Author(s): Sujatha N Rao* and Kuldeep GB
Objective: The primary objective of the present study was to evaluate the serum electrolyte levels in diabetic nephropathy compared with age matched healthy control.
Method: Cross sectional study involving 240 individuals in the populations of Bengaluru, India from the period of January 2019 to December 2019 was considered for the study. Venous blood was collected from 240 individuals comprising 120 Diabetics with nephropathy and 120 healthy individuals and analyzed for Glycosylated Hemoglobin(HbA1c), serum sodium, potassium, chloride, calcium, magnesium and phosphorous along with their demographic details.
Results: Age, gender had a statistical significance with diabetic nephropathy, among electrolytes, calcium, potassium and chloride levels were significantly elevated while sodium, magnesium and phosphorous displayed significant decrease in Diabetics with nephropathy compared to healthy control population.
Conclusion: These variations in electrolyte levels can be a signal of progression of Type 2 Diabetes into Diabetic Nephropathy. Hence frequent monitoring of these electrolytes helps in early detection of diabetic complications thus preventing it from progressing further.
Type II diabetes mellitus have been identified as the biggest silent lifestyle epidemics in the human history [1, 2]. It warrants an immediate attention for research, particularly in the Indian context as India has emerged as the second largest contributor of diabetics to the world population with more than 72.9 million adults, positioned only after China (120 million) [3]. Recent study by Anjana et al. report that more than half of the Indian adult population is diabetic [4]. The increase in diabetes also amounts to incremental enhancement to the complications related to diabetes such as neuropathy, nephropathy, dyslipidemia, retinopathy, etc. The majority of the patients die because of kidney diseases and cardiovascular complications (coronary artery disease, peripheral arterial disease and cerebrovascular disease [5, 6]. India also reported the second highest number of diabetes related deaths in the world [3]. Among these, diabetic nephropathy, the most common microvascular complication, is known to impact more than 1/3rd of the diabetics [2, 6]. Electrolytes sodium, chloride, potassium, calcium, phosphorous and magnesium have crucial role in metabolism and are closely linked with each other. Sodium and potassium are needed for the dietary glucose absorption apart from their role in maintaining electrochemical neutrality and acid base balance along with chloride which indicates that these electrolytes also affect diabetes [7-9]. Calcium elevates the glucose levels in the body by acting as the second messenger for stress hormones. It is also essential for the secretion and release of insulin from P cells of the pancreas in response to hyperglycemia and controls glycolysis for the synthesis of ATP. Meanwhile, phosphorus is a component of phospholipids of the cell membrane through which glucose is transported into the cell by the insulin receptors. Inside the cell, glucose phosphate ester formation requires phosphorus, which is also needed as a part of the coenzymes of glucose metabolism. Magnesium is required for the binding activity of the insulin besides activating several enzymes of glucose metabolism [5, 10, 11]. Alterations in these electrolyte levels are found to be associated with diabetes mellitus [12, 13]. Previous studies evaluating the relationship between electrolyte levels and diabetes have shown contradictory results [14-19]. Also, association of electrolytes with diabetic related complications has not been well studied till date. Therefore our study aims to evaluate the serum electrolyte levels in diabetic nephropathy.
This is a cross sectional study conducted at the Shree Krishna Sevashrama Hospital, Bengaluru, and Karnataka, India from January 2019 to December 2019. A total of 240 individuals, which can be divided into 2 groups as per WHO criteria for diabetes were included in this study that were matched for age and gender. After obtaining the Institutional ethical committee approval, informedconsent was taken from all the individuals participated in this study. The subjects were divided into 2 groups. The Group 1 comprised of 120 healthy individuals who had availed wellness plan offered by the institution, in the age ranging from 35 to 75 years of either gender. The exclusion criteria comprised of pregnant and lactating women. The Group 2 comprised of 120 confirmed patients of Type 2 DM with nephropathy, exhibiting symptoms such as oedema, albuminuria with low albumin levels in the blood and serum creatinine higher than 1.4 mg/dl.
