Author(s): Luiz Eduardo Imbelloni, Andre Augusto de Araujo, Jaime Weslei Sakamoto, Eduardo Piccinini Viana, Wagner Ferreira Filho, Marcos Kayu Mori, Geraldo Borges de Morais Filho
In 2010, we started implementing the ACERTO project in a hospital in the northeast of the Brazilian Public Health (SUS) after five weeks with all stakeholders involved in the departments of Anesthesiology, Orthopedics, Geriatrics, Nutrition, Nursing, Physiotherapy, Psychology and Social Service. In the same way as in other hospitals, the implementation of fast track surgery was not obtained by all departments and all health professionals. The use of ACERTO protocol with clinical measures of accelerating patient recovery decreased length of stay, the number of suspensions of surgery, the need for ICU, the use of vesical catheter, the time of fasting, the time of oral food reintroduction, high earlier and faster return to family life, working as humanization of treatment to the elderly. Analgesia in all patients was obtained with local anesthetics through different plexus blocks with neurostimulator and no patient used spinal opioids. In medicine the vast majority is terribly attached to their arguments and no one is willing to give in to new truths. Dreaming costs nothing and the implementation of the ACERTO Project will cost nothing to any institution.
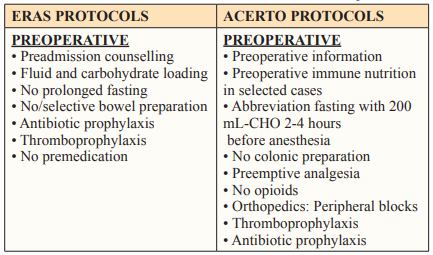
The ACERTO project (ACEleração da Recuperação TOtal Pós-operatória) is a program created in 2005 at the University Hospital Júlio Muller and was based on an existing European work ERAS (Enhanced Recovery after Surgery) to develop the ideas presented in the 90s by Professor Henrik Kehlet, a Danish colorectal surgeon, from Copenhagen University. In order to improve the quality of care for surgical patients and decrease the cost of such care, several groups have proposed to standardize the perioperative care approach. The implementation of this project to accelerate postoperative recovery in elderly patients with hip and hip fractures in Brazilian Public Health System (SUS) hospital has as main objectives reducing the length of hospital hospitalization, surgical complications and increased patient satisfaction after surgery. The implementation resulted in the publication of 15 scientific articles in several journals, all with patients over 60 years of femur and hip fracture. There are some differences between the two projects (Table 1).
Population aging is a worldwide phenomenon. The increase in longevity represents a victory for humanity, as it attests yet another overcoming of man in the face of obstacles to his survival. However, aging has brought with it numerous other issues, mainly in relation to health care. According to the World Health Organization (WHO), an elderly person is every individual aged 60 or over. Brazil has more than 28 million people in this age group, a number that represents 13% of the country’s population [1].
Studies show that in the last 30 years the quality of life of elderly Brazilians has not only improved, but healthy longevity has increased. The denominations Third Age and Fourth Age overlap with the labels old age-initial/old-young and old age advanced/ old-old, introduced in 1974 [2,3]. She was a pioneer in proposing the idea that there are multiple ages in old age.
The fourth age brings a level of biocultural incompleteness, vulnerability and unpredictability that differentiates it from the third age (initial old age), which is marked by more positive aspects. Old people are at the limit of their functional capacity, which results in restrictions on interventions and social policy. Further efforts are needed to deal with the challenges represented by the growing number of old-aged people in the populations and the increasing prevalence of frailty and psychological mortality represented by loss of identity, psychological autonomy and sense of control. This increase in the elderly population requires adjustments in the health requirements for this group of patients both in medical research and in health policy [4,5].
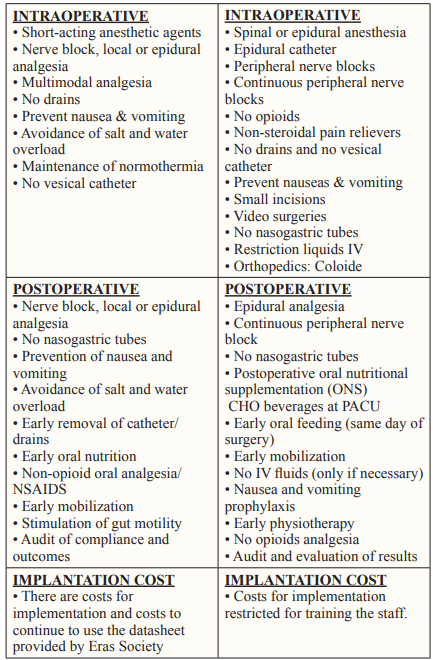
The elderly population tends to grow in Brazil in the coming decades, as shown by the IBGE’s Population Projection, updated in 2018 (Figure 1).
