Author(s): <p>Naseema Begum Nidagundi</p>
Introduction: Fibroblasts are the most important cells in wound healing. Chlorhexidine is the most widely used and investigated chemical plaque control agent after periodontal surgeries and Low-level laser therapy (LLLT), or photo biomodulation (PBM), refers to using photons to modulate biological activity. Since literature have shown promising results on fibroblasts viability following LASER irradiation, we aimed to evaluate and compare the effect of chlorhexidine mouthwash and LASER on survival of human gingival fibroblasts.
Material and Methods: The experimental and control groups are as follows: Group I - Control, Group II - Fibroblasts treated with Chlorhexidine (Peridex), Group III - Fibroblasts irradiated with diode LASER. The cells in group II were treated with Chlorhexidine (Peridex-0.12%) whereas the cells in group III were irradiated diode LASER 5 seconds and cell viability was assessed using MTT Assay.
Statistical Analysis: Comparison between all three groups was done by Kruskall Wallis ANOVA Inter group comparison (>2 groups) was done using Kruskall Wallis ANOVA followed by pair wise comparison using Mann Whitney U test.
Results: No change in the viability of cells in the control group, whereas the viability decreased to 50.4 % in group 2, which was statistically significant when compared with the control group (p<0.01) and increased to 101.86 % in grp 3, but statistically insignificant when compared to control group (p>0.01). Also, there was a statistically significant difference observed between group 2 and group 3 (p<0.01).
Conclusion: Chlorhexidine treatment to fibroblasts resulted in the decreased viability of the fibroblasts, and LASER irradiated cells, neither showed a significant reduction nor a significant increase in viability of fibroblasts. And when the two test groups, chlorhexidine treated and LASER irradiated groups, were compared there was a statistically significant difference observed.
Fibroblasts are responsible for the production of structural proteins, and extracellular matrix and are the predominant cellular element in the gingival and periodontal connective tissue. Thus, any toxic effects on these cells have important implications in periodontal wound healing [1].
Tissue healing involves an intense activity of diverse cell types, such as epithelial and endothelial cells, and fibroblasts, which play a key role in this process. They secrete multiple growth factors during wound re epithelialization and participate actively in forming granulation tissue and synthesizing a complex extracellular matrix after re-epithelialization. All these processes directly involve the proliferation and migration capacity of these cells [2].
The most widely used and investigated chemical plaque control agent is Chlorhexidine (CHX). The superior effect of CHX is due to its substantivity. CHX is accepted as a safe and effective antiplaque agent, but several studies showed that CHX is cytotoxic to many cells such as human dermal fibroblasts, gingival and periodontal ligament fibroblasts, and alveolar bone cells [3].
Low-level laser therapy (LLLT), or photo biomodulation (PBM), refers to using photons to modulate biological activity. This type of therapy uses non-thermal laser light, mostly from the red and near-infrared regions of the spectrum [3]. The application of lasers as an adjunct to conventional periodontal therapy is becoming more and more prevalent in dental offices as well as the use of LLLT promotes the bio stimulation of fibroblasts and accelerates the healing process [4].
Since chlorhexidine is most commonly prescribed mouthwash following periodontal surgeries, and literature have shown promising results on fibroblasts viability following LASER irradiation, we planned to evaluate and compare their effect on fibroblasts invitro.
Hence, the aim of this study is to evaluate and compare the effect of chlorhexidine mouthwash and LASER on survival of human gingival fibroblasts.
The experimental and control groups are as follows:
Group I - Control
Group II - Fibroblasts treated with Chlorhexidine (Peridex)
Group III - Fibroblasts irradiated with diode LASER
The cells were seeded in a 24-well flat-bottom microplate and maintained at 37°C in 95% humidity and 5% CO2 overnight. The cells in group II were treated with Chlorhexidine (Peridex-0.12%) and incubated for 3 days, whereas the cells in group III were irradiated diode LASER every 24 hours totalizing 3 applications during 3 consecutive days. (The procedure of LASER irradiation is discussed below). The wells in both the groups were then washed twice with PBS. 20 μl of the MTT reagent solution (5 mg/ ml of PBS) was added to each well and the plate was incubated for 4 h in the dark. The formazan crystals formed were then dissolved by adding 100 μl dimethyl sulfoxide (DMSO) and absorbance was recorded at 570 nm using a microplate reader (Bio-Rad, California, USA) [5].
