Author(s): <p>A M R Suresh*, Dimple Kashyap, Tapas Priyaranjan Behera and Anoop kumar Tarsolia</p>
Muscle Energy Technique, Non-traumatic Lumbo, Pelvic Pain
Pelvic girdle and low back pain have fallen under the diagnostic umbrella of non-specific low back pain (NSLBP) [1-6]. Consequently, a misconception that any exercise is good exercise was created. It is true that low back pain can have it’s etiology in pelvic girdle mal-alignment, and similarly low back pain with neural irritation can lead to inco-ordination of muscles causing pelvic mal-alignment [7-14]. However, clinically there appears to be very little non-specific about such problems. Traditionally, manual therapists have viewed impairment as loss of range of motion and/or perceived stiffness on joint mobilization. However, when considering low back pain and pelvic girdle dysfunction, the effects of muscular force transduction are becoming more evident as being an important impairment variable [16]. The clinician needs to be aware of Newton’s third law of ‘action- reaction’, the effects of inverse dynamics and the desire for symmetrical and appropriately timed force dissipation (‘damping’ and ‘propagation’) by supporting musculature. Sometimes these are referred to as ‘neuromuscular vectors’ [17]. Essentially, efficiency of movement is the desired outcome of any movement strategy, whereby muscles are considered as a series of slings acting across joints with differing movement functions. Most of us have experienced the stiffness and awkwardness of movement when learning a novel task [15]. Pain and dysfunction and/or inappropriate physiotherapy can result in excessive stiffness, which compromises the ‘fluidity’ and range of movement. Hence, such stiffness is the result of non-optimal neuro-muscular firing, rather than passive stiffness based on adhesions, scar tissue or degenerative changes [13]. Good clinical assessment with the application of appropriate muscle energy, manual therapy, soft tissue massage and dry needling techniques for reduction in of pain and muscle spasms, as well as appropriate exercise prescription for strength, endurance and motor control can be used as a management strategy whilst simultaneously ascertaining the ‘cause of the cause’ of dysfunction [9]. Therefore, don’t just rush into any rehabilitation protocol.
It is important to understand that motor inco-ordination in the pelvic girdle can be the result of peripheral and/or central mechanisms. Peripheral mechanisms include reflexogenic muscle spasms whilst central mechanisms include cortical inhibition of muscles and/or delayed central transmission due to noxious input affecting intra-cortical synergistic control between various cerebral, cerebellar and mid brain regions of the central nervous system (CNS). Altered proprioceptive input can result in an inaccurate ‘virtual body concept of self’ resulting in inaccurate feedback during the execution of motor tasks. Attention, stress and fear can inpact motor planning through altered perceptions of task demand and the environment where the execution of the task is to take place [18].
The sacroiliac or pelvic joint is not your typical joint. Rather than being made up of two bones and fibrous tissue encapsulating synovial fluid whose primary function is acting a ‘pulley’ to muscle action, the sacroiliac joint is a ligamentous fibrous non-conforming articulation with varying degrees of movement depending upon gender and collagen fibre type. A young person with JHS tend to be on one end of the SIJ movement spectrum whereas an elderly man would be on the other end [5].
Muscle energy technique (MET) is a common conservative treatment for pathology around the spine, particularly lumbopelvic pain (LPP). MET is considered a gentle manual therapy for restricted motion of the spine and extremities and is an active technique where the patient, not the clinician, controls the corrective force. This treatment requires the patient to perform voluntary muscle contractions of varying intensity, in a precise direction, while the clinician applies a counterforce not allowing movement to occur. For many years, MET has been advocated to treat muscle imbalances of the lumbopelvic region such as pelvis asymmetry [9]. The theory behind MET suggests that the technique is used to correct an asymmetry by targeting a contraction of the on the painful side of the low back and moving the innominate in a corrected direction [13]. It is worth noting however, that evidence suggests that non-symptomatic individuals have also been shown to have pelvis asymmetries. Despite this, MET is frequently used by manual therapy clinicians.
Unfortunately, few studies have examined the effectiveness of MET. Previous research has found that MET of the low back, improved self-report of disability when used with supervised neuromuscular re-education and resistance exercise training, but the effect of MET as an isolated treatment has not been determined. Cervical range of motion increased after 7 MET sessions, which consisted of four 5-second contractions over a 4-week period, and lumbar extension increased after 2 sessions per week for 4 weeks. Five-second contractions have shown greatest results with application at the atlanto-axial joint and the thoracic spine. While MET was successful in two studies, the effect of one treatment session was not reported and only range of motion was assessed. Roberts indicated the short-term effects of MET as decreased pain, increased range of motion, decreased muscle tension and spasm, and increased strength [4]. However, these effects seemed to last only a few seconds to minutes, indicating that for continued benefit, MET would have to be applied multiple times throughout the day. At present, the treatment window and lasting effect of a single MET session is undefined.