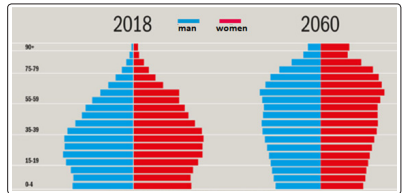
Figure 1: Brazilian Population Released In 2018 by Ibge and Projection For 2060
According to the survey, in 2043, a quarter of the population should be over 60 years old, while the proportion of young people up to 14 years will be only 16.3% [1]. A phenomenon that accompanies population aging is the feminization of old age, that is, the highest proportion of women than men in the elderly population, especially at older ages advanced. In a cross-sectional, population-based study, with individuals over 60 years old, 57.6% were female [6].
Osteoporosis represents a public health problem, since it increases the risk of femur fracture in the elderly, a condition with high morbidity and mortality and high costs. The main treatment for femoral fracture is surgery and the longer you are bedridden the greater the chances of having complications such as infection, deep vein thrombosis and pulmonary embolism and finally death. In a review article published in 2004, the mortality rate was 5.5% during hospitalization, varying between 4.7% in the 1st month and 10.8% in the 6th month. Advanced age, number of comorbidities, male gender and presence of cognitive deficits were identified as the main factors related to the greater mortality [7].
The first unit for geriatric orthopedic rehabilitation was created in the United Kingdom in the early 1950s. And in 1974, Dr. Devas an English orthopedic surgeon coined the term “Geriatric Orthopedics” [8]. Geriatric people are not just elderly adults. Your bone and soft tissue quality is quite different from the quality common in young orthopedic patients.
There is evidence that the recovery from surgery can be reduced and accelerated convalescence. This approach became known as “fast track surgery”, and incorporates not only surgeons but also anesthesiologists, nurses, nutritionists, psychologists, physiotherapists, and social worker as active participants in the care of the patient. In Medicine, a happy coincidence means that a scientific discovery was obtained unexpectedly. The ACERTO project is a program that aims to accelerate postoperative recovery supported by multimodal protocols and evidence-based medicine (EBM). The EBM translates into the practice of medicine in a context in which clinical experience is integrated with the ability to critically analyze and apply scientific information in a rational way in order to improve the quality of patient care [9].
Thus, an event that has just been observed as the ACERTO project may go unnoticed by the lack of preparation or lack of knowledge of health professionals. In 2005, a multidisciplinary program was implemented involving general surgery, anesthesia, nutrition, nursing and evidence-based practice based physiotherapy andthe results showed that the project it is feasible within our reality, improving morbidity and decreasing the length of hospital stay in surgery general [10].
Surgical treatment of femoral fractures in patients older than 60 years admitted to the SUS hospital are only performed with the patient being referred to the Intensive Care Unit (ICU), passage of a bladder catheter and analgesia with spinal opioid. In order to implement the ACERTO Project, during six months, 105 patients with femur fractures were operated on after meeting the inclusion criteria [11]. The inclusion criteria were: normal blood volume, no pre-existing neurological disease, no coagulation disorders, no infection at the puncture site, which was not agitated, had no mental confusion and/or delirium, who did not use bladder catheters, with hemoglobin level > 10 g% and who was not in the ICU. The use of a postoperative acceleration project reduced the fasting time, the length of hospital stay and provided faster hospital discharge in elderly patients with femoral fractures. From May to August 2011, 83 subjects 60 years and older admitted consecutively with a femoral neck or intertrochanteric fracture attributable to a conventional conduct of anesthesiology service and from September to December 2012, 85 subjects with the same type of fracture undergoing new protocol of perioperative care (ACERTO) (Table 2).
