Author(s): Ftoon Kedwan
Background: This is an experiment report on Health Information Systems’ (HIS) integration project. It reports a successful implementation experience of HIS integration with the pharmaceutical Pyxis system that is used for medication dispensing. The Information Technology (IT) department in King Khalid Eye Specialist Hospital (KKESH) in the Kingdom of Saudi Arabia led this project to its final successful deployment. Rhapsody Engine successful adoption in the integration process helped KKESH achieve their productivity goals by improving hospital’s staff daily duties and clinical workflow. It also eliminated the system’s errors and alerting notifications.
Objective: This experience paper discusses three main questions: What is the power of systems integration? What are the systems’ integration standards? What are the main key performance indicators for IT related projects? It also discusses the implemented solutions that solved many potential problems that could be encountered by similar big organizations such as the KKESH. Several drawbacks of having isolated internal systems will be discussed. Similarly, many difficulties encountered during the integration process were demonstrated in detail. Henceforth, this experiment report can be considered as a road map for medical organizations with similar size and limitations should they consider integrating their internal systems for better health care management and productivity. Method: The adopted solution was implementing the Rhapsody integration engine to integrate HIS with Pyxis machines. To solve the systems’ compatibility issues, the ITD staff used a mapper tool to convert the query results from an XML format to the HL7 format. A shared folder was created between the Rhapsody Engine and the Pyxis system to read all the ADT messages seamlessly. Results: The hospital reported successful piloting implementation of this project. Some of the key project findings from this project experience are demonstrated and documented at the end of the paper, which would be of potential use to an organization who undergoes a similar experience. Conclusion: This project reported a successful systems’ integration project to set an example of an ever developing and prospering healthcare facility.
King Khalid Eye Specialist Hospital (KKESH) is a specialized hospital working under the Saudi Ministry of Health (MOH) [1]. It involves multiple systems as the Health Information System (HIS) Pharmaceutical System and Pyxis System an automated medication dispensing system [2-4]. Due to these systems&rsquo: decentralization and isolation in separate working environments, the hospital decided to move towards digitizing and automating all clinical workflow processes for a smooth patient care assurance. This systemized transformation is to reduce data duplication and save numerous data entry time and effort [5].
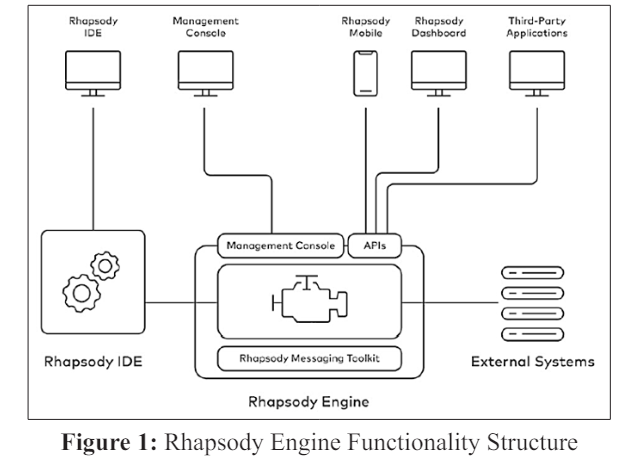
Systems integration is the systems&rsquo: ability to exchange data and information across the organization seamlessly. The Information Technology Department (ITD) embraced Rhapsody Engine as a means of system integration mechanism [6]. Rhapsody is a healthcare systems integration engine that allows for timely information sharing following the Rhapsody engine functionality structure illustrated in Fig. 1 [7]. Rhapsody ensures data transfer reliability and accuracy, provides powerful and flexible database connectivity, and facilitates data extraction and insertion into custom databases. Such flexibility allows for personalized application utilities and report development for almost all clinical purposes. Besides, it supports many communications standard protocols such as Health Level Seven International (HL7) Extensible Markup Language (XML) and web services [8,9]. The objective of this experiment report is to share the ITD personnel technical experience with Rhapsody engine system integration project, and to give an example of a method of productivity improvement using a health informatics solution. In the next section, section 2, the environment where this project took place will be briefly described. This section is thought to help other organizations reading this experience paper to consider the difference/similarity of technical environments for fair comparison of project outcomes. Then, the main project drives are explained under section 2.2 followed by the implications of those drives, which make up the main reason of holding this project in the first place. After that, the implemtnation steps of the solution (Rhapsody engine) us demonstrated step by step. Section 3 discusses the results of the integration project implementation and discusses some key findings and lessons learned. The last section, section 4, concludes the experiment reporting and points at one implementation limitation that is considered for future work.