Evidence to support the use of lumbar manipulation in patients with acute Lumbo-pelvic pain with moderate severity has been reported, yet, because the treatment pattern of manually trained clinicians varies, we were interested to determine if MET offered similar benefits (albeit, short-term) in patients with acute LPP. Subsequently, the purpose of this study was to determine the effectiveness of brief MET session on posterior innominate/ Pelvic pain when used on subjects with non-traumatic pelvic pain.
Experimental Hypothesis: Muscle Energy Technique has statistical significant relation with Pelvic pain.
Null Hypothesis: Muscle Energy Technique has no statistically significant relation with Pelvic pain.
Participants were recruited on a conveniently random sampling basis who reported to Pandit Deendayal Upadhyay National institute for the persons with Physical disabilities (Divyangjan), PDUNIPPD on OPD basis for the complaints of pain over one side of the low back/ Pelvis .
Participants who met the criteria were provided with a written information sheet outlining the requirements of participation and were provided with the opportunity to discuss all procedures with the primary researcher. Written informed consent was obtained before commencement of the study and all participants were aware that they had the opportunity to withdraw from the study prior to data analysis.

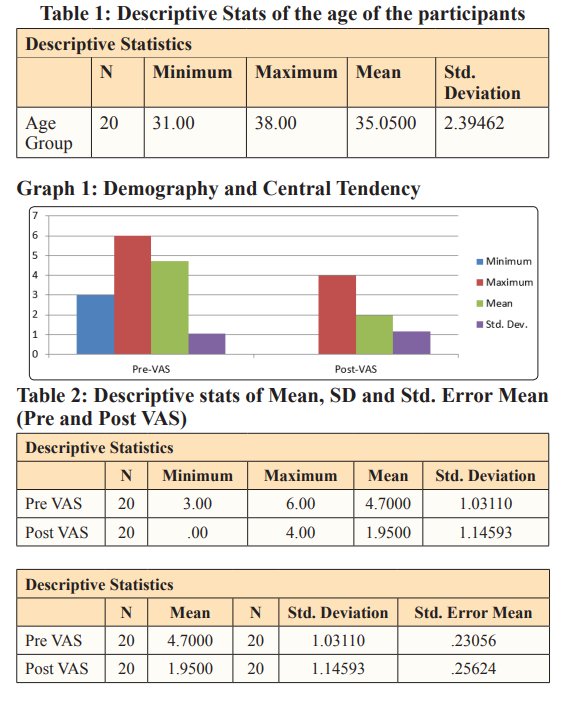
The sample consisted of 20 male participants who were allocated for comparision of the treatment effects before and after. The mean age of participants was 35.05 years (± 2.39) as shown in Table 1 and Graph 1.