The results showed that the implementation of the project reduced the time spent in the hospital before surgery, the time of preoperative fasting, the number of surgeries canceled, the length of stay in the PACU, the abbreviation of the postoperative fast still in the PACU and the reintroduction of the meal in the ward. All 85 patients were able to be discharged on the first morning after surgery. In this study, costs were not carried out; however.
In another study with 400 patients, there was a reduction from 21.38% to 100% in all parameters evaluated, and it can be inferred that the implementation of the ACERTO project, SUS system costs decreased in elderly patients with fractures of the femur [12,13].
Prospectively analyzing 26 patients (4 men and 22 women) aged 100 years with hip fracture, the average hospital stay until the day of surgery was 4.76 ± 2.61 days, and two patients were transferred to the ICU for surgical problems [14]. All 26 patients after the implantation of the project were ready for discharge in the first post-operative day. Regional anesthetic techniques (spinal anesthesia and lumbar plexus block) were used in all patients for post-operative analgesia.
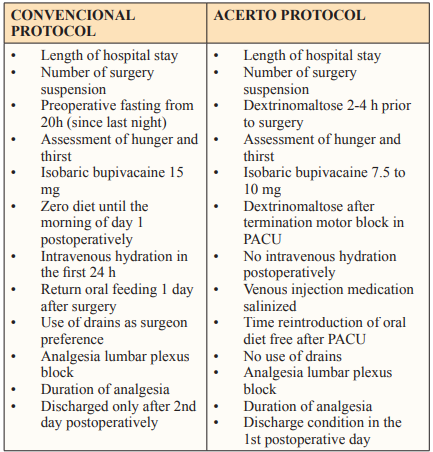
By implementing the ACERTO project managed by an anesthetist, orthopedist, geriatrician, nutrition service, nursing and social service and few tests for these patients, it was possible to optimize the perioperative period, reducing the need for ICU, drains, hospital stay and costs, in the 15 articles published (Table 3). Data taken from the various published references shows the incidence of variables before and after implementation of the ACERTO project and decrease in percentage (Table 4) [11-14,23,24,26,32].

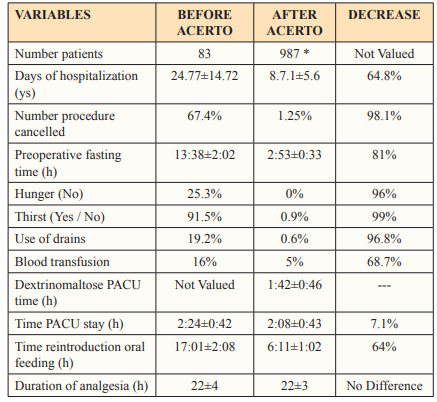
* Data from the following References: [11-14,23,24,26,32].
According to the World Health Organization (WHO), an elderly person is every individual aged 60 or over. Brazil has more than 28 million people in this age group, a number that represents 13% of the country’s population [1]. The trend is that, in 2031, the number of elderly people exceeds the number of children and adolescents in Brazil [1]. The number of elderly people aged 100 years and over reaches 11,422 people. Of this total, 7,950 are women and 3,472 are men [1].
Geriatric individuals may have medical problems and comorbidities such as diabetes mellitus, hypertension, vascular disorder, cancer or dementia. The safety margin of certain drugs and their incidence of adverse effects, reactions may be different from those of the general population. Musculoskeletal injuries and diseases in the elderly are major challenges for orthopedists and anesthesiologists. Osteoporosis, often found in the elderly, and should be carefully considered a treatable condition. The skin and soft tissues of the elderly are generally fragile and less tolerant of surgical trauma. Fractures in the elderly (≥ 60 years) have a major public health impact and take a heavy social and economic toll. According to demographic changes in the general population, the incidence of hip fractures will also increase in the coming years [15].
Studying from 2008 to 2012 in SUS patients, 181 thousand cases of femur fracture were cataloged, with an incidence of 67.5% female, resulting in a woman / man ratio of 1.67/1 [16]. Given the increasing number of elderly people in the world, the management of these patients will become increasingly important in the future. Perioperative care is also becoming more complex, with an increasing number of patients with a number of specific drugs for simultaneous diseases and for the prevention of thromboembolism. Multidisciplinary projects must take all of these data into account and design perioperative treatment with acceleration of the entire process from admission to discharge. The anesthesiologist must take care of the analgesia since admission and if possible at home with continuous plexus block techniques.
