Author(s): Lino Di Rienzo Businco, Marco Radici, Pasquale Longo, Fausto Carru and Andrea Di Rienzo Businco
Introduction: KOS represent an innovative non-surgical solution developed at the Karolinska University Hospital in Stockholm (Sweden) which consists of a intranasal stimulation via an air inflated catheter indicated to treat non allergic rhinitis and migraine. The KOS method for rhinitis has proved to be so effective as it simultaneously stimulates the nasal mucosa and the local autonomic nervous system, which represents the predisposing ultrastructural factor and is able to maintain the neurogenic inflammation responsible for the nasal symptoms of chronic rhinitis, very disabling for the quality of life of rhinitic patients.
We wanted to verify whether the positive results obtained in the treatment of non-allergic rhinitis that we observed in our previous study could also be obtained in patients with allergic rhinitis, who similarly share many of the nasal symptoms.
Materials and Methods: A total of 110 patients (63 males), aged >18 years, consecutively enrolled, all undergoing complete ENT evaluation with physical clinical examination, endoscopy, nasal symptoms VAS and SNOT-22 questionnaire, affected by allergic rhinitis (AR) persistent moderate-to-severe grade. All patients were alternately assigned to 2 homogeneous groups (Group A: Control Subjects, Group B: KOS Treated Patients), each group included 55 individuals. Simple randomization was achieved with a sequence of random numbers from a computer-generated sequence. During the study, both groups received standard medications (Ebastine tablet 10 mg and Mometasone furoate nasal spray 50 mcg/actuation per nostril per day) for 90 days. At the beginning of medical treatment, group B patients underwent first KOS treatment (repeated after 20 days). Both groups were asked to report any side effects during the study.
Results: The treated patients already benefited immediately after the extraction of the balloon reporting a sensation of a more patent nose and reduction of nasal secretions which progressively improves in the following days.
For the subjective complaints (nasal obstruction, sneezing, rhinorrhea, and itching), the improvement was significant within each group, with the most significant improvements in treatment group B. When the KOS treatment group was compared with medical treatment alone (Group A), greater efficacy was observed in Group B with regards to the reduction of nasal symptoms and nasal endoscopic findings.
Regarding the objective results (rhinomanometric assessments), similar trends, such as subjective ones, were observed within each group. The improvements within each treatment group were significant without side effects.
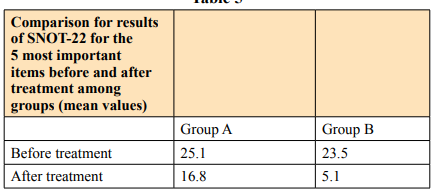
Comparison between Groups A and B, before and after treatment, with the SNOT-22 questionnaire relating to the 5 most important questions (5 most important items) showed an improvement in both study groups but with better results, however regards efficacy, in Group B.
Discussion: Our results reveal a greater efficacy achieved using a combined approach, with the association between medical treatment and KOS, compared to medical treatment alone, in the control of the sympotms of AR associated with hypertrophy of the inferior turbinates. The symptoms evaluated by VAS showed greater efficacy in their control in those patients in treatment group B, in particular those patients who had undergone treatment with KOS presented objective parameters (AAR, endoscopic score) and SNOT-22 better than the group receives only medical care.
Conclusion: KOS treatment, in combination with medical therapy, improves nasal flow more effectively than medical treatment alone in persistent moderate to severe AR. In particular, the local nasal symptoms were significantly reduced.
Patients undergoing the KOS treatment report improvement in their nasal rhinitis symptoms within a few days, which improve further, also in our experience, after a second boost application.
Allergic rhinitis (AR) is an epidemic clinical condition very common worldwide often overlapped with aspecific rhinitic conditions (infective, irritative, vasomotor, cold) presenting with the main and most disabling symptoms of nasal obstruction and rhinorrea. This condition is almost always related with inferior turbinate hypertrophy, caused by immunophlogosis which leads to persistent inflammation with edema and mucosal prolapse that obstruct the nasal cavities and sometimes the paranasal sinuses. Inferior turbinate hypertrophy may become irreversible when vascular dilatation leads to prolapse of the submucosal venous sinusoids that become unresponsive to the local sympathetic nervous system and medical care. Several studies have revealed that a percentage (between 20-25%) of the population has nasal obstructive symptoms with hypertrophy of the inferior turbinates, related to allergy [1,2,3].