Surviving cells (%) = Mean OD of test compound /Mean OD of Negative control x100
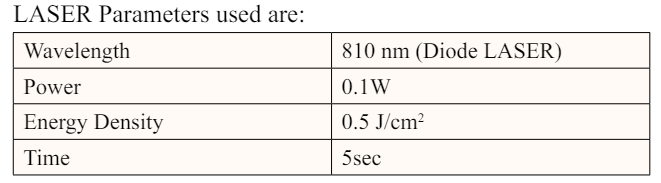
Diode laser of wavelengths of 810 nm, with an 8mm delivery device and output power of 0.1W was used. The fibre tip was placed perpendicular to the bottom of each well at a fixed distance of 15 mm to cover only 1 well of a 96-well plate. The required irradiation time for delivering an energy density of 0.5 J/cm2, was 5 sec. The laser treatment was performed after every 24-hr followed by 48 and 72 hr of incubation [4].
Inter group comparison (>2 groups) was done using Kruskall Wallis ANOVA followed by pair wise comparison using Mann Whitney U test.
For all the statistical tests, p<0.05 was considered to be statistically significant, keeping α error at 5% and β error at 20%, thus giving a power to the study as 80%.
* = statistically significant difference (p<0.05)
** = statistically highly significant difference (p<0.01) # = non-significant difference (p>0.05)
Results: Data obtained from the MTT Assay is given in Table
No.1 and represented in Graph 1.
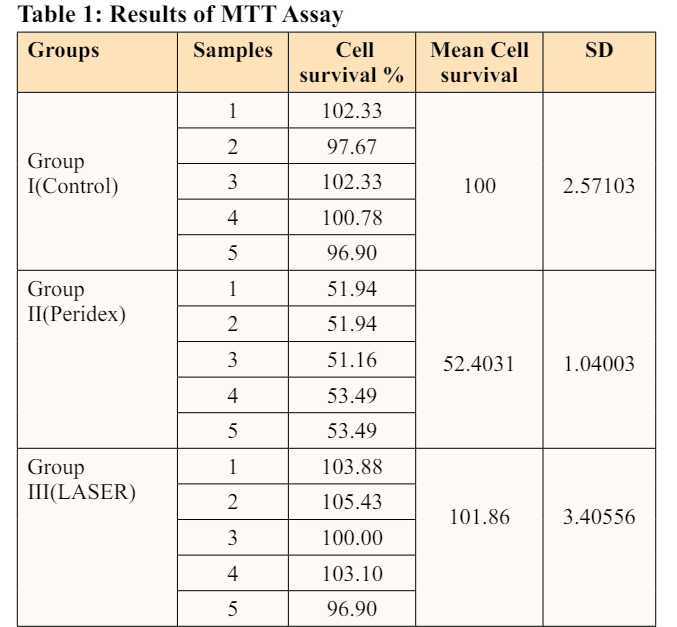
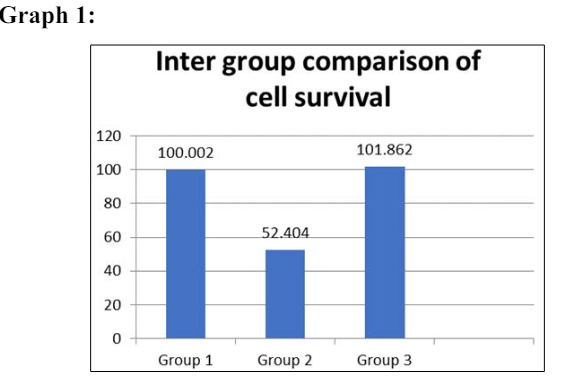
Table 1 and Graph 1 show results from the MTT assay showing no change in the viability of cells in the control group, whereas the viability decreased to 50.4 % in group 2, which was statistically significant when compared with the control group (p<0.01) and increased to 101.86 % in grp 3, but statistically insignificant when compared to control group (p>0.01). Also, there was a statistically significant difference observed between group 2 and group 3 (p<0.01).
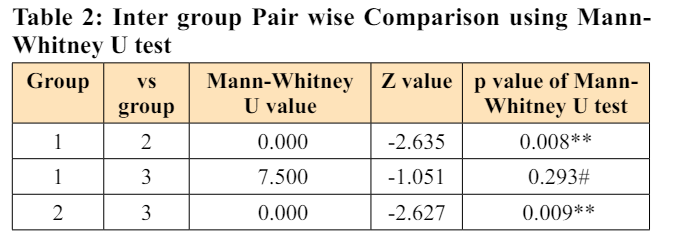
Table 2 is showing Inter group Pair wise comparison using Mann- Whitney U test, statistically significant difference was observed when group 1 was compared with group 2 (p<0.05) and when group 2 was compared with group 3 (p<0.05). There was no statistically significant difference noted when 1was compared with group 3 (p>0.05).
In the present study cell viability was evaluated after chlorhexidine (Group II) and Laser treatment (Group III) and later the viability was compared between two groups.
The results of our study showed that Chlorhexidine is cytotoxic to cells in vitro, Similar results were observed in many of the previous studies such as studies by Jeffery J. Pucher et al, Paul Goldschmidt et al, Flemingson et al, Ioannis Tsourounakis et al, Marzena Wyganowska-Swiatkowska et al and many others [6-10].
