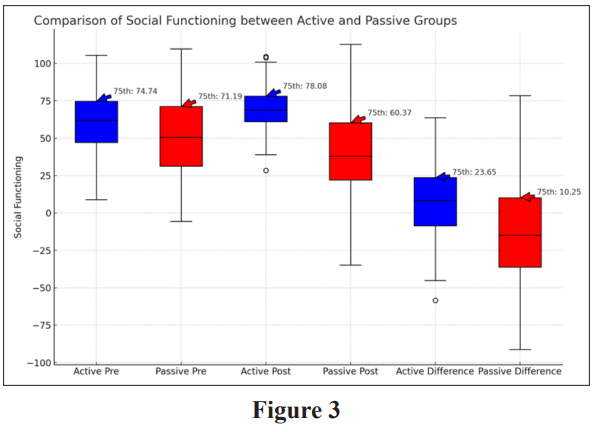
The individual scales and total reaction differed substantially between the active and passive groups, with the exception of VAS weariness (p = 0.049). Furthermore, the passive group had a tendency towards better QLQ-C30 response: n = 12 (31%) versus n = 3 (9%), p = 0.06 (Table 2).

This is an individual depiction of the total reaction to active sound intervention (left) and passive sound intervention (right). Changes in the various domains are color-coded as follows: deterioration (red), no change (yellow), and improvement (green). Missing values are greyed out.

The current prospective randomized exploratory trial assessed patient responses to a four-week, self-administered sound intervention. The effects on many aspects of physical and emotional well-being, including quality of life, sleep quality, pain, exhaustion, and affective reactions, were evaluated. The key findings of these studies are summarized as follows:
The chosen sound reduced stress more effectively in patients with increased stress levels leading to recovery and handling the effects of the medications effectively. Further research is needed to determine the extent to which sound as Medicine affects patients’ reactions in conjunction with relaxation techniques to deliver better outcomes.
In this exploratory randomized experiment, a four-week sound intervention was found to be practicable and safe in oncology outpatients. Passive sound intervention improved patient-reported outcomes in terms of social functioning, weariness, and emotional responses. The predefined total reaction rate was statistically greater after the passive sound intervention. However, when active sound interventions were induced, many emotional releases were noticed and positive outcomes and recovery noticed.
One can read the book, “Power of Sound”-Dr. Sujata Singhi which includes many real life experiences of cancer patients who have been healed completely when Dr. Sujata Singhi used “Sound as Medicine” on them [1-4].