Elderly patients often do not show typical signs and symptoms of an illness, thus making an early and accurate diagnosis more difficult. In addition, these patients often suffer from substantial comorbidity, which further complicates treatment. Elderly patients are generally more vulnerable to the adverse effects of anesthesia and surgery, due to the combination of declining organ function, changes in pharmacokinetics and pharmacodynamic of drugs and observed comorbidities. Elderly hip fracture is associated with increased morbidity, functional decline and use of nursing in home services, as well as a higher mortality rate.
Femur and hip fracture patients represent a clinical management challenge; they are an increasingly large group of elderly people predominantly with a variety of medical comorbidities under varying levels of control. In addition, they are facing surgical correction of the fracture and, often, difficult post-operative rehabilitation. In a study with 24,062 patients aged over 60 years and a proximal femur fracture, it ranged from 5.52% in one month to 24.94% in two years after the fracture [7]. The annual cost of treating the hip fracture is very high. The introduction of orthopedic-hospitalist comanagement service has reduced significantly the time of surgery and length of hospital stay for 1.6 days and this way more patients reaching the operating room. Two types of hip fractures are responsible for the vast majority of cases. A rate of 45% of hip fractures is intracapsular, involving the head and neck of the femur; another 45% are intertrochanteric fractures. Both fractures usually involve low-energy trauma, such as falling from a chair or tripping over a rug. Intertrochanteric and subtrochanteric fractures represent the remaining 10% and are extracapsular [17,18]. The main goals of treatment are to stabilize the fracture, decrease pain and restore the level of function before the fracture. Surgery is the preferred treatment because it provides stable fixation, facilitating the return to walking activity and decreasing the risk of complications. Surgery is also associated with a shorter hospital stay, improving rehabilitation and recovery. The ACERTO project provides for all these steps in femoral fracture surgeries in the elderly. Surgical stabilization should be performed as soon as possible, ideally within 48 hours.
Hip fractures have serious repercussions in elderly individuals. The vast majority of hip fractures are easily diagnosed based on clinical findings and standard radiographs. If the radiograph is not sufficient, magnetic resonance imaging is indicated to confirm the diagnosis. This problem is of great relevance because of high morbidity and mortality, high rate of disability after treatment, and increasing costs to society with low treatment-related results. The primary goal of orthopedic treatment for these elderly patients should be to return to function, although some patients with severe comorbidities, the treatment objective can be a return to independent life that is, independent walking, dressing, and going to the bathroom and eat. For most patients with hip fractures, this goal is best accomplished with surgery followed by early mobilization.
The time to perform the surgery is essential for recovery. In general, the ideal is that the surgery be performed within 24 to 48 hours after admission [19]. In SUS hospitals, this time is practically impossible to achieve. The implementation of the ACERTO Protocol managed to reduce the hospitalization time from 24 days to 11 days [12]. Decision regarding the time to perform the surgery must be an interaction between geriatrician, anesthetist, surgeon, nutrition and nursing service and the hospital board. Improving adherence requires a continuous and dynamic process. The implementation of the ACERTO protocol was adhered to byall Services; however anesthesiologists were the biggest obstacle to implantation in all patients [13].
In a retrospective study during one year of observation with 340 patients with hip fractures, they were compared with patients treated operatively and nonoperatively [20]. The study concludes that hip fracture patients who were treated non-operatively have a higher risk of mortality at both one and two years after fracture. Overall mortality rates at one (14.4%) and two years (24.4%) in operated patients were significantly lower when compared to patients not operated on at both one (29.8%) and two years (45.6%) after fracture.
The type of surgery is based on the characteristics of the fracture, a decision of the surgeon and depends on the material existing in SUS hospitals. An economic analysis of hip fracture in the older adults is required in order to better understand the current scenario of the problem and to develop appropriate coping strategies, especially in hospitals where they serve the Brazilian Public Health System. Analyze the incremental cost-utility ratio of the treatment of hip fracture in elderly patients, concluded that the early surgery strategy proved to be dominant, since presented lower cost and better results in relation to the late one. The direct medical cost was significantly increased statistically significant among patients operated late. In-hospital mortality was higher in the 16.9% late surgery group versus 7.4% operated early. The cost was significantly lower in early surgery R$ 9,854.34 (US$ 4,387.17) against R$ 26,754.56 (US$ 11,911.03) in late surgery, life adjusted for quality, respectively [21]. The average time between trauma and surgery was 9.4 days, with an average hospitalization of 13.4 days.