When medical treatments (antihistamines, steroids, specific desensitizing immunotherapy) are not sufficient to resolve the patient’s nasal symptoms, the quality of life is considerably compromised and it is often necessary to subject the patient to a surgical approach to improve the flow of air through the nose. Turbinate surgery is, in fact, very common and represents the eighth operation, in order of frequency, performed in ENT surgery [4].
Numerous surgical techniques have been proposed for the treatment of inferior turbinate hypertrophy: the main problem consists in increasing the flow of nasal air while maintaining the functionality of the mucosa, an area of important protective actions and absorption of drugs useful in post-treatment - longterm surgery of allergic inflammation (turbinectomy, submucosal surgical emptying, cryocoagulation, electrocaustication, laser, radiofrequency, coblator, Mechan, Quantic Molecular Resonance).
Many of these techniques and, in particular, those performed at high temperatures and the extremely destructive ones, with almost complete amputation of the turbinate, while ensuring an increase in the nasal air flow, were accompanied by the loss of nasal sensitivity and the formation of vortices of air up to dreadful conditions of “empty nose” syndromes with crusting, bleeding and synechia, with an extremely negative impact on the quality of life (QoL) of patients and their psychic balance [5].
Almost no effect are expected after too much invasive surgical procedures on rhinitic sympotoms such as rhinorrea, sneezing, itching, and patients dislike undergoing to these surgical procedures.
In the present study we aimed to establish the efficacy and safety of a new technique recently introduced in Sweden (Chordate) for the treatment of non-allergic rhinitis named KOS (Kinetic Oscillation Stimulation) using a specific medical device for the non-surgical therapy of inflammation nasal neurogenic, to evaluate its effectiveness in a group of patients with moderate to severe persistent allergic rhinitis, as an adjunct to standard medical treatment (nasal steroid and oral antihistamine).
KOS represent an innovative non-surgical solution developed at the Karolinska University Hospital in Stockholm (Sweden) which consists of a intranasal stimulation via an air inflated catheter indicated to treat non allergic rhinitis and migraine. The KOS method for rhinitis has proved to be so effective as it simultaneously stimulates the nasal mucosa and the local autonomic nervous system, which represents the predisposing ultrastructural factor and is able to maintain the neurogenic inflammation responsible for the nasal symptoms of chronic rhinitis, very disabling for the quality of life of rhinitic patients [6,7,8].
We wanted to verify whether the positive results obtained in the treatment of non-allergic rhinitis that we observed in our previous study could also be obtained in patients with allergic rhinitis, who similarly share many of the nasal symptoms [9].
The aim of the study was to compare the variation of parameters and clinical-instrumental symptoms at the beginning and at the end of the treatment. The patients were then divided into two study groups, the first treated with pharmacological treatment and the second with both medical treatment and intranasal KOS.
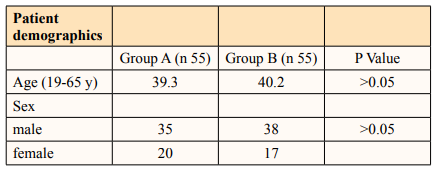
A total of 110 patients (63 males), aged >18 years, consecutively enrolled in the present study (Table I), all undergoing complete ENT evaluation with physical clinical examination, endoscopy, nasal symptoms VAS and SNOT-22 questionnaire, affected by allergic rhinitis (AR) persistent moderate-to-severe grade, based on ARIA/EAACI criteria (Alergic Rhinitis and its Impact of Asthma document and the European Academy of Allergology and Clinical Immunology) with inferior turbinate hypertrophy. All patients had a positive allergenic skin prick test for dust mites (Dermatophagoides pteronyssinus or Dermatophagoides farinae) and/or plant allergens (Gramineae, Cupressus or Parietaria) and had specific IgE (immunoglobulin E) for the class 3 major allergen -4 (Rast -CAP System EIA method, Pharmacia, Uppsala). These patients had not received any form of medical treatment in the 4 months prior to study entry (maximum 6 antihistamine tablets and/or 10 actuations of steroid spray in each nostril).