Although these studies evaluated the cytotoxicity of chlorhexidine in gingival fibroblasts, a comparison of the reported results is difficult due to the variability of the applied methodology, namely the commercial product used (with different compositions and sometimes containing alcohol), the studied concentrations, the exposure time and the chosen medium. A decrease in chlorhexidine cytotoxicity was also identified when the medium contains FBS [10].
The present study demonstrated no significant increase in the proliferation of human gingival fibroblasts irradiated with LASER compared to non-irradiated cells. These findings were discordant with previous studies including a study by Fernanda G. Basso et al (2012) where it was observed that fibroblasts irradiated with LASER with 0.5 and 3 J/cm2 resulted in a significant increase in cell metabolism compared with the nonirradiated group [11]. Here diode LASER of 780 ± 3nm wavelength was used with varying energy densities including 0.5J/cm2, at 0.04W, for 40 seconds of duration. But in our study, the duration for which the cells were exposed to LASER was only 15 seconds in total. Therefore, the reason for no significant increase in viability of cells could be the lesser duration of exposure which was 5 seconds and hence less joules used.
Mohammad Ayoub Rigi Ladiz1et al (2020) evaluated the effect of a single session of the laser by using similar parameters as our study (810nm diode LASER,0.5J) and observed results contrary to our study with a significant increase in viability of gingival fibroblasts after 24 hrs,48hrs, and 72 hrs even after only a single session of exposure, but this study did not mention the duration of exposure of cells to LASER [12].
A preliminary report by Barbara Sterczala et al (2021) also showed results contrary to the results of our study, showing a significant increase in the proliferation of gingival fibroblasts irradiated with LASER, but here varying wavelengths and energy densities were used and it did not include diode LASER [13].
Chlorhexidine treatment to fibroblasts resulted in the decreased viability of the fibroblasts, and LASER irradiated cells, neither showed a significant reduction nor a significant increase in viability of fibroblasts. And when the two test groups, chlorhexidine treated and LASER irradiated groups, were compared there was a statistically significant difference observed.
1.Khedr MM, Fahmy Ali WA, Saleh AA, El-Tayeb TA (2016) Effect of laser on the human gingival fibroblast treated with chlorhexidine. Life Science Journal 13: 2.
2.Basso FG, Pansani TN, Turrioni AP, Bagnato VS, Hebling J, et al. (2012) In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent. 2012: 719452.
3.Sukumaran SK, Vadakkekuttical RJ, Kanakath H (2020) Comparative evaluation of the effect of curcumin and chlorhexidine on human fibroblast viability and migration: An in vitro study. J Indian Soc Periodontol 24: 109-116.
4.Ladiz MA, Mirzaei A, Hendi SS, Najafi-Vosough R, Hooshyarfard A, et al. (2020) Effect of photobiomodulation with 810 and 940 nm diode lasers on human gingival fibroblasts. Dental and Medical Problems 57: 369-376.
5.Kumbar VM, Peram MR, Kugaji MS, Shah T, Patil SP, et al. (2020) Effect of curcumin on growth, biofilm formation, and virulence factor gene expression of Porphyromonas gingivalis. Odontology 109: 18-28.
6.Pucher JJ, Daniel C (1992) The effects of chlorhexidine digluconate on human fibroblasts in vitro. Journal of periodontology 63: 526-532.
7.Goldschmidt P, Cogen R, Taubman S (1977) Cytopathologic effects of chlorhexidine on human cells. Journal of periodontology 48: 212-215.
8.Flemingson, Emmadi P, Ambalavanan N, Ramakrishnan T, Vijayalakshmi R (2008) Effect of three commercial mouth rinses on cultured human gingival fibroblast: an in vitro study. Indian J Dent Res 19: 29-35.
9.Tsourounakis I, Palaiologou-Gallis AA, Stoute D, Maney P, Lallier TE (2013) Effect of essential oil and chlorhexidine mouthwashes on gingival fibroblast survival and migration. Journal of periodontology 84:1211-1220.
10.Wyganowska-Swiatkowska M, Kotwicka M, Urbaniak P, Nowak A, Skrzypczak-Jankun E, et al. (2016) Clinical implications of the growth-suppressive effects of chlorhexidine at low and high concentrations on human gingival fibroblasts and changes in morphology. International Journal of Molecular Medicine. 37: 1594-1600.
11.Basso FG, Pansani TN, Turrioni AP, Bagnato VS, Hebling J, et al. (2012) In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent. 2012: 719452.
12.Ladiz MA, Mirzaei A, Hendi SS, Najafi-Vosough R, Hooshyarfard A, et al. (2020) Effect of photobiomodulation with 810 and 940 nm diode lasers on human gingival fibroblasts. Dental and Medical Problems 57: 369-376.
View PDF