Most people with hip fractures are elderly and are treated surgically, which requires anesthesia. Surgery to correct the fracture can be performed with general anesthesia, epidural, spinal anesthesia or a combination of these techniques. Spinal anesthesia is often used for surgical treatment of hip fractures in elderly patients, and is often preferred for its effectiveness, rapid onset of action, minimal effect on mental status, reduced blood loss and protection against thromboembolism complications [11-13]. In the elderly, there is a high prevalence of clinical problems and reduced mechanisms of physiological compensation.
Elderly individuals with hip fractures have a series of comorbidities that are associated with a great increase in the risk of morbidity and mortality. The choice of the type of anesthesia should be made after the joint decision of the geriatrician, anesthesiologist and the orthopedic surgeon. And to this day, the ideal technique has not yet been identified.
In a recent meta-analysis over a six-year period with twenty retrospective observational and three prospective randomized controlled studies with 413,999 patients, assessing the influence of anesthetic technique for hip fracture surgery showed that neuraxial anesthesia is associated with a reduced in-hospital mortality and length of hospitalization [22]. However, type of anesthesia did not influence the 30-day mortality. Regarding the secondary outcomes the incidence of myocardial infarction and respiratory failure was significant lower in the neuraxial anesthesia group.
In all 15 articles published with ACERTO project, the anesthesia performed was always spinal anesthesia with lumbosacral plexus block for analgesia before the procedure for mobilization or at the end of surgery for analgesia only [11-14,23-33]. In the case of blockage only for analgesia, subanesthetic doses of dextroketamine were administered to perform spinal anesthesia [34].
Spinal anesthesia is associated with the risk of hypotension due to the rapid extension of sympathetic block, hindering cardiovascular adaptation and compromising the blood supply to several vital organs. Lower dose of local anesthetic reduces the severity and incidence of hypotension during spinal anesthesia [35]. Studying low doses (7.5 mg) of isobaric bupivacaine provided adequate spinal anesthesia for surgical treatment of hip fractures in the elderly compared to the total dose (15 mg) of the same solution, causing dramatically less hypotension, eliminating the need for the use of vasopressors and with less need for the use of a bladder catheter. This low dose provided less head dispersion, less motor block and shorter PACU stay [23].
Standard practice of nothing by mouth has been applied for decades in patients undergoing procedures elective surgical procedures. However, recent data indicate that a liberal fasting regime does not increase the risk for these patients. High carbohydrate drink (CHO) significantly reduces preoperative discomfort without affect gastric content. Reduce preoperative fasting time with a carbohydrate-rich solution up to two hours before the operation, such as early postoperative feeding brings numerous benefits to the patient [36,37].
Prospective, randomized clinical trial conducted in a Brazilian Public Health hospital, with 100 patients undergoing hip fracture surgery with a group of NPO and another receiving 200 ml CHO, showed that the fasting time decreased from approximately 14 hours to 3 hours [26]. The results of this study clearly show that in the elderly inpatients, the liberal use of CHO is an easy and practical way to increase patient comfort and satisfaction with anesthesia care.
A recent review of studies showed that the abbreviation of preoperative fasting with a drink enriched with carbohydrates or carbohydrates and glutamine proved to be effective in the care of surgical patients, optimizing the recovery of the postoperative period. Abbreviation of preoperative fasting time with ingestion of maltodextrin solution is beneficial to pulmonary function and preserves dominant handgrip strength [38,39].
Due to the use of 200 ml of CHO 2 to 4 hours before the procedure, restrictive administration of lactated Ringer was used in parallel with 500 ml of 6% hydroxyethyl starch 130 / 0.4 in 0.9% sodium chloride in all patients in all 15 articles, resulting in decreased hypotension. All patients received an average of 1,200 ml of Ringer with Lactate during the surgical procedure.
Likewise, all patients received CHO in the PACU immediately after the end of the motor block of the lower limbs of the spinal anesthesia with a stay in the PACU of less than 2 hours. After ingesting 200 ml CHO and not observing nausea or vomiting, patients were referred to the ward. Transoperative hydration averaged 1,200 Ringer’s lactate and 500 ml 6% hydroxyethyl starch 130/0.4 in 0.9% sodium chloride in all patients. The implementation of the ACERTO project allowed the removal of venous hydration and the reintroduction of oral feeding in the infirmary lasting less than 6:30 hours. Finally, all the patients were released from hospital the day after the surgical procedure [12,13].