KKESH is an ophthalmology hospital operated by the MOH.
The hospital provides a kingdom-wide ophthalmic care through
different programs, such as the outreach and research initiatives
[10]. As a leading hospital serving over 140,560 outpatients
and 10,888 inpatients each year, KKESH embraces the mission
of providing the best ophthalmic care for the entire middle
eastern region, putting patient care on its top priorities. KKESH
also dedicates lots of efforts to increase the knowledge of the
ophthalmic diseases by providing public awareness programs and
trainings whenever feasible.
KKESH&rsquo:s ITD provides the required technical services to all
hospital&rsquo:s staff to help maintain their working goals, increase
hospital&rsquo:s productivity, and enhance its global medical excellency
[11,12]. The ITD staff are trying continuously to promote new
technologies in KKESH by supporting exploratory and innovative
applications, hoping to reach the level of making KKESH a
paperless hospital by computerizing all of the internal processes
and procedures.
There are certain evidences that lead to the necessity of adopting an integrated HIS such as the following institutional key facts:
KKESH started an initiative with a local vendor to fix the system&rsquo:s integration problem between the internal HIS and the pharmaceutical system [3]. However, the HIS integration project failed, and the vendor did not meet all the agreed-upon requirements before the end of the contract. Thus, HIS system integration project was postponed based on the instructions of the higher management until further notice.
Since the local vendor left the project without handing over the project documentations, the system reached a level of hopelessness with tons of system bugs and issues. The HIS system kept generating ADT (Admit, Discharge, and Transfer) error messages [13]. One of those messages is the Admission Message (ADT-02) that included all the patients&rsquo: information except for the most important piece of data, the Medical Record Number (MRN). Instead, the system mistakenly replaced it with a random internal number. Another HIS error was creating ADT-02 only for patients who have admission appointments, and missed all patients admitted through the emergency department and the one-day surgery wards.
Moreover, the Transfer Message (ADT08) was generated correctly including the patients&rsquo: MRN. However, the Pyxis users were still stuck because the transfer transaction in Pyxis machines depend on the admission phase completeness. While the ADT-02 included a random internal number (possibly another patient&rsquo:s identifier). The Pyxis machines could not map between the two messages and update the patient&rsquo:s information chart accordingly. Similarly, Discharge Messages (ADT03) were created by the HIS, but it did not contain any data. Hence, it became clear that the vendor has completely failed to integrate the two systems, and the hospitals workflow was at risk.
Failure of the HIS-Pyxis systems integration project affected the inpatient pharmacy processes significantly. It added extra workload on both pharmacists and nurses as they had to operate the Pyxis system manually. In addition, it led to a substantial financial loss because KKESH had to purchase six other Pyxis machines for each floor, since they could not ?talk? with each other [14,15].
In regard to the ADT02 mistake of not including the patient&rsquo:s MRN, pharmacists could not use the Pyxis machines to fill patients&rsquo: medications due to missing patient&rsquo:s identification number, the MRN. Hence, to be able to dispense patients&rsquo: medications, nurses had to validate patient&rsquo:s information with the HIS, and then add the patient&rsquo:s MRN manually to patients&rsquo: files in the Pyxis system. This Manual updating and processing of patients&rsquo: identification details and critical medical information may potentially affect patient&rsquo:s privacy and safety and increase medication errors, risking patients&rsquo: lives.
The ADT03 problem caused the entire discharged patients the trouble of appearing in the Pyxis system as if they were still admitted. The Pyxis system had the discharged patients as well as the newly admitted patients, all in the same location in the system. This patients&rsquo: status confusion mixed up patients&rsquo: medication lists in the Pyxis system. This is considered to be a fatal mistake as patients could be prescribed other patients&rsquo: medications. To avoid this disastrous mistake, the nurses had to inform the pharmacists to discharge patients manually away from the use of the Pyxis system. All those troubles led the hospital to depend heavily on paper-based processes moving away from the KKESH&rsquo:s technical mission and vision.