The criteria used to enroll patients in the study were: nasal symptoms (nasal obstruction, runny nose-rhinorrea, sneezing, and itching) with a score >5 on a 0-10 visual analog scale (VAS); nasal resistance values > 0.25 (measured by rhinomanometry); and a clinical endoscopy score >2 (1 = small turbinate not in contact with septum or nasal floor; 2 = mild hypertrophic turbinate in contact with septum; 3 = moderate hypertrophic turbinate in contact with septum and nasal floor; 4 = severe hypertrophic turbinate in contact with the septum, nasal floor and upper endonasal compartment with complete nasal obstruction). Patients with non-allergic turbinate hypertrophy or nasal obstruction due to other reasons, such as significant septal deviations, previous turbinate or nasal surgery, nasal polyposis, recurrent sinusitis, severe systemic diseases, infections, and oncological conditions are were excluded from this study. All patients signed the Informed Consent Form and the study was officially approved by the local Ethics Committee.
All patients were alternately assigned to 2 homogeneous groups (Group A: Control Subjects, Group B: KOS Treated Patients), each group included 55 individuals. Simple randomization was achieved with a sequence of random numbers from a computergenerated sequence. During the study, both groups received standard medications (Ebastine tablet 10 mg and Mometasone furoate nasal spray 50 mcg/actuation per nostril per day) for 90 days. At the beginning of medical treatment, group B patients underwent first KOS treatment (repeated after 20 days). Both groups were asked to report any side effects during the study.
Group B: Patients undergoing KOS treatment according to standard protocol for 10 minutes of application in each nasal cavity. The KOS treatment was repeated 20 days after the first application.
The procedure did not cause bleeding or pain and did not require the insertion of nasal swabs in any of the patients in the treatment group.
The KOS balloon catheter is inserted into the nasal cavity through the nostril without the need for anesthesia or drug administration. To facilitate insertion, the balloon was introduced completely deflated and lubricated with medical oily ointment (Vaseline, paraffin). After introduction into the nostril, the balloon is inflated with air supplied by the Controller, and the stimulation determined by the kinetic oscillation of the balloon lasting 10 minutes begins (displayed on the display by a digital countdown). During the procedure, some sneezing and an itchy sensation in the jaw or zygomatic region may appear for a few seconds from the beginning of the stimulation, without the need to interrupt the treatment. At the end of 10 minutes, the balloon was deflated automatically and removed from the nostril without the need for any subsequent medication (no swabs, no drugs). No home analgesic therapies were required.
At study entry (time T0), participants were asked to rate the severity of subjective outcomes (nasal obstruction, rhinorrhea, sneezing, and itching), from 0 to 10, on a visual analog scale (VAS).
Before and after treatment, all patients were asked to answer a SNOT-22 (22-item Sino-Nasal Outcome Test) questionnaire and, subsequently, the results for the 5 most important items were compared.
SNOT-22: The 22-item Sino-Nasal Outcome Test (SNOT-22) is a modification of a pre-existing instrument, the SNOT-20 and it is a validated QoL instrument for the Italian population. The SNOT-22 questionnaire is scored using a Likert scale where 0=”No problem”, 1=”Very mild problem”, 2=”Mild or slight problem”, 3=”Moderate problem”, 4=”Severe problem”, and 5=”Problem as bad as it can be”. Higher total scores on the SNOT22 survey, obtained by means of the arithmetic sum of the score of the individual items, suggest worse patient functioning, greater severity of symptoms and a deterioration in quality of life (total score range: 0-110). In consideration that symptom severity and patient QoL are major drivers in the decision for KOS treatment, the objective of this study was to evaluate the proportion of patients receiving a minimal clinically important difference (MCID) of at least a 9-point improvement on the SNOT- 22 after KOS treatment, based on their preoperative QoL level.
The objective results (rhinomanometry) were evaluated to determine the resistance of the nasal passage. Rhinomanometry measures nasal airflow and pressure during breathing. Nasal resistance values were evaluated by active anterior rhinomanometry (AAR) (Rhinopocket ED200, Euroclinic srl, Bologna, Italy).