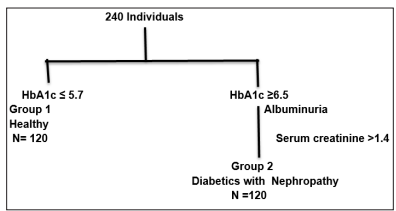
Figure 1: Flow Chart For The Selection of Study Population
Blood sample was collected to obtain the level of electrolytes. 7 ml of venous blood was collected from the antecubital vein by taking aseptic precautions and was divided into 2 parts. The first part was transferred to labelled EDTA tube, centrifuged to obtain plasma, which was analyzed for HbA1c. The second part of the sample was allowed to clot, serum was separated by centrifugation and used for the estimation of Sodium, potassium, chloride, calcium, phosphorus, magnesium and creatinine by Auto lab VERSA Clinical Chemistry Analyzer manufactured by Euro diagnostic System pvt ltd, Chennai, India. Serum Calcium was analyzed as calcium arsenazo complex. Serum Phosphorus was analyzed by moly date uv method. Serum Magnesium was analysed by calmagite colorimetric method. Serum Chloride was analyzed by Photometric test using ferric (111) perchlorate. Serum Sodium and serum Potassium was analyzed by Enzymatic photometric test method. Serum Creatinine was analyzed by jaffe’s kinetic method. Routine urine analysis for glucose and albumin was conducted in all the subjects In case of Diabetics with nephropathy group, 24h urine samples were collected for the estimation of albuminuria by, immune turbid metric method.
The data were expressed as mean± S.D. All the statistical analysis was performed using the SPSS statistical tool. Student test was performed to find the difference between diabetics with nephropathy and the control group. The results of all the tests with p value < 0.001 was considered as statistically highly significant.
| Parameter | Group 1 Healthy Control N=120 |
Group 2 diabetics with nephropathy N= 120 |
|---|---|---|
| Age | 41.36±5.57 | 60.23± 13.88 |
| Male | 68 (57%) | 96 (80%) |
| Female | 52(43%) | 24 (20%) |
| HbA1c | 5.23± 0.40 | 10.22± 1.76 |
| Serum Creatinine mg/dl Normal Range 0.6-1.4 mg/dl | 0.90± 0.14 | 1.8± 0.10 |
| Albuminuria | ----ve | +ve |
As shown in Table 1, mean age of diabetics with nephropathy was significantly higher (60.23±13.88, p=0.001) than the mean age of the control group 41.36±5.57. Chances of progression of diabetes into diabetic nephropathy increased with age as per our study. Relationship with gender and diabetic nephropathy was also observed to be statistically significant. Males comprised of 57 % of control group and 80% of diabetics with nephropathy group. Females comprised of 43% in control group and 20% in diabetics with nephropathy group indicating that Males were more prone to diabetic nephropathy compared to Females. HbA1c level in case of diabetics with nephropathy was significantly higher (10.22±1.76) than the control group (5.23± 0.40). Table 2 shows the various electrolyte levels in both the study groups, serum Calcium in diabetics with nephropathy was statistically significantly higher (10.30 ± 0.2, p = 0.001) compared to that of control group (9.25± 0.65).Serum Phosphorous in diabetics with nephropathy, even though statistically significantly lower (3.30± 0.21, p=0.0001) than that of control group (3.89± 0.55), its levels were within the normal range. Serum Magnesium in diabetics with nephropathy was statistically significantly lowered (1.19± 0.11, p =0.0001) compared to control group (2.48± 0.10).