Hip fractures in the elderly are among the most common reasons for hospitalization. Upon admission to SUS hospitals, elderlyindividuals with hip fractures are generally malnourished. Nutritional status increases the risk of complications postoperative and mortality in patients with fracture hip. In Brazil, the IBRANUTRI study identified that malnutrition was present in 48.1% of patients and the severe malnutrition in 12.6% of patients, among patients, hospitalized by the Brazilian Public Health System. Staying during hospitalization may deteriorate due to inadequate food intake associated with surgical trauma. Malnutrition prevalence in acute hip fracture varies substantially depending on the assessment measure applied [40-42].
The early identification of the nutritional status of the elderly with hip fractures and their immediate treatment are vital to reduce hospital stay, complications and hospital costs. The incidence of malnutrition and progression in this patient population is attributed to cachexia, chronic diseases and social problems for protein energy intake [40]. Malnutrition diagnoses immediately upon hospitalization of patients with hip fracture needs to be treated as a disease not without consequence, and food needs considered a fundamental medication in these patients. In a recent ESPEN guideline regarding nutrition in surgery, he indicated that early oral feeding is the best way of nutrition in surgical patients [43,44]. This oral feeding avoids any type of nutritional therapy, especially in the post-operative period of major surgery. The guideline showed that malnutrition and malnutrition are risk factors for postoperative complications. And early enteral feeding is especially relevant for any surgical patient at nutritional risk, especially for those undergoing high gastrointestinal surgery. The ESPEN guideline should be applied to elderly orthopedic patients since the entire gastrointestinal tract is free without problems, from the mouth to the anus. This applied to all 15 articles after implantation of the ACERTO project in a SUS hospital.
In all 15 published articles based on the ACERTO conduct, the fasting time with CHO substance was below 3 hours, the use of CHO in the PACU below 2 hours and the reintroduction of food in the ward around 6:30 hours. The implementation of a surgery acceleration project showing the importance of food in the control of the nutritional status of these elderly individuals with hip fracture.
Fractures in elderly patients are the most frequent accidents in this population with predominance of females and their worldwide incidence is constantly growing. These patients experience substantial perioperative pain and, if inadequately controlled, are associated with numerous complications that include pneumonia, urinary tract infection, delirium and venous thromboembolism. Oral and parenteral administration of opioids continues to be the mainstay of treatment for acute pain but have their own profile of side effects that include nausea, vomiting, delirium, respiratory depression and urinary retention [45]. Regional anesthesia may provide better analgesia, while decreasing opioid-related side effects. Effective postoperative analgesia reduces the incidence of postoperative complications, decreases hospital stay, increases patient satisfaction and decreases costs.
In several services, hip fracture is performed with local anesthetics hyperbaric or isobaric bupivacaine associated with the use of opioid adjuvants (fentanyl and morphine). Patients under spinal anesthesia with 0.5% bupivacaine hyperbaric combined with 200 μg of intrathecal morphine, had a higher incidence of urinary catheterization, more time to urinate and more time to urinate compared to patients receiving only local anesthetics. Based on current evidence, a recent meta-analysis showed that urinary catheterization during total knee arthroplasty may increase urinary tract infection in the postoperative period, and routine use in these patients may not be necessary. Routine preoperative bladder catheterization may not be justified in patients with total hip arthroplasty. Postoperative catheterization, as needed, can be more cost effective [46-48].
In the implementation of the ACERTO project in a SUS hospital, both concepts were used: analgesia without opioids and not using a delayed bladder probe [11-13,23-33]. In all these studies, lumbar plexus block was used both anteriorly and posteriorly, with the aid of a neurostimulator depending on the position of the surgery. Normally in surgeries in the supine position, lumbar plexus block was performed before surgery, with an association of 2% lidocaine with epinephrine (20 mL) and 0.5% bupivacaine (20 mL). When surgery was performed in lateral decubitus, subanesthetic doses of dextroketamine (0.1 mg/kg) were administered and postoperative analgesia was obtained with posterior lumbar plexus block (psoas compartment) and injection only 0.25% bupivacaine (40 mL), providing analgesia for around 22 hours [12,13,24]. There was no need to use a bladder catheter in any patient after the ACERTO project was implemented.