The problem was first addressed by initiating a resolution committee of the pharmacy director and ITD professionals. Their obvious goal was to fix the HIS system integration problem. The ITD had to search for alternative solutions to be built from scratch after failure to get in touch with the previous local vendor. After thorough searching and investigation, the ITD director agreed to implement the Rhapsody integration engine as a suitable solution to integrate HIS with Pyxis machines.
The ITD started the integration project by purchasing a Rhapsody Engine license, and then training the ITD staff with its functionality and maintenance. After that, the ITD staff started developing a custom-made query design to extract all needed information for the ADT messages. Soon after, three foundation routes, for the ADT actions, were created as a first step of building the system integration process. After that, Rhapsody engine configuration settings were addressed to run the three routes&rsquo: queries sequentially every 10 minutes.
To solve the systems&rsquo: compatibility issues, the ITD staff used a mapper tool to convert the query results from an XML format to the HL7 format by mapping each field in the XML to the correct position in the HL7 message. The mapping process was done successfully for all system fields including MRN, Patient&rsquo:s Name, Floor, Room, Bed, and the admitting physician name. However, the dates formats got confused between the birth and the admission dates in both the Rhapsody Engine and the Pyxis system. They failed to be mapped, thus, ITD staff had to write a Java code that reads HL7 messages including dates and then convert the dates into the Pyxis format.
As a last coding step, ITD staff created a shared folder between the Rhapsody Engine and the Pyxis system to read all the ADT messages seamlessly. After completing the systems&rsquo: integration implementation and testing phases from the technical side, the user testing and approval phase was started. Hence, the ITD, pharmacists and clinical units&rsquo: mangers agreed to implement the Rhapsody engine solution starting in two floors only as a pilot deployment in the first month [16]. Piloting the project deployment among the floors and departments helped the ITD staff and the Pyxis users to easily adapt to the new change and evaluate the integration process suitability and efficiency.
During the piloting phase, Pyxis users suffered from two issues. First, patients&rsquo: transfer messages were not being created until the end of the patient transfer process in the HIS. Subsequently, when the patient physically transfers to another floor, room or bed, the patient&rsquo:s information in Pyxis will not be updated with the patient&rsquo:s new location unless the nurses complete the transfer transaction in the HIS system instantly. Since this is a human part issue, and not a system error, the only solution was that the floor units&rsquo: mangers and the nursing administrators must support the transfer transaction completion by ensuring the nurses transfer the patients in the HIS on time.
The second problem was regarding the patients&rsquo: discharge process. The pharmacists found that some medications were dispensed for patients whom were already discharged from the HIS, but they still appear in the Pyxis system. Such a case could risk patients health and safety by taking the wrong medication, or not taking it at all because it does not show up in the Pyxis terminal interface. After comprehensive investigations, ITD staff found that patients were not discharged on time by the nurses. Thus, on the next day, the admission clerk discharged the patient from the HIS using the manual date entry function to complete the discharge transaction on the actual date and time. However, Rhapsody engine programmed to work with the clock, and it never goes back to read actions from the past. Therefore, the Rhapsody engine did not read that discharge transaction and did not create an ADT03 message. Thus, the discharged patient was still appearing as admitted in the Pyxis system. This type of discrepancies is contradicted with the American Health Information Management Association (AHIMA) and its data quality management characteristics, in addition to KKESH polices [17]. ITD arranged a meeting with the departments of pharmacy, nursing and the admission office to clarify the issue and the consequences of delaying patients&rsquo: discharge system transactions. Again, this appeared to be a human mistake and the system was not changed or amended in this regard.
After successful piloting implementation on two floors, the hospital decided to activate Pyxis machines on the rest of KKESH floors. In the final stage, the pharmacists got trained on monitoring the Rhapsody engine performance and system status notifications, in addition to searching for messages using Rhapsody management console [18].