Active Anterior Rhinomanometry (AAR): AAR was performed using a rhinomanometer, calibrated according to standard requirements of the ICSR guidelines. The same operator, using the same instrument and following the standard operation procedure, performed rhinomanometry measurements. Patients wore a face mask with a small plastic catheter inserted in one nostril and attached to flexible silicone tubing leading to the pressure port of the meter, through a pierced piece of tape. During the examination, it was asked to the patients to close their mouths and breathe. For each nostril a rhinogram was recorded which related inspiratory and expiratory nasal airflow to transnasal pressure. For each nasal resistance, the AAR parameters considered were inspiratory and expiratory total nasal airway resistances. In various studies, mean total nasal airway resistance was found to be from 0.21 to 0.24 Pa/cm3/s, ranging from 0.14 to 0.37 Pa/cm3/s.
Total nasal airway resistance reflects the resistance of both side of nasal cavity. The advantage of measuring the total nasal airway resistance is to avoid the effect of nasal cycle over unilateral nasal airway resistance.
The AAR is a rapid test during which the patient must maintain a flow of air, breathing independently through the nose. In accordance with the International Committee for the Standardization of Rhinomanometry, episodes of nasal airflow resistance were measured at a standard pressure (150 Pascal), and total episodes of nasal resistance were calculated from unilateral rhinomanometric recordings.
AAR measurements were not performed if the patient presented in a symptomatic phase of an acute common cold or nasal allergy crisis, thus delaying the measurement until resolution of the acute phase, while those patients presenting with severe obstruction as far as concerning breathing through the nose, for which it was therefore impossible to record rhinomanometric values, were excluded from the study. AAR measurements were performed in a seated position, after a 15-minute acclimatization period in the room under standard temperature and humidity conditions.
In order to obtain functional data on the state of the nasal mucosa in the 2 study groups, the mucociliary transport time (MCTt) was calculated, before and after treatment. All patients underwent nasal MCTt evaluation, using a blend of charcoal powder and 3% saccharin. The MCTt was calculated as the time interval from the moment the powder was placed on the head of the inferiorturbinate (anterior compartment) until the appearance of a smear of the same powder on the oropharynx during direct pharyngoscopic examination , together when the patient reported a sweet taste in the throat.
Muco-Ciliary Transport Time (MCTt): MCTt was measured with an inert, colored tracer (charcoal powder). We swabbed a small quantity of the mixture onto the head of the inferior turbinate. Because the constituent of this tracer interacts with nasal secretions in different ways, it allows a precise evaluation of how an insoluble medium (charcoal) behave in a fluid. The use of this tracer provided us with information on mucociliary function objectively (via the appearance of the tracer on the posterior pharyngeal wall). Normal MCTt values in adults are 13 minutes (±3) for charcoal powder.
All these questionnaires and tests were repeated 3 months later (time T1).
Statistical Analysis The p-value of between-group improvement was calculated for all subjective and objective outcomes, and Chi-square was used.
The significance score was set at 0.05 to test the null hypothesis that there is no significant difference in objective and subjective nasal symptom reduction between the control and treatment groups.
Statistical analyzes were performed using SPSS (software package used for statistical analysis) Statistics version 17.0 (Chicago, IL, USA).
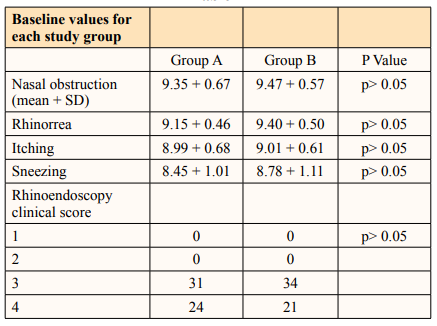
The study focused on 110 patients, aged 19-65 years (Table 1). At baseline, differences between groups were not significant (Table 2).
Group B patients reported no pain during the procedure. Some participants reported a slight itching or discomfort in the first minute of the procedure which however did not stop anyone from finishing the 10 minute application to the nasal passages. None of the participants experienced side effects during or after the procedure.
The treated patients already benefited immediately after the extraction of the balloon reporting a sensation of a more patent nose and reduction of nasal secretions which progressively improves in the following days.
For the subjective complaints (nasal obstruction, sneezing, rhinorrhea, and itching), the improvement was significant within each group, with the most significant improvements in treatment group B. When the KOS treatment group was compared with medical treatment alone (Group A), greater efficacy was observed in Group B with regards to the reduction of nasal symptoms and nasal endoscopic findings (Table 3).