In a systematic review comparing the analgesic efficacy of fentanyl versus femoral nerve block before of positioning to perform spinal anesthesia in femoral fracture patients evaluated with pain scales showed that femoral nerve block reduced the level of pain and the need for additional analgesia [49]. The review showed the importance of using subanesthetic doses of dextroketamine for analgesia for subarachnoid puncture and for sedation during the surgical procedure.
Delirium is the most common postoperative neurological complication in elderly patients operated on hip fracture and is associated with increased morbidity and mortality. Changes in the level of consciousness in the elderly individual are characteristic of postoperative delirium and its cause is multifactorial and its pathophysiology remains to be clarified. Pain after fracture and its response to injury and the use of opioid for pain treatment are likely risk factors for delirium in elderly patients [50]. In these patients, medications for sedation and drug analgesia should be reduced, and local anesthetics for peripheral block analgesia should be preferred [12-14].
In a systematic review showed that subanesthetic ketamine administration reduces postoperative markers of inflammation as well as postoperative pain and opioid consumption [51,52]. In the implementation of the ACERTO project, subanesthetic doses of dextroketamine were frequently used [34] and the incidence of delirium in 224 patients was 5.8% [34, 32].
Procedural sedation encompasses a wide range of patients, procedures, venues, and specialty providers. Recent studies indicate that the anxiolytic agent administered before surgery has a negative impact on the perioperative period in relation to the patient’s experience, which is important nowadays in patient-centered implementation and in the decision shared with patients and family members. Anxiolytic-sedative agents are used preoperatively in a large majority of patients and the pharmacokinetic characteristics of many of these agents are not ideal for the indication and intended objective [53-55]. Added to these data, reduced anxiety was not observed in elderly patients. The results of this study emphasize the need for clear guidelineson the use of anxiolytic drugs in the perioperative period.
Several medical and psychiatric institutions are against the use of benzodiazepines or non-benzodiazepine hypnotics in older adult individuals [56]. Observational studies consistently report that benzodiazepine use is associated with a clinically significant increase in the risk of falls and fractures. Benzodiazepines are associated with falls through a number of mechanisms, including increased reaction time, interrupted balance and gait, sedation, and impaired vision. The ACERTO Project recommends a minimum of sedation and in the experience with patients over 60 years of age, the use of dextroketamine seems to have a much better result.
In August 2010, already using several approaches from the ERAS project, I was introduced to the ACERTO Project and because it is a totally free project. In a meeting with the direction of the Hospital do Brazilian Public Health (SUS) I decided to do the implantation for hip fracture elderly due to the few vacancies in IUC and the hospital’s routine of only performing surgery with guaranteed reservation in this unit. Until 2020, the implementation of ACERTO resulted in 15 published articles, with a reduction in the preoperative and postoperative fasting time, a decrease the number of suspensions of surgery, a decrease in hospital stay, a reduction in costs, and adherence by almost all Hospital Departments. Recovery acceleration projects like ACERTO have improved patient recovery time, hospital stay and have resulted in fewer complications for a variety of operations, including orthopedic patients.
A hip fracture is a significant injury to anyone, but for older people it can be catastrophic. Many of these patients never fully recover and some die as a result of the fracture. Hip fractures are associated with high rates of morbidity and mainly loss of functional independence. The projects to accelerate postoperative recovery are multidisciplinary with protocols designed to improve patient outcomes, hospital experience and efficiency after surgery, focusing mainly on the patient, family involvement, multimodal analgesia, and the long-term prevention of fasting before and after surgery, adequate nutrition, early mobility and better evidence for damage prevention.
A hip fracture is a significant injury to anyone, but for older people it can be catastrophic. Many of these patients never fully recover and some die as a result of the fracture. Hip fractures are associated with high rates of morbidity and mainly loss of functional independence. The projects to accelerate postoperative recovery are multidisciplinary with protocols designed to improve patient outcomes, hospital experience and efficiency after surgery, focusing mainly on the patient, family involvement, multimodal analgesia, and the long-term prevention of fasting before and after surgery, adequate nutrition, early mobility and better evidence for damage prevention.