Serum Sodium in diabetics with nephropathy was significantly lowered (82.01± 7.12, p=0.0001) compared to control population (139.30±3.80).Serum Potassium in diabetics with nephropathy was significantly higher (5.59± 0.67, p=0.0001) compared to that of control population (4.59± 0.5). Serum Chloride in diabetics with nephropathy was statistically significantly higher (131.80±9.30, p=0.0001) compared to control (101.93± 4.44). Table 3 shows the correlation of serum electrolytes with HbA1c in diabetics with nephropathy patients. HbA1c is negatively correlated with phosphorous(r = - 0.03), Magnesium (r = - 0.06) and Sodium (r = - 0.04). HbA1c is positively correlated with Calcium ( r =0.09 ),potassium (r=0.12)and Chloride (r=0.20).
| Normal Range of serum Electrolytes |
Electrolyte levels in Control Healthy Group 1 |
Electrolyte levels in Diabetics with Nephropathy Group 2 |
P value | |
|---|---|---|---|---|
| Serum Calcium | 8.4-10 mg/dl | 9.25± 0.65 | 10.30± 0.21 | 0.0001 |
| Serum Phosphorous | 2.5-5.0 mg/dl | 3.89± 0.55 | 3.30± 0.21 | 0.0001 |
| Serum Magnesium | 1.6-3.0 mg/dl | 2.48± 0.10 | 1.19± 0.11 | 0.0001 |
| Serum Sodium | 135-145 m Eq/L | 139.30±3.80 | 82.01± 7.12 | 0.0001 |
| Serum Potassium | 3.5- 5.2 m Eq/L | 4.59± 0.51 | 5.59± 0.67 | 0.0001 |
| Serum Chloride | 96-106m Eq/L | 101.93± 4.44 | 131.80± 9.30 | 0.0001 |
| Calcium | 0.09 | 0.0001 |
|---|---|---|
| Phosphorous | -0.03 | 0.0001 |
| 0.0001 | ||
| Magnesium | 0.06 | 0.0001 |
| Sodium | -0.04 | 0.0001 |
| Potassium | 0.12 | 0.0001 |
| Chloride | 0.20 | 0.0001 |
Our study results indicated that the demographic variables such as age had a statistically significant association with diabetic nephropathy. Both age and gender had an impact on diabetic nephropathy as per our study. Similar observations were reported by previous studies [2, 11, 12, 14, 15]. The age reported for onset of diabetic nephropathy was comparatively higher in Saudi Arabia than our results [20]. In our study of serum electrolytes- sodium, phosphorous, and magnesium were decreased in their level significantly while calcium, potassium and chloride were elevated significantly in diabetics with nephropathy group compared to the control group. Deranged glucose metabolism and hyperglycemia along with alterations in Renin Angiotensin mechanism in diabetic nephropathy results in an osmotic force that moves water from intracellular space to extracellular space diluting the extracellular sodium resulting in lowered plasma sodium levels while refluxing the potassium to extracellular space causing Hyperkalemia [21, 22]. Previous studies reported similar findings in case of sodium and not in case of potassium [9, 13]. Increased chloride levels may be due to increased synthesis and release of ketone bodies in diabetic nephropathy leading to diabetic ketoacidosis resulting in Renal Tubular Acidosis. Nephron dysfunction leads to impaired excretion of potassium and hydrogen resulting in increased chloride levels. Similar findings were reported by previous studies [22]. Increased serum calcium is due to calcium reabsorption in PCT which is associated with sodium reabsorption. Calcium competes with magnesium for transport in the loop of Henle resulting in low magnesium levels. As per Resnick Ionic Hypothesis, decreased Magnesium levels are associated with elevated calcium levels [8].
Our study showed higher calcium, chloride, potassium and low sodium, magnesium and phosphorous in diabetic nephropathy reflecting the altered electrolyte levels. These variations in electrolyte levels can be a signal of progression of Type 2 diabetes into diabetic nephropathy. Hence frequent monitoring of these electrolytes helps in early detection of diabetic complications thus preventing it from progressing further.
Authors thank Sri Krishna Sevashrama Hospital, Benagaluru for giving us an opportunity to conduct this study.