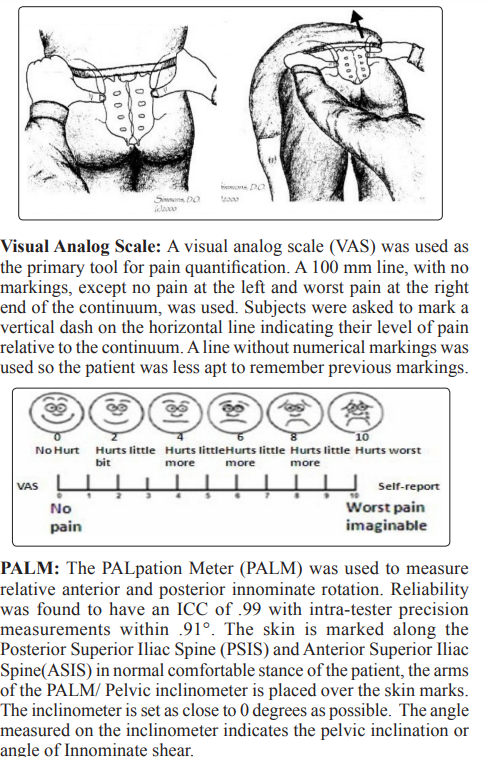
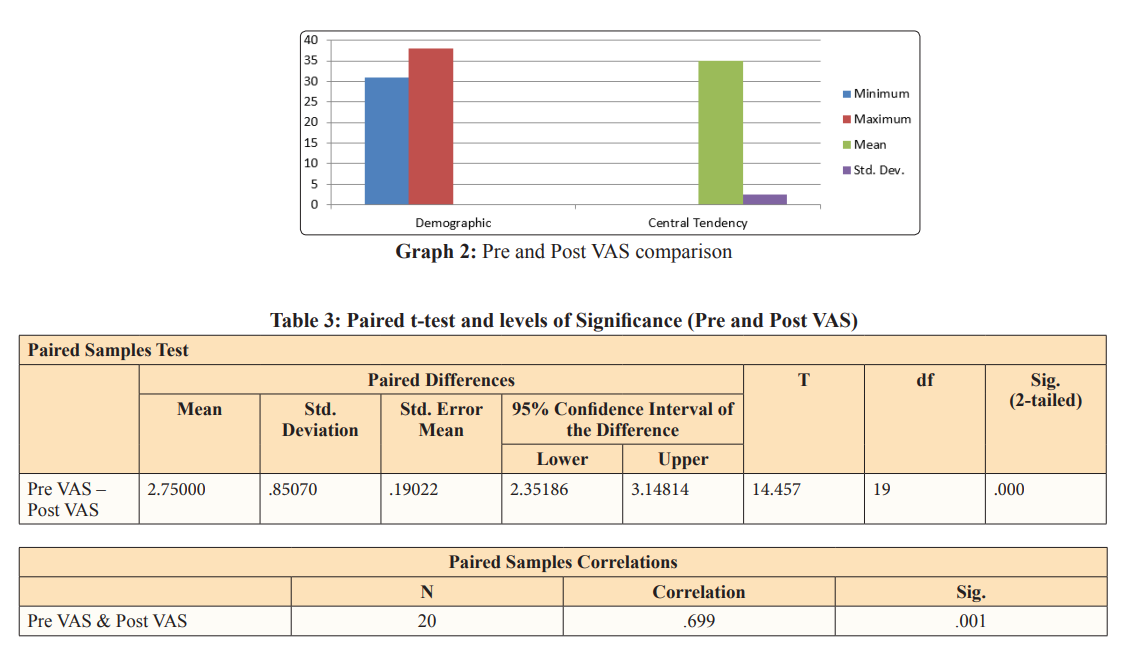
The study findings regarding statistical difference of VAS, when MET was applied for two days (once daily) and the effects were compared as pre and post treatment effects using paired t-test and the correlation on VAS, shows a decrease of mean and SD from baseline (4.7 ± 1.03) to (1.95 ± 1.14) with (t=14.457, p =.001) indicating a very high level of significance as shown in Table 2 and 3 and Graph 2.
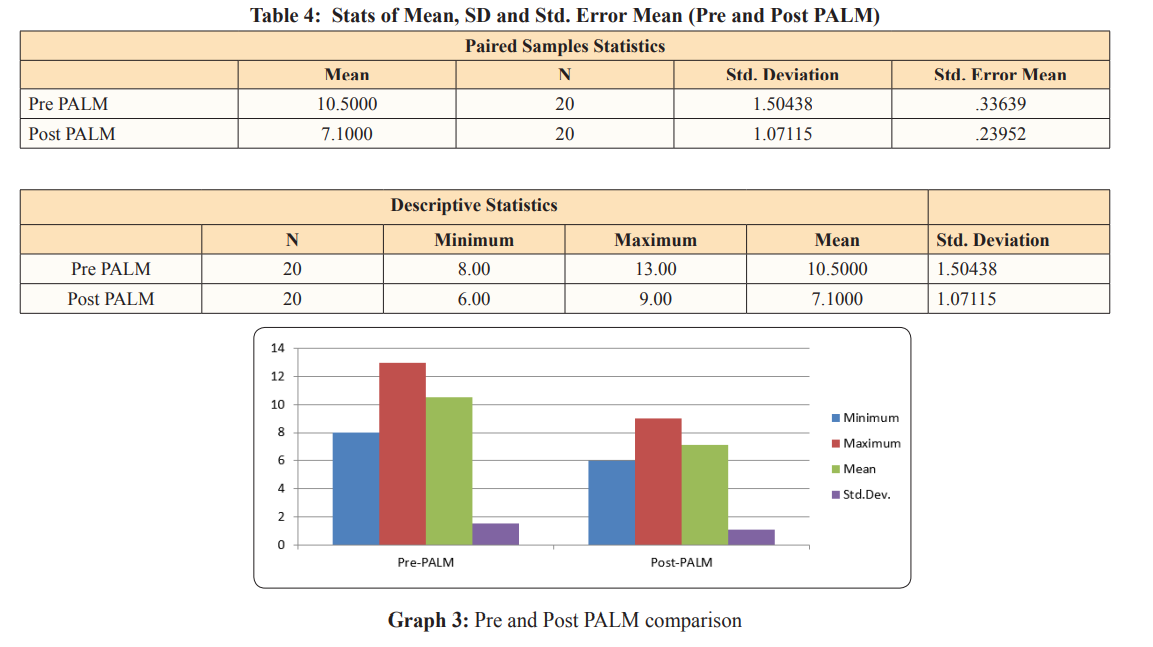
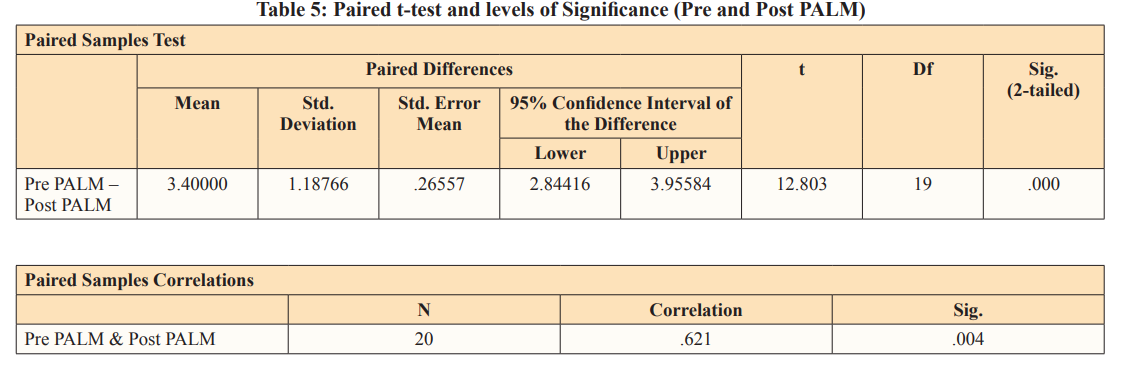
The study findings regarding statistical difference of anteriorisation of posterior shear of innominate , when MET was applied for two days (once daily) and the effects were compared as pre and post treatment effects using paired t-test and the correlation on PALM, shows a decrease of mean and SD from baseline (10.5 ± 1.50) to (7.1 ± 1.07) with (t=12.803, p =.004) indicating a high level of significance as shown in Table 4 & 5 and Graph 3.
The results showed that Muscle Energy Technique is as effective as any other manual therapy techniques (an already researched treatment tool) in the treatment of lumbo-pelvic pain or Posterior innominate. Results obtained from the different outcome measures VAS and PALPATION meter considered in this study suggests that MET was highly effective in managing pain and neutralising the pelvic rotation angles with LPP [19-26]. The treatment is evidenced, and provided as much benefit as any other manual therapy techniques for LPP. Some objective outcomes showed a trend which suggested that there might have been a great interaction if the sample size was larger.
Thus the conclusion from this research is that there was a high statistical significance between the pre and post treatment with brief MET sessions in acute LPP.
A large percentage of the adult population suffers from Low Back and Lumbo-Pelvic Pain (LPP), with a high frequency of recurrent episodes. A variety of manual therapy techniques were used in the management of low back pain to reduce pain, improve function, and reduce disability. In recent years, muscle energy techniques were increasingly used in clinics to treat LPP [1]. Muscle energy techniques can be employed to reposition a dysfunctional joint and treat the affected musculature, the patient perform a voluntary muscle contraction “in a precisely controlled direction, against a distinctly executed counter force applied by the operator” [9,13]. Studies to evaluate balance performance in unstable sitting and trunk muscle response to quick force release in 16 patients with chronic low back pain and 14 matched healthy control subjects, revealing that patients with low back pain demonstrated poorer postural control of the lumbar spine and longer trunk muscle response times than normal subjects. Correlation between these two phenomena suggests a common underlying pathology in the lumbar spine.