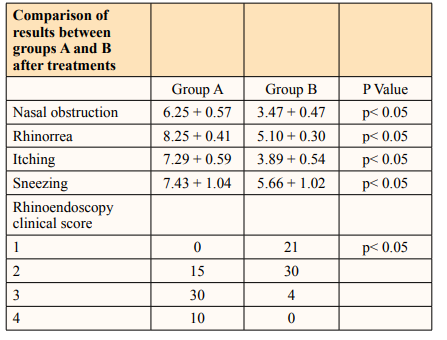
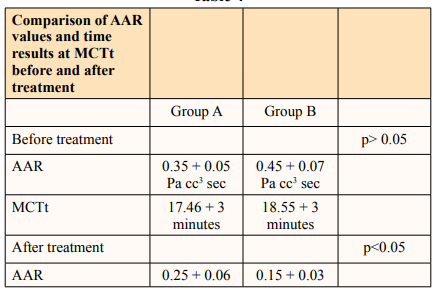
Regarding the objective results (rhinomanometric assessments), similar trends, such as subjective ones, were observed within each group (Tables 4). The improvements within each treatment group were significant without side effects.
Among the treatment groups, the group that received KOS as part of the treatment approach showed significantly greater symtpoms improvement than control group A.
The rhino-endoscopic clinical score (Table 3).showed significant improvements in both groups, but these were significantly higher in treatment group B (p<0.05).
The MCTt results showed no statistically significant differences between the two groups when comparing pre- and post-treatment values, thus indicating a substantial similarity between medical and KOS group as regards mucociliary function (Table 5).
Comparison between Groups A and B, before and after treatment, with the SNOT-22 questionnaire relating to the 5 most importantquestions (5 most important items) showed an improvement in both study groups but with better results, however regards efficacy, in Group B (Table 5).
Our results reveal a greater efficacy achieved using a combined approach, with the association between medical treatment and KOS, compared to medical treatment alone, in the control of the sympotms of AR associated with hypertrophy of the inferior turbinates. The symptoms evaluated by VAS showed greater efficacy in their control in those patients in treatment group B, in particular those patients who had undergone treatment with KOS presented objective parameters (AAR, endoscopic score) and SNOT-22 better than the group receives only medical care.
The lower reactivity of the mucosa after KOS is due to the downregulation of the tone of the parasympathetic system, with a reduction in the amount of inflammatory cells. Decreasing local nasal phlogosis and reactivity to allergens is one of the main goals of treatment for allergic rhinitis.
The mechanism behind this effect is not fully understood and further studies are needed, but it has been explained as a possible effect on the sensory nerves and the autonomic nerve system, i.e. the sympathetic part, or through the trigeminal parasympathetic reflex and an associated beneficial impact on autonomic balance (7, 9).
The results suggest an action due to the combined effectiveness of controlling the allergic response when KOS treatment is combined with medical treatment, acting in synergy.
The tMCT results reveal that the function of the mucosal surface of the turbinate, even after KOS, is preserved and improved and is a very important feature in a category of patients, such as those affected by AR who have to undergo local medical treatment of the nose for periods prolonged running the risk of mucosal atrophy.
Combining standard medical treatments for AR with KOS allow to reduce drugs intake (expecially nasal steroids) saving money for expensive and prolonged out pocket medications, and improve nasal symptoms, obtaining augmented benefit on quality of life of these patients.
KOS treatment, in combination with medical therapy, improves nasal flow more effectively than medical treatment alone in persistent moderate to severe AR. In particular, the local nasal symptoms were significantly reduced.
Patients undergoing the KOS treatment report improvement in their nasal rhinitis symptoms within a few days, which improve further, also in our experience, after a second boost application. However, the therapy can be repeated as often as the specialist deems it necessary, but in our experience is advisable to repeat the second treatment 20-30 days after the first application to maximize the therapeutic results and obtain an homogeneous treatment of the whole nasal cavities. Further researches are in progress to assess the stability of results we obtained, and the benefit of multiple and repeated application over the years for maintenance purpose to identify a precise and tailored therapeutic scheme.