Upon successful implementation of the Rhapsody engine to integrate KKESH HIS and the pharmaceutical system (Pyxis), both systems were able to share and exchange patients&rsquo: data smoothly. Errors such as missing MRNs or discharge dates were not a problem anymore. Accurate admission time/date were enforced by the integration of both systems. Manual work was not necessary as well, since whatever data needed by either systems can be easily fetched by the other system electronically. This section also discusses the questions serving as the main objectives of this paper, which are as follows:
Integrated healthcare systems have a direct impact on having fewer medical practical and procedural errors, better adherence to AHIMA and MOH standards, better patient satisfaction, easier and faster workflow for healthcare workers, the overall quality of healthcare services provided, and most importantly, maintaining the integrity and accessibility of healthcare services.
A standard is a set of procedural controls that when enforced, a successful implementation is assured [19]. The ISO/IEC TS 24748-6:2016 (International Organization for Standardization / International Electrotechnical Commission Technical Specifications) specifies the standardized lifecycle for Systems and software integration engineering projects. Those standards were closely monitored and observed throughout the implementation of the current medical systems integration project of HIS and Pyxis systems. The standards specify the steps to follow from the start until the successful project closure. Hence, the KKESH integration project started with carefully planning for the integration project by discussing all integration engine options and choosing the most scalable and reliable option, Rhapsody engine. Then, identifying the stakeholders and engaging ?most of? them in the implementation rounds later on. After that, putting forward an implementation workflow design and architecture and following it closely as the project proceeds. Lastly, testing the integrated systems functionality and correctness of systems outcome. Systems maintenance is an ongoing procedure that ensures the smooth continuity of system&rsquo:s provision of services.
KPI metrics measure the level of successfulness on reaching the objectives of any implemented project [20]. Continuously evaluating KPIs assures that the project is running according to the standardized plan and in compliance with the organization&rsquo:s strategic goals. High KPI values are an indication of a timely, risk-free, and reduced ratios of project failure. KKESH integration project of HIS and Pyxis had the following main KPIs:
1. Improving healthcare workers productivity, performance, and satisfaction.
2. Eliminating the errors continuously aroused by the system, e.g., ADT-02 and ADT08.
3. Reducing the additional ITD costs, e.g., buying several Pyxis machines for each hospital floor.
4. Finishing the project on time and within budget.
Fortunately, the integration project has concluded with satisfactory levels of the four main KPIs. While those are the main project KPIs, they affect other secondary goals, such as maintaining patients&rsquo: safety by reducing the system errors, reducing employee turn-over by improving employee&rsquo:s satisfaction, etc. Among many other practical and personal lessons learned from this project implementation experience [21]. KKESH valued three main findings the most:
In this project, ITD staff did not involve the admission office personnel until the very last stage when problems requested their involvement. It is believed that involving all potential end-users in any ITD related projects is essential for the project implementation successfulness and completeness.
ITD staff must be intuitive, creative and persistent. These are the three main characteristics of any ITD individual. In this project, Pyxis users were totally relying on the HIS vendors for its functionality, which turned to be not the best approach. However, with the ITD&rsquo:s productive efforts, together with the higher management support, the Pyxis system is up and running.
Selecting vendors to implement a huge ITD project is a very critical step. That is because selecting the wrong vendor solely based on a cheaper quotation or due to personal preference might cause numerous financial and organizational complications. KKESH learned to select a vendor with a history of a minimum of three similar successfully implemented projects in similar environments as of KKESH hospital.
KKESH hospital believes in the power of technology in providing a high level of patients care and service. Hence, ITD received a lot of support and encouragement to implement the most recent technologies available, such as the Rhapsody engine, to achieve KKESH productivity goals. This project reported a successful systems&rsquo: integration project to set an example of an ever developing and prospering healthcare facility. However, the integration project suffers from one limitation. The system runs on a real time bases instead of batch processing. Hence, in some emergency cases when medications need to be dispensed immediately after admitting the patient in the system, the Pyxis system will not allow medications dispensing to any particular patient before a period of 10 minutes delay, starting from after the patient is admitted in the HIS system. Solving this problem is still in progress as a future work.
There are no conflicts of interest to report.