Low back pain characteristically involves the signs of local tenderness, tissue texture change and asymmetrical contraction of muscles. Sustained muscle contraction is often a primary source of lumbopelvic dysfunction and pain [27]. Research on 40 asymptomatic subjects to investigate the effectiveness of muscle energy technique in increasing passive knee extension and to explore the mechanism behind any observed change; a significant increase in range of motion was observed at the knee following a single application of muscle energy technique. So, muscle energy is an effective technique; meaning it engages a restrictive barrier and requires the patient’s participation for maximal effect. As the patient performs an isometric contraction, golgi activation results in direct inhibition of agonist muscles, A reflexive reciprocal inhibition occurs at the antagonistic muscles, As the patient relaxes, agonist and antagonist muscles remain inhibited allowing the joint to be moved further into the restricted range of motion patients with disorders such as low back [30-36]. The results of the present study revealed that, there was statistically significant decrease in post natal low back pain and the functional level for group (A), that was treated by MET, this was supported by Wilson et al. who stated that using MET and resistance exercises may benefit a patient greater than using neuromuscular re-education and resistance exercises to reduce low back pain and improve functional level.
Muscle Energy Technique was as effective as Manipulation in the treatment of low back pain. The treatment was not harmful, but provided as much benefit. The physiological mechanisms underlying the therapeutic effects of MET are unclear and may involve a variety of neurological and biomechanical mechanisms, including hypoalgesia, altered proprioception, motor programming and control, and changes in tissue fluid. Lasting biomechanical changes to muscle property following MET have not been demonstrated, and changes to muscle extensibility and spinal range of motion may be related to mechanisms promoting hypoalgesia and an increase in stretch tolerance [42]. Clinical studies suggest MET and related post-isometric techniques reduce pain and discomfort when applied to the spine. MET may have physiological effects, regardless of the presence or absence of dysfunction. MET has several uses that can help increase muscle strength, increase range of motion (ROM) and decrease edema, muscle energy techniques may have a greater impact on outcomes when administered over more than 1 treatment session in conjunction with therapeutic and motor-control exercise. MET combined with supervised motor control and resistance exercises may be more effective for decreasing disability and improving function in patients with acute low back pain [37-47].
In the current study, MET in the study group had an important effect on correcting pelvic tilting, reducing pain and improving function. These findings are in favour of our hypotheses where there was significant difference between pre and post treatment outcomes as the posterior innominate and pain severity were highly improved with application of two sessions of MET. It is an agreement that exercises are safe, effective and reduce the risks of future low back pain. MET was used alone without adding any other muscular exercises, to improve regaining its strength which required regaining of lumbopelvic stability and correcting its abnormality [9, 23, 26]. Many studies were done for determining the effect of MET on muscle abnormalities and R.O.M even in asymptomatic subject. There are a number of studies that supported the use of MET for pain syndromes.
In a relative study conducted by Fryer aiming to determine MET theory, practice and concept and what changes should be done to make it more effective especially in pelvic asymmetry found that it is likely to be common and unrelated to biomechanical dysfunction. An asymmetrical static pelvic finding should be considered an incidental finding unless supported by positive motion, or pain provocation tests which is concurrent with the current study as we concentrated on the most effective muscle acting to regain pelvic stability (iliopsoas and lower back muscle). Once this stability is regained, the body balance will also be regained through improving muscle condition by emphasizing on the shortened and the weak muscles which was gained through MET exercise. According to origin and insertion of those muscles, MET helps to stretch muscles and regain its strength in order to allow the pelvic bone to return to its normal condition and be at the same level although it takes time to achieve this. It is a common belief within schools of manual therapy that isometric contraction and relaxation of a long muscle under stretch enhances that stretch [16, 40].
Up to our best of knowledge, very few studies investigated the effect of MET on anterior pelvic tilt. Selkow used MET for iliopsoas and hamstring muscle in anterior pelvic patients with non-specific back pain. Although pelvic tilt was not measured and used during patients selection only, found that MET is an effective form of manual therapy used to correct lumbopelvic pain or low back pain. Also, Niemisto et al. investigated the effect of MET in combination with stabilizing exercises and physical consultation in one group, and physical consultation only for another group in chronic low back pain (CLBP) patients. The MET with stabilizing exercises group was more effective in reducing pain severity than the physical consultation group [3, 6].
Long et al studied the role of specific exercises in managing LBP through a randomized control trial using large patient numbers and the outcome measures included pain intensity and disability. Patients were divided into an exercise group and a medication group. Pain and disabilities were significantly improved in the exercise group exercise compared with the second one (medication) in every outcome [52-84].